Abstract
Background
Studies on body composition in preterm very low birth weight (VLBW < 1500 g) survivors are inconsistent and trajectories later in life unknown. We assessed body composition and its change from young to mid-adulthood in VLBW adults.
Methods
We studied 137 VLBW adults and 158 term-born controls from two birth cohorts in Finland and Norway at mean age 36 years. Body composition was assessed by 8-polar bioelectrical impedance. We compared results with dual-energy x-ray absorptiometry measurements at 24 years.
Results
In mid-adulthood, VLBW women and men were shorter than controls. Fat percentage (mean difference in women 1.1%; 95% CI, –1.5% to 3.5%, men 0.8%; –2.0% to 3.6%) and BMI were similar. VLBW women had 2.9 (0.9 to 4.8) kg and VLBW men 5.3 (2.7 to 8.1) kg lower lean body mass than controls, mostly attributable to shorter height. Between young and mid-adulthood, both groups gained fat and lean body mass (p for interaction VLBW x age>0.3).
Conclusion
Compared with term-born controls, VLBW adults had similar body fat percentage but lower lean body mass, largely explained by their shorter height. This could contribute to lower insulin sensitivity and muscular fitness previously found in VLBW survivors and predispose to functional limitations with increasing age.
Impact
-
In mid-adulthood, individuals born preterm with very low birth weight had similar body fat percentage but lower lean body mass than those born at term. This was largely explained by their shorter height.
-
First study to report longitudinal assessments of body size and composition from young to mid-adulthood in very low birth weight adults.
-
Lower lean body mass in very low birth weight adults could contribute to lower insulin sensitivity and muscular fitness and lead to earlier functional limitations with increasing age.
Similar content being viewed by others
Introduction
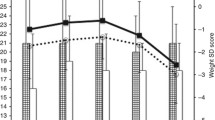
Approximately 10% of infants worldwide are born preterm (<37 completed weeks of gestation)1 and approximately 1% preterm with very low birth weight (VLBW; <1500 g).2 Adults born preterm have increased rates of non-communicable diseases such as type 2 diabetes,3,4 coronary heart disease,5 hypertension,4,6,7,8,9,10,11 osteopenia or osteoporosis12,13 and obstructive airways disease14 and higher levels of risk factors of these diseases.9,10,12,13,15,16,17 The mechanisms are unknown, nevertheless alterations in body composition are a good candidate as preterm birth profoundly alters growth of newborn tissues.6,7 This may result in altered fat and lean mass, key components of body mass18 that are related to the risk of chronic non-communicable diseases9,13,15,19 and may also contribute to reduced functional capacity later in life. Follow-up studies report shorter height and smaller head circumference in VLBW adults, indicating impaired skeletal and brain growth.9,20,21,22 Studies also suggest that adults born VLBW or extremely low birth weight (ELBW; <1000 g) have lower lean body mass9, Main background and maternal characteristics are described in Table 1. The VLBW participants were born at mean 29.4 (SD 2.4) weeks of gestation with a mean birth weight of 1169 (SD 214) grams, while control participants were born at mean 40.0 (SD 1.2) weeks of gestation weighing 3660 (SD 479) grams. Adults born with VLBW had lower educational attainment than controls (p = 0.02). The anthropometry and body composition results are described in Table 2. Compared with controls, VLBW women were 4.1 (95% CI: 1.5 to 6.4) cm and men 6.1 (95% CI: 3.6 to 8.5) cm shorter, and they had smaller head circumference. There were no group differences in fat percentage, fat mass and BMI. Among women, 12 (18.5%) VLBW, and 25 (30.9%) control participants were overweight, and 18 (27.7%) VLBW and 15 (18.5%) control participants were obese. Among men, overweight was observed in 18 (36.7%) VLBW, and 24 (38.7%) control participants, and 9 (18.4%) VLBW and 6 (9.7%) control participants were obese. Differences in overweight and obesity were not statistically significant. Adults born with VLBW had lower lean body mass. However, lean body mass adjusted for height showed no difference between the groups. The young adulthood anthropometric and body composition outcomes are described in Table 2 and Fig. 2. VLBW men and women were shorter and had smaller heads than controls. VLBW men had 1.2 (95% CI: 0.1 to 2.2) kg/m2 lower BMI than control men, whereas there was no difference in BMI among women (Table 2). In addition, VLBW men had a smaller hip and waist circumference. Both men and women in the VLBW group had lower lean body mass, but after adjustment for height, the result remained statistically significant only for VLBW women (Fig. 2, Table 2). Among men, we found a significant VLBW x age (young or mid-adulthood) interaction in waist circumference (p = 0.03). In young adulthood, VLBW men had smaller waist circumference (mean difference 3.6 cm, 95% CI: 0.7 to 6.5) compared with control men. Waist circumference increased on average by 