Abstract
Purpose
Evaluating the learning curve (LC) in surgical training is complex, as multiple factors influence skills acquisition. Among these, the impact of new technology might be the most critical. Few studies have assessed how new technology can influence LC, especially in novices with no surgical experience.
Methods
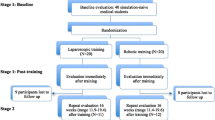
A prospective observational or interventional study was performed at an international minimally invasive training center from August 22nd to 26th 2022. Two different groups of novices (medical vs. non-medical) were compared to assess how medical background could have an impact on performing laparoscopic and robotic tasks. Both groups were evaluated by performing a standardized set of validated simulation tasks: the Laparoscopic Assessment Skills Training Testing method (LASTT) and the advanced peg transfer task on four different robotic platforms (DaVinci X and Si, Versius CMR and Hugo™ RAS System). Performance was graded using the validated Global Operative Assessment of Laparoscopic Skills (GOALS) Score System for laparoscopic and the Global Evaluative Assessment of Robotic Skills (GEARS) Score System. The main outcome measure was the ability to complete the exercises in the required times across novice groups.
Results
Thirteen medical and fourteen non-medical novices participated. The medical group performed significantly better in all LASTT exercises, reaching higher GOALS in-depth perception (p = 0.008), bimanual dexterity (p = 0.008), and efficiency (p = 0.021). There were no significant differences across groups for time to task completion, depth perception, bimanual dexterity, autonomy, or robotic control on any robotic platform.
Conclusion
While medical students were more skilled in laparoscopy, no differences were found between groups on robotic platforms. Robotics democratized skills acquisition with a more predictable LC independent of medical experience.

Similar content being viewed by others
References
De Witte B, Di Rienzo F, Martin X, Haixia Y, Collet C, Hoyek N. Implementing cognitive training into a surgical skill course: a pilot study on laparoscopic suturing and knot tying. Surg Innov. 2018;25:625–35. https://doi.org/10.1177/1553350618800148.
Vergis A, Hardy K. Cognitive and technical skill assessment in surgical education: a changing Horizon. Indian J Surg. 2017;79:153–7. https://doi.org/10.1007/s12262-017-1603-5.
Cobianchi L, Dal Mas F, Verde JM, et al. Why non-technical skills matter in surgery. New paradigms for surgical leaders. Discov Health Systems. 2022;1(1):2. https://doi.org/10.1007/s44250-022-00002-w.
Reitano E, de’Angelis N, Schembari E, et al. Learning curve for laparoscopic cholecystectomy has not been defined: a systematic review. ANZ J Surg. 2021;91(9):554–60. https://doi.org/10.1111/ans.17021.
Sheetz KH, Norton EC, Birkmeyer JD, Dimick JB. Provider experience and the comparative safety of laparoscopic and open colectomy. Health Serv Res. 2017;52(1):56. https://doi.org/10.1111/1475-6773.12482.
Fung G, Sha M, Kunduzi B, Froghi F, Rehman S, Froghi S. Learning curves in minimally invasive pancreatic surgery : a systematic review. Langenbeck’s Arch Surg. 2022. https://doi.org/10.1007/s00423-022-02470-3.
de’Angelis N, Lizzi V, Azoulay D, Brunetti F. Robotic versus laparoscopic right colectomy for colon cancer: analysis of the initial simultaneous learning curve of a surgical fellow. J Laparoendosc Adv Surg Tech. 2016;26:882–92. https://doi.org/10.1089/lap.2016.0321.
Siddaiah-Subramanya M, Tiang KW, Nyandowe M. A new era of minimally invasive surgery: progress and development of major technical innovations in general surgery over the last decade. Surg J. 2017;3:163–6. https://doi.org/10.1055/s-0037-1608651.
Leroy J, Diana M, Perretta S, Wall J, De Ruijter V, Marescaux J. Original technique to close the transrectal viscerotomy access in a NOTES transrectal and transgastric segmental colectomy. Surg Innov. 2011;18:193–200. https://doi.org/10.1177/1553350611411490.
Reitano E, Famularo S, Dallemagne B, et al. Educational scoring system in laparoscopic cholecystectomy : is it the right time to standardize ? Medicina. 2023;59(3):446. https://doi.org/10.3390/medicina59030446.
