Abstract
Objective
Our hypothesis was that the activity of placental nutrient-sensing pathways is associated with adiposity and metabolic health in childhood.
Research design and methods
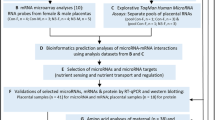
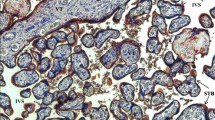
Using placental villus samples from healthy mothers from the Healthy Start Study, we measured the abundance and phosphorylation of key intermediates in the mTOR, insulin, AMPK, and ER stress signaling pathways. Using multivariate multiple regression models, we tested the association between placental proteins and offspring adiposity (%fat mass) at birth (n = 109), 4–6 months (n = 104), and 4–6 years old (n = 64), adjusted for offspring sex and age.
Results
Placental mTORC1 phosphorylation was positively associated with adiposity at birth (R2 = 0.13, P = 0.009) and 4–6 years (R2 = 0.15, P = 0.046). The mTORC2 target PKCα was positively associated with systolic blood pressure at 4–6 years (β = 2.90, P = 0.005). AMPK phosphorylation was positively associated with adiposity at birth (β = 2.32, P = 0.023), but the ratio of phosphorylated to total AMPK was negatively associated with skinfold thickness (β = −2.37, P = 0.022) and body weight (β = −2.92, P = 0.005) at 4–6 years.
Conclusions
This is the first report of associations between key placental protein activity measures and longitudinal child outcomes at various life stages. Our data indicate that AMPK and mTOR signaling are linked to cardiometabolic measures at birth and 4–6 years, providing novel insight into potential mechanisms underpinning how metabolic signaling in the placenta is associated with future risk of cardiovascular disease.



Similar content being viewed by others
References
Skinner, AC, Ravanbakht, SN, Skelton, JA, Perrin, EM, & Armstrong, SC (2018). Prevalence of obesity and severe obesity in US children, 1999–2016. Pediatrics, e20173459.
Barker DJ. The developmental origins of insulin resistance. Hormone Res Paediatrics. 2005;64:2–7.
Gluckman PD, Hanson MA. The developmental origins of the metabolic syndrome. Trends Endocrinol Metab. 2004;15:183–7.
Gluckman PD, Hanson MA, Cooper C. In utero and early-life conditions and adult health and disease. N Engl J Med. 2008;359:1524.
Burton GJ, Fowden AL, Thornburg KL. Placental origins of chronic disease. Physiol Rev. 2016;96:1509–65.
Barker DJ, Gelow J, Thornburg K, Osmond C, Kajantie E, Eriksson JG. The early origins of chronic heart failure: impaired placental growth and initiation of insulin resistance in childhood. Eur J Heart Failure. 2010;12:819–25.
Barker DJ, Thornburg KL, Osmond C, Kajantie E, Eriksson JG. The surface area of the placenta and hypertension in the offspring in later life. Int J Dev Biol. 2010;54:525.
Barker DJ, Larsen G, Osmond C, Thornburg KL, Kajantie E, Eriksson JG. The placental origins of sudden cardiac death. Int J Epidemiol. 2012;41:1394–9.
Jansson T, Powell TL. Role of placental nutrient sensing in developmental programming. Clin Obstet Gynecol. 2013;56:591.
Chen L, Guilmette J, Luo Z-C, Cloutier A, Wang W-J, Yang M-N, et al. Placental 11β-HSD2 and cardiometabolic health indicators in infancy. Diabetes Care. 2019;42:964–71.
Laviola L, Perrini S, Belsanti G, Natalicchio A, Montrone C, Leonardini A, et al. Intrauterine growth restriction in humans is associated with abnormalities in placental insulin-like growth factor signaling. Endocrinology. 2005;146:1498–505.
Yung H-w, Calabrese S, Hynx D, Hemmings BA, Cetin I, Charnock-Jones DS, et al. Evidence of placental translation inhibition and endoplasmic reticulum stress in the etiology of human intrauterine growth restriction. Am J Pathol. 2008;173:451–62.