7.0 cm in VLBW men and 1.8 cm in control men, such that the difference was no longer seen in mid-adulthood (mean difference 0.7 cm; 95% CI: -3.4 to 5.0; Table 2). Otherwise, we found no significant VLBW x age interactions (Table 2). Participants in both groups gained weight between young and mid-adulthood but differences in their body composition remained largely similar between the two ages. We conducted two sets of non-participant analyses. First, the participants who attended the mid-adulthood clinical visit were compared with those who were invited but did not attend (Supplementary table 1). In this non-participant analysis, maternal BMI was lower among non-participating controls (mean 21.6, SD 2.7) than participating controls (mean 22.8, SD 3.2, p = 0.004). Second, we carried out a non-participant analysis comparing participants who attended both the young and mid-adulthood clinical visit with those who completed DXA assessment in young adulthood but did not attend BIA assessment in the mid-adulthood (Supplementary table 2). Control men who attended DXA assessment in young adulthood but did not attend BIA in mid-adulthood had lower BMI and lean body mass adjusted for height in young adulthood compared with control men who participated at both time points. There were no other differences between non-participants and participants. In mid-adulthood women and men born preterm with very low birth weight were shorter and had smaller head circumference than their peers born at term. They also had lower lean body mass which was largely explained by their shorter height. While both the VLBW and term-born participants gained weight between young and mid-adulthood, differences in body composition between the groups remained largely similar or, if anything, became smaller. We conducted the mid-adulthood measurements in two birth cohorts with harmonized methods, which increased power and added precision. Assessors were blinded to birth status. We carried out audits before and during data collection to ensure similar measurements. As to limitations, we used two different measurement techniques to measure body composition. In young adulthood body composition was assessed by DXA which is based on the three-compartment model of body composition comprising fat, lean tissue mass and bone mineral In mid-adulthood we used 8-polar bioelectrical impedance analysis, based on two-compartment-model comprising fat and lean mass without distinguishing between bone mineral and other lean mass.37 The absolute differences in body composition between young and mid-adulthood should thus be treated with caution. However, our conclusions are mainly based on differences between VLBW and control groups, where the same measurement technique was used at the same time point. Many studies have investigated and compared these two body composition measurement techniques;37,38,39,40,41,42 DXA is accurate43 and is considered as a reference method in clinical research, but it is expensive and requires special radiological equipment.44 Bioelectrical impedance analysis is a non-invasive, simple, low-cost, safe technique45 and is a widely used method for epidemiological and clinical purposes40 and particularly useful in comparing differences between groups,41 although it does not distinguish bone from other lean tissues. Our study is the first to report longitudinal assessments of body size and composition from young to mid-adulthood. Body composition differences between VLBW adults and controls remained largely similar between these ages. Previous findings that VLBW young adults have lower lean body mass, which was largely attributable to shorter height35,46 was also observed in mid-adulthood. No change in fat percentage or BMI seemed to emerge between young and mid-adulthood. The only statistically significant interaction between group and age was for men’s waist circumference, where waist circumference increased more rapidly among VLBW than control men, such that no difference was any longer seen in mid-adulthood. Findings on fat percentage and BMI among adults born preterm vary between studies. Contrary to our findings, some studies have reported higher fat percentages among VLBW adults.10,46,47,48 A systematic review by Markopoulou et al. included nine studies estimating fat percentage measured by BIA, DXA or whole body magnetic resonance imaging (MRI) in preterm born adults compared with term-born controls. Results showed higher fat percentage both in random effect (mean difference 1.5 percentage points, p = 0.03) and fixed effect (mean difference 1.2 percentage points, p = 0.009) models.47 This difference falls within our confidence intervals and would not have been observed in the present study. However, there was moderate heterogeneity, and the difference was largely attributable to three of the nine studies. Two of the studies showing higher fat percentage included adults born at any degree of prematurity, most of whom are were late preterm, 34-36 completed weeks.28,49 Together with another study10 not included