Brown C, Abdelrahman T, Patel N, Thomas C, Pollitt MJ, Lewis WG. Operative learning curve trajectory in a cohort of surgical trainees. Br J Surg. 2017;104:1405–11. https://doi.org/10.1002/bjs.10584.
Hasan A, Pozzi M, Hamilton JR. New surgical procedures: can we minimise the learning curve? BMJ. 2000;320:171–3. https://doi.org/10.1136/bmj.320.7228.171.
DiMeo AJ, Afamefuna CJ, Ward SJ, et al. Biomedical engineering professional skills development: The RADxSM tech impact on graduates and faculty. IEEE Open J Eng Med Biol. 2021;2:163–9. https://doi.org/10.1109/OJEMB.2021.3070831.
Rambukwella M, Balamurugan A, Klapholz H, Beninger P. The application of engineering principles and practices to medical education: preparing the next generation of physicians. Med Sci Educ. 2021;31:897–904. https://doi.org/10.1007/s40670-021-01217-x.
de Ruijter V, Halvax P, Dallemagne B, Swanström L, Marescaux J, Perretta S. The business engineering surgical technologies (BEST) teaching method: incubating talents for surgical innovation. Surg Endosc. 2015;29:48–54. https://doi.org/10.1007/s00464-014-3652-1.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–9. https://doi.org/10.1136/bmj.39335.541782.
Vassiliou MC, Feldman LS, Andrew CG, et al. A global assessment tool for evaluation of intraoperative laparoscopic skills. Am J Surg. 2005;190:107–13. https://doi.org/10.1016/j.amjsurg.2005.04.004.
Goh AC, Goldfarb DW, Sander JC, Miles BJ, Dunkin BJ. Global evaluative assessment of robotic skills: validation of a clinical assessment tool to measure robotic surgical skills. J Urol. 2012;187:247–52. https://doi.org/10.1016/j.juro.2011.09.032.
Davila DG, Helm MC, Frelich MJ, Gould JC, Goldblatt MI. Robotic skills can be aided by laparoscopic training. Surg Endosc. 2017;32:2683–8. https://doi.org/10.1007/s00464-017-5963-5.
Panait L, Shetty S, Shewokis PA, Sanchez JA. Do laparoscopic skills transfer to robotic surgery? J Surg. 2014;187:53–8. https://doi.org/10.1016/j.jss.2013.10.014.
Hassan SO, Dudhia J, Syed LH, et al. Conventional laparoscopic vs robotic training: which is better for naive users? A randomized prospective crossover study. J Surg Educ. 2015;72(4):592–9. https://doi.org/10.1016/j.jsurg.2014.12.008.
Kanitra JJ, Khogali-Jakary N, Gambhir SB, et al. Transference of skills in robotic vs. laparoscopic simulation: a randomized controlled trial. BMC Surg. 2021;21:379. https://doi.org/10.1186/s12893-021-01385-y.
Bhayani SB, Andriole GL. Three-dimensional (3D) vision: does it improve laparoscopic skills? An assessment of a 3D head-mounted visualization system. Rev Urol. 2005;7:211–4.
Torricelli FC, Barbosa JA, Marchini GS. Impact of laparoscopic surgery training laboratory on surgeon’s performance. World J Gastrointest Surg. 2016;8:735–43. https://doi.org/10.4240/wjgs.v8.i11.735.
Gupta A, Lawendy B, Goldenberg MG, Grober E, Lee JY, Perlis N. Can video games enhance surgical skills acquisition for medical students? A systematic review. Surg. 2021;169:821–9. https://doi.org/10.1016/j.surg.2020.11.034.
Sammut M, Sammut M, Andrejevic P. The benefits of being a video gamer in laparoscopic surgery. Int J Surg. 2017;45:42–6. https://doi.org/10.1016/j.ijsu.2017.07.07.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors have no conflict of interest to disclose.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Reitano, E., Riva, P., Keller, D.S. et al. A prospective observational study on minimally invasive surgery skill acquisition across novice levels. Global Surg Educ 2, 84 (2023). https://doi.org/10.1007/s44186-023-00159-9
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s44186-023-00159-9