Gaccioli F, White V, Capobianco E, Powell TL, Jawerbaum A, Jansson T. Maternal overweight induced by a diet with high content of saturated fat activates placental mTOR and eIF2alpha signaling and increases fetal growth in rats. Biol Reprod. 2013;89:91–11. 96
Jansson N, Rosario FJ, Gaccioli F, Lager S, Jones HN, Roos S, et al. Activation of placental mTOR signaling and amino acid transporters in obese women giving birth to large babies. J Clin Endocrinol Metabol. 2013;98:105–13.
Kim J, Guan K-L. mTOR as a central hub of nutrient signalling and cell growth. Nat Cell Biol. 2019;21:63.
Rosario FJ, Kanai Y, Powell TL, Jansson T. Mammalian target of rapamycin signalling modulates amino acid uptake by regulating transporter cell surface abundance in primary human trophoblast cells. J Physiol. 2013;591:609–25.
Rosario FJ, Powell TL, Jansson T. Mechanistic target of rapamycin (mTOR) regulates trophoblast folate uptake by modulating the cell surface expression of FR-α and the RFC. Sci Reports. 2016;6:31705.
Rosario FJ, Gupta MB, Myatt L, Powell TL, Glenn JP, Cox L, et al. Mechanistic target of rapamycin complex 1 promotes the expression of genes encoding electron transport chain proteins and stimulates oxidative phosphorylation in primary human trophoblast cells by regulating mitochondrial biogenesis. Sci. Reports. 2019;9:246.
Kola, B, Grossman, AB, & Korbonits, M. The role of AMP-activated protein kinase in obesity. In: Obesity and metabolism, Vol. 36, Karger Publishers; 2008. pp. 198–211.
Sauder KA, Stamatoiu AV, Leshchinskaya E, Ringham BM, Glueck DH, Dabelea D. Cord blood vitamin D levels and early childhood blood pressure: the healthy start study. J Am Heart Assoc. 2019;8:e011485.
Starling AP, Brinton JT, Glueck DH, Shapiro AL, Harrod CS, Lynch AM, et al. Associations of maternal BMI and gestational weight gain with neonatal adiposity in the Healthy Start study. Am J Clin Nutrition. 2014;101:302–9.
Barker DJ, Godfrey K, Gluckman PD, Harding JE, Owens JA, Robinson JS. Fetal nutrition and cardiovascular disease in adult life. The Lancet. 1993;341:938–41.
Boney CM, Verma A, Tucker R, Vohr BR. Metabolic syndrome in childhood: association with birth weight, maternal obesity, and gestational diabetes mellitus. Pediatrics. 2005;115:e290–e296.
Roberts VH, Smith J, McLea SA, Heizer AB, Richardson JL, Myatt L. Effect of increasing maternal body mass index on oxidative and nitrative stress in the human placenta. Placenta. 2009;30:169–75.
Saben J, Lindsey F, Zhong Y, Thakali K, Badger T, Andres A, et al. Maternal obesity is associated with a lipotoxic placental environment. Placenta. 2014;35:171–7.
Gupta, M, & Jansson, T. Novel roles of mTOR signaling in regulating fetal growth. Biol Reprod. 2018;100:872–84.
Chen, Y-Y, Rosario, FJ, Shehab, MA, Powell, TL, Gupta, MB, & Jansson, T. Increased ubiquitination and reduced plasma membrane trafficking of placental amino acid transporter SNAT-2 in human IUGR. Clin Sci. 2015;129:1131–41.
Tee, AR, & Blenis, J. mTOR, translational control and human disease. Paper presented at the Seminars in cell & developmental biology. 2005.
Thoreen CC, Chantranupong L, Keys HR, Wang T, Gray NS, Sabatini DM. A unifying model for mTORC1-mediated regulation of mRNA translation. Nature. 2012;485:109.