in the meta-analysis suggests that increased fat percentage is a feature of adults born late preterm but not earlier preterm. However, one of the studies included in the meta-analysis showed higher fat percentage in extremely low birth weight adults.48 This is partly consistent with another study using air displacement plethystomography showing that men but not women born at 33 weeks or less had 13% higher fat percentage, whereas men or women born late preterm showed no difference compared with controls.46 Reasons for these discrepancies are not known. Our finding of no difference in fat percentage does not exclude differences in fat distribution. Putting on weight causes adipocytes to enlarge and increases not only subcutaneous fat but also fat deposits in other vulnerable areas of the body. This ectopic fat is deposited in the intra-abdominal visceral fat depot, in muscle, in the liver and in the beta cells. On a population level, waist circumference is a commonly used indicator of abdominal fat and is a strong predictor of cardiovascular mortality.50 Studies on young adults born preterm in our source cohorts HeSVA and NTNU9,21 have reported lower waist circumference, which has not been confirmed in other studies.48,51 Our findings suggest that at least among men any difference in waist circumference in young adult age seems to level off by mid-adulthood. Visceral fat can be more accurately measured by MRI. One MRI study reported that 23 adults born at <33 weeks have higher visceral fat and hepatocellular fat, than 29 term-born controls,51 but all analyses were adjusted for BMI making the significance of the finding unclear. Another MRI study found no difference in visceral fat area between 29 extremely low birth weight adults and 13 controls. A study of 78 VLBW adults and 72 sibling-controls reported no difference in visceral fat volume or hepatocellular or muscle fat.52 Our findings related to lean body mass are largely in line with previous research. As others,9,13,23,48 we found lower lean body mass among VLBW adults. After height adjustment the results did not remain statistically significant. Lean body mass tracks across life course24 and usually starts to decline 3-8% per decade after the age of 30 years.53 A major component of lean body mass is muscle, and lower amount of muscle could contribute to reduced muscular fitness54 and insulin sensitivity19 previously shown in adults born preterm. Lower lean mass and higher fat percentage have also been associated with lower bone mineral density lower,55 although it is uncertain whether body composition predicts bone fractures over and above the risk associated with other clinical risk factors.56 As VLBW adults have lower lean body mass in their young and mid-adulthood, this normal decline in lean body mass could be expected to cause reduced functional capacity and predispose to various non-communicable diseases3,5,14 earlier than among adults born at term. However, in our study the difference in lean body mass remained similar in young and mid-adulthood, and we found no difference in the speed of decline in lean body mass between VLBW adults and controls. While we found no difference in fat percentage, other risk factors, such as higher blood pressure21,22 and reduced insulin sensitivity9,19,28 in adults born preterm may underlie the increased risk non-communicalbe diseases.9,13,15,19 In conclusion, adults born with very low birth weight entering middle age were shorter and had smaller head circumference than adults born at term. In addition, they had lower lean body mass largely attributable to their shorter height. There was no difference in body fat percentage or BMI. While the participants gained weight between young and mid-adulthood, differences in body composition remained largely similar. Lower lean body mass could contribute to lower insulin sensitivity and muscular fitness and lead to earlier functional limitations with increasing age.Results
Background characteristics of the mid-adulthood clinical visit
Body composition in mid-adulthood
Body composition in young adulthood and its development to mid-adulthood
Non-participants
Discussion
Main findings
Study strengths and limitations
Consistency with previous research
Clinical implications
Data availability
The datasets generated and/or analyzed during the current study include sensitive health data and cannot be made publicly available. Aggregated data is available from the corresponding author on reasonable request.
References
Lawn, J. E. et al. Small babies, big risks: global estimates of prevalence and mortality for vulnerable newborns to accelerate change and improve counting. Lancet 401, 1707–1719 (2023).
The 2022 March of Dimes Report Card. [cited 2023 Jun 30]; Available from: https://www.marchofdimes.org/peristats/state-summaries/united-states?top=3®=99&lev=1&stop=55&obj=3&slev=4.
Kajantie, E., Osmond, C., Barker, D. J. & Eriksson, J. G. Preterm birth-a risk factor for Type 2 Diabetes? The Helsinki Birth Cohort Study. Diabetes Care 33, 2623–2625 (2010).