Um SH, D’Alessio D, Thomas G. Nutrient overload, insulin resistance, and ribosomal protein S6 kinase 1, S6K1. Cell Metab. 2006;3:393–402.
Rosario FJ, Jansson N, Kanai Y, Prasad PD, Powell TL, Jansson T. Maternal protein restriction in the rat inhibits placental insulin, mTOR, and STAT3 signaling and down-regulates placental amino acid transporters. Endocrinology. 2011;152:1119–29.
Kavitha JV, Rosario FJ, Nijland MJ, McDonald TJ, Wu G, Kanai Y, et al. Down-regulation of placental mTOR, insulin/IGF-I signaling, and nutrient transporters in response to maternal nutrient restriction in the baboon. FASEB J. 2014;28:1294–305.
Zhang BB, Zhou G, Li C. AMPK: an emerging drug target for diabetes and the metabolic syndrome. Cell Metab. 2009;9:407–16.
Ó’Grada, C. Fetal origins, childhood development, and famine: a bibliography and literature review. SSRN Elect J. 2012;1–76. https://doi.org/10.2139/ssrn.1980709.
Ma Y, Zhu MJ, Uthlaut AB, Nijland MJ, Nathanielsz PW, Hess BW, et al. Upregulation of growth signaling and nutrient transporters in cotyledons of early to mid-gestational nutrient restricted ewes. Placenta. 2011;32:255–63.
Martino J, Sebert S, Segura M, Garcia-Valdes L, Florido J, Padilla M, et al. Maternal body weight and gestational diabetes differentially influence placental and pregnancy outcomes. J Clin Endocrinol. 2016;101:59–68.
Boyle K, Patinkin Z, Shapiro A, Bader C, Vanderlinden L, Kechris K, et al. Maternal obesity alters fatty acid oxidation, AMPK activity, and associated DNA methylation in mesenchymal stem cells from human infants. Mol Metab. 2017;6:1503–16.
Konopatskaya O, Poole AW. Protein kinase Cα: disease regulator and therapeutic target. Trends Pharmacol Sci. 2010;31:8–14.
Drägert K, Bhattacharya I, Pellegrini G, Seebeck P, Azzi A, Brown SA, et al. Deletion of rictor in brain and fat alters peripheral clock gene expression and increases blood pressure. Hypertension. 2015;66:332–9.
Tang H, Wu K, Wang J, Vinjamuri S, Gu Y, Song S, et al. Pathogenic role of mTORC1 and mTORC2 in pulmonary hypertension. JACC Basic Transl Sci. 2018;3:744–62.
Acknowledgements
The authors thank M. Martinez (the Healthy Start Study project coordinator, Colorado School of Public Health, University of Colorado) and the Healthy Start team for their hard work and dedication to this study.
Funding
The Healthy Start BabyBUMP Project is supported by grants from the American Heart Association (predoctoral fellowship 14PRE18230008) and by the parent Healthy Start Study (to DD). The Healthy Start Study was supported by the National Institute of Health (R01 DK076648 to DD) and the Colorado Clinical and Translational Sciences Institute (UL1 TR001082) for maternal visits and collection of birth measures. The funders had no influence on the results of the study.
Author information
Authors and Affiliations
Contributions
TJ contributed to the conception of the article. MRK, KE, KEB, DD, JEF, and TJ contributed to data collection. MRK, KE, and KK contributed to the statistical analysis. TJ, MRK, IVY, DD, and KEB contributed to the interpretation of the results. MRK, KEB, and TJ drafted the manuscript. All authors approved the final version of the manuscript. TJ is the guarantor of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Keleher, M.R., Erickson, K., Kechris, K. et al. Associations between the activity of placental nutrient-sensing pathways and neonatal and postnatal metabolic health: the ECHO Healthy Start cohort. Int J Obes 44, 2203–2212 (2020). https://doi.org/10.1038/s41366-020-0574-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-020-0574-y
- Springer Nature Limited