Raju, T. N. K., Buist, A. S., Blaisdell, C. J., Moxey-Mims, M. & Saigal, S. Adults born preterm: a review of general health and system-specific outcomes. Acta Paediatr. 106, 1409–1437 (2017).
Crump, C. et al. Association of preterm birth with risk of ischemic heart disease in adulthood. JAMA Pediatr. 173, 736–743 (2019).
Barker, D. J., Osmond, C., Forsén, T. J., Kajantie, E. & Eriksson, J. G. Trajectories of growth among children who have coronary events as adults. N. Engl. J. Med. 353, 1802–1809 (2005).
Barker, D. J., Osmond, C., Kajantie, E. & Eriksson, J. G. Growth and chronic disease: findings in the Helsinki birth cohort. Ann. Hum. Biol. 36, 445–458 (2009).
Crump, C., Sundquist, J. & Sundquist, K. Risk of Hypertension into adulthood in persons born prematurely: a national cohort study. Eur. Heart J. 41, 1542–1550 (2020).
Hovi, P. et al. Glucose regulation in young adults with very low birth weight. N. Engl. J. Med. 356, 2053–2063 (2007).
Sipola-Leppänen, M. et al. Cardiometabolic risk factors in young adults who were born preterm. Am. J. Epidemiol. 181, 861–873 (2015).
Wells, J. C., Chomtho, S. & Fewtrell, M. S. Programming of body composition by early growth and nutrition. Proc. Nutr. Soc. 66, 423–434 (2007).
Balasuriya, C. N. D. et al. Peak bone mass and bone microarchitecture in adults born with low birth weight preterm or at term: a cohort study. J. Clin. Endocrinol. Metab. 102, 2491–2500 (2017).
Hovi, P. et al. Decreased bone mineral density in adults born with very low birth weight: a cohort study. PLoS Med. 6, e1000135 (2009).
Pulakka, A. et al. Preterm birth and asthma and copd in adulthood: a nationwide register study from two nordic countries. Eur. Respir. J. 61, 2201763 (2023).
Karvonen, R. et al. Cardiac autonomic function in adults born preterm. J. Pediatr. 208, 96–103.e104 (2019).
Tikanmäki, M. et al. Physical fitness in young adults born preterm. Pediatrics 137, e20151289 (2016).
Doyle, L. W. et al. Expiratory airflow in late adolescence and early adulthood in individuals born very preterm or with very low birthweight compared with controls born at term or with normal birthweight: a meta-analysis of individual participant data. Lancet Respir. Med. 7, 677–686 (2019).
Borga, M. et al. Advanced body composition assessment: from body mass index to body composition profiling. J. Investig. Med. 66, 1–9 (2018).
Kajantie, E. et al. Insulin sensitivity and secretory response in adults born preterm: the Helsinki study of very low birth weight adults. J. Clin. Endocrinol. Metab. 100, 244–250 (2015).
Euser, A. M., de Wit, C. C., Finken, M. J., Rijken, M. & Wit, J. M. Growth of preterm born children. Horm. Res. 70, 319–328 (2008).
Evensen, K. A. et al. Effects of preterm birth and fetal growth retardation on cardiovascular risk factors in young adulthood. Early Hum. Dev. 85, 239–245 (2009).
Hovi, P. et al. Blood pressure in young adults born at very low birth weight: adults born preterm international collaboration. Hypertension 68, 880–887 (2016).
**e, L. F. et al. The long-term impact of very preterm birth on adult bone mineral density. Bone Rep. 10, 100189 (2019).
Eriksson, J., Forsén, T., Tuomilehto, J., Osmond, C. & Barker, D. Size at birth, fat-free mass and resting metabolic rate in adult life. Horm. Metab. Res. 34, 72–76 (2002).
Ericson, A. & Källén, B. Very low birthweight boys at the age of 19. Arch. Dis. Child Fetal Neonatal Ed. 78, F171–F174 (1998).
Euser, A. M. et al. Associations between prenatal and infancy weight gain and bmi, fat mass, and fat distribution in young adulthood: a prospective cohort study in males and females born very preterm. Am. J. Clin. Nutr. 81, 480–487 (2005).
Saigal, S. et al. Growth trajectories of extremely low birth weight infants from birth to young adulthood: a longitudinal, population-based study. Pediatr. Res. 60, 751–758 (2006).
Mathai, S. et al. Increased adiposity in adults born preterm and their children. PLoS One 8, e81840 (2013).
Breukhoven, P. E., Kerkhof, G. F., Willemsen, R. H. & Hokken-Koelega, A. C. Fat mass and lipid profile in young adults born preterm. J. Clin. Endocrinol. Metab. 97, 1294–1302 (2012).
Lee, K. S. et al. Outcome of very low birth weight infants in industrialized countries: 1947–1987. Am. J. Epidemiol. 141, 1188–1193 (1995).
Official Statistics of Finland (OSF): Births and newborns 2019, Official Statistics of Finland. [cited 2023 Jun 30]; available from: https://www.stat.fi/til/synt/2019/02/synt_2019_02_2020-12-04_laa_001_en.html.
Kajantie, E. et al. Young adults with very low birth weight: leaving the parental home and sexual relationships-Helsinki Study of Very Low Birth Weight Adults. Pediatrics 122, e62–e72 (2008).
Bakketeig, L. S. et al. Pre-pregnancy risk factors of small-for-gestational age births among parous women in Scandinavia. Acta Obstet. Gynecol. Scand. 72, 273–279 (1993).
Evensen, K. A. et al. Motor skills in adolescents with low birth weight. Arch. Dis. Child Fetal Neonatal Ed. 89, F451–F455 (2004).
Balasuriya, C. N. D. et al. Metabolic outcomes in adults born preterm with very low birthweight or small for gestational age at term: a cohort study. J. Clin. Endocrinol. Metab. 103, 4437–4446 (2018).
Tolonen H. (ed). EHES Manual: Part B. Fieldwork procedures. 2nd ed. Helsinki, Finnish Institute for Health and Welfare; 2016.
Achamrah, N. et al. Comparison of body composition assessment by dxa and bia according to the body mass index: a retrospective study on 3655 measures. PLoS One 13, e0200465 (2018).
Day, K. et al. Comparison of a bioelectrical impedance device against the reference method dual energy x-ray absorptiometry and anthropometry for the evaluation of body composition in adults. Nutrients 10, 1469 (2018).
Krachler, B. et al. Bmi and an anthropometry-based estimate of fat mass percentage are both valid discriminators of cardiometabolic risk: a comparison with Dxa and bioimpedance. J. Obes. 2013, 862514 (2013).
Marra, M. et al. Assessment of body composition in health and disease using Bioelectrical Impedance Analysis (Bia) and Dual Energy X-Ray Absorptiometry (Dxa): A critical overview. Contrast Media Mol. Imaging 2019, 3548284 (2019).
Wells, J. C. & Fewtrell, M. S. Measuring body composition. Arch. Dis. Child 91, 612–617 (2006).
Wingo, B. C., Barry, V. G., Ellis, A. C. & Gower, B. A. Comparison of segmental body composition estimated by bioelectrical impedance analysis and dual-energy x-ray absorptiometry. Clin. Nutr. ESPEN 28, 141–147 (2018).
Lopes, S., Fontes, T., Tavares, R. G., Rodrigues, L. M. & Ferreira-Pêgo, C. Bioimpedance and dual-energy x-ray absorptiometry are not equivalent technologies: comparing fat mass and fat-free mass. Int. J. Environ. Res. Public Health 19, 13940 (2022).
Andreoli, A., Scalzo, G., Masala, S., Tarantino, U. & Guglielmi, G. Body composition assessment by dual-energy X-Ray Absorptiometry (Dxa). Musculoskelet. Radiol. 114, 286–300 (2009).
Lee, S. Y. & Gallagher, D. Assessment methods in human body composition. Curr. Opin. Clin. Nutr. Metab. Care 11, 566–572 (2008).
Bortolotto, C. C. et al. Prematurity and body composition at 6, 18, and 30 years of age: pelotas (brazil) 2004, 1993, and 1982 birth cohorts. BMC Public Health 21, 321 (2021).
Markopoulou, P., Papanikolaou, E., Analytis, A., Zoumakis, E. & Siahanidou, T. Preterm birth as a risk factor for metabolic syndrome and cardiovascular disease in adult life: a systematic review and meta-analysis. J. Pediatr. 210, 69–80.e65 (2019).
Morrison, K. M. et al. Cardiometabolic health in adults born premature with extremely low birth weight. Pediatrics 138, e20160515 (2016).
Kerkhof, G. F. et al. Influence of preterm birth and small birth size on serum anti-müllerian hormone levels in young adult women. Eur. J. Endocrinol. 163, 937–944 (2010).
Song, X. et al. Comparison of various surrogate obesity indicators as predictors of cardiovascular mortality in four European populations. Eur. J. Clin. Nutr. 67, 1298–1302 (2013).
Thomas, E. L. et al. Aberrant adiposity and ectopic lipid deposition characterize the adult phenotype of the preterm infant. Pediatr. Res. 70, 507–512 (2011).
Kuula, J. et al. Abdominal adipose tissue and liver fat imaging in very low birth weight adults born preterm: birth cohort with sibling-controls. Sci. Rep. 12, 9905 (2022).
Volpi, E., Nazemi, R. & Fujita, S. Muscle tissue changes with aging. Curr. Opin. Clin. Nutr. Metab. Care 7, 405–410 (2004).
Tikanmäki, M. et al. Physical fitness in young adults born preterm. Pediatrics 141, e20173993 (2018).
Deng, K. L. et al. Association between body composition and bone mineral density in children and adolescents: a systematic review and meta-analysis. Int. J. Environ. Res. Public Health 18, 12126 (2021).
Leslie, W. D. et al. Estimated lean mass and fat mass differentially affect femoral bone density and strength index but are not frax independent risk factors for fracture. J. Bone Min. Res. 29, 2511–2519 (2014).
Funding
The follow-up study was funded and supported by Academy of Finland (315690 and 355514); Alma and K.A Snellman Foundation, Oulu, Finland; Central Norway Regional Health Authority, Stjørdal, Norway; Dam Foundation, Oslo, Norway; Department of Clinical and Molecular Medicine, Norwegian University of Science and Technology (NTNU), Trondheim, Norway; European Union’s Horizon 2020 Research and Innovation Program: Research on European Children and Adults born Preterm (RECAP Preterm), Trondheim, Norway and Helsinki, Finland (733280); Evald and Hilda Nissi Foundation, Espoo, Finland; Eye Foundation, Helsinki, Finland; Eye and Tissue Bank Foundation, Helsinki, Finland; Faculty of Medicine and Health Sciences, NTNU, Trondheim, Norway; Finnish Diabetes Research Foundation, Tampere, Finland; Finnish Foundation for Cardiovascular Research, Helsinki, Finland; Finnish Medical Foundation, Helsinki, Finland; Foundation for Pediatric Research, Helsinki, Finland; the Joint Research Committee of St. Olavs Hospital HF and Faculty of Medicine and Health Sciences, NTNU, Trondheim, Norway; Mary and Georg C. Ehrnrooth Foundation Helsinki, Finland; Novo Nordisk Foundation, Hellerup, Denmark; Signe and Ane Gyllenberg Foundation, Helsinki, Finland; Sigrid Juselius Foundation, Helsinki, Finland; University of Oulu Graduate School, University of Oulu, Oulu, Finland. Open Access funding provided by Finnish Institute for Health and Welfare.
Author information
Authors and Affiliations
Contributions
L.J. provided substantial contribution to the analysis and interpretation of data and drafted the initial manuscript. M.K. and A.P.M.J. provided substantial contribution to acquisition of data, revised the manuscript critically for important intellectual content and approved the final version to be published. K.A.D.A., S.D.B., C.B., A.K.S., U.S., M.S.I., S.A. and P.H. revised the manuscript critically for important intellectual content and approved the final version to be published. K.A.I.E. and E.K. provided substantial contribution to conception and design, acquisiton of data, analysis and interpretation of data and revised the manuscript critically for important intellectual content and approved the final version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Informed consent
Written informed consent was required and received from all participants who attended the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jussinniemi, L., Kulmala, M.K., Aakvik, K.A.D. et al. Body composition in adults born preterm with very low birth weight. Pediatr Res 95, 1316–1324 (2024). https://doi.org/10.1038/s41390-023-02896-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02896-5
- Springer Nature America, Inc.
This article is cited by
-
Body composition of very preterm infants in mid-adulthood
Pediatric Research (2023)