Abstract
Background
The purpose of this study was to evaluate the flexion-gap of the native knees in the normal population and to assess any gender-specific variations in the flexion gap of the knees.
Methods
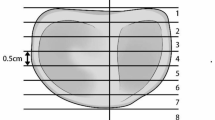
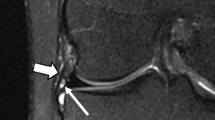
A total of 50 normal asymptomatic volunteers with normal knee radiographs were selected for MRI of the knee. The left knee was scanned in an open MRI using a T1-weighted sequence. Imaging was performed in neutral, passive varus and valgus stress at 90° of knee flexion by placing custom-made blocks on a special board consecutively below the distal part of the leg.
Results
The study population consisted of 26 males and 24 females with a mean age of 25.77 years. Under varus stress, the mean lateral flexion gap increased to 9.28 ± 1.53 mm and under valgus stress, the mean medial flexion gap increased to 2.75 ± 1.22 mm from neutral. The increase in the flexion gap on the lateral side was 5.28 ± 1.79 mm, which was significantly higher compared to that on the medial side. In gender-specific analysis, the mean lateral flexion gap was 10.21 mm in females and 8.46 mm in males under varus stress.
Conclusion
The findings of the study indicate that the lateral soft tissues are more lax compared to the medial soft tissue structures and this laxity is higher in females as compared to males. The study provides evidence of the existing physiological variations of these soft tissue structures resulting in a trapezoidal flexion gap in the native knees rather than the recommended rectangular gap.






Similar content being viewed by others
Data availability
The manuscript data can be made available on request.
References
Willcox, N. M. J., Clarke, J. V., Smith, B. R. K., Deakin, A. H., & Deep, K. (2012). A comparison of radiological and computer navigation measurements of lower limb coronal alignment before and after total knee replacement. The Journal of Bone and Joint Surgery Series B, 94, 1234–1240. https://doi.org/10.1302/0301-620X.94B9.28250
Scott, W. N. (2017). Insall & Scott surgery of the knee. (6th ed.). Churchill Livingstone/Elsevier.
Scuderi, G., & Insall, J. (1989). The posterior stabilized knee prosthesis. Orthopedic Clinics of North America, 20, 71–78
Beverland D. E. (2009). Soft-tissue balance in total knee arthroplasty. In European instructional lectures. Springer Berlin Heidelberg. pp. 213–8.
Tokuhara, Y., Kadoya, Y., Kanekasu, K., Kondo, M., Kobayashi, A., & Takaoka, K. (2006). Evaluation of the flexion gap by axial radiography of the distal femur. The Journal of Bone and Joint Surgery Series B, 88, 1327–1330. https://doi.org/10.1302/0301-620X.88B1017793
Tokuhara, Y., Kadoya, Y., Nakagawa, S., Kobayashi, A., Takaoka, K., & Surgeon, O. (2004). The flexion gap in normal knees AN MRI STUDY. The Journal of Bone and Joint Surgery [British Volume], 86, 1133–1139. https://doi.org/10.1302/0301-620X.86B8
Matsuda, S., & Ito, H. (2015). Ligament balancing in total knee arthroplasty—Medial stabilizing technique. Asia-Pacific Journal of Sports Medicine, Arthroscopy, Rehabilitation and Technology, 2, 108–113. https://doi.org/10.1016/j.asmart.2015.07.002
Deep, K. (2014). Collateral ligament laxity in knees: what is normal? Clinical Orthopaedics and Related Research, 472, 3426–3431. https://doi.org/10.1007/s11999-014-3865-6
Okazaki, K., Miura, H., Matsuda, S., Takeuchi, N., Mawatari, T., Hashizume, M., et al. (2006). Asymmetry of mediolateral laxity of the normal knee. Journal of Orthopaedic Science, 11, 264–266. https://doi.org/10.1007/s00776-006-1009-x
Rajendran, K. (1985). Mechanism of locking at the knee joint. Journal of Anatomy, 143, 189–194
Thomine, J. M., Boudjemaa, A., Gibon, Y., & Biga, N. (1981). Varizing axial distances in osteoarthrosis of the knee (author’s transl). Revue de Chirurgie Orthopedique et Reparatrice de l’Appareil Moteur, 67, 319–327
Yoo, J. C., Ahn, J. H., Sung, K. S., Wang, J. H., Lee, S. H., Bae, S. W., et al. (2006). Measurement and comparison of the difference in normal medial and lateral knee joint opening. Knee Surgery, Sport Traumatology, Arthroscopy, 14, 1238–1244. https://doi.org/10.1007/s00167-006-0095-9
Ahlberg, A., Moussa, M., & Al-Nahdi, M. (1988). On geographical variations in the normal range of joint motion. Clinical Orthopaedics and Related Research. https://doi.org/10.1097/00003086-198809000-00040
Mulholland, S. J., & Wyss, U. P. (2001). Activities of daily living in non-Western cultures: Range of motion requirements for hip and knee joint implants. International Journal of Rehabilitation Research, 24, 191–198. https://doi.org/10.1097/00004356-200109000-00004
Dennis, D. A., Komistek, R. D., Walker, S. A., Cheal, E. J., & Stiehl, J. B. (2001). Femoral condylar lift-off in vivo in total knee arthroplasty. The Journal of Bone and Joint Surgery. British Volume, 83, 33
Dennis, D. A., Komistek, R. D., Mahfouz, M. R., Haas, B. D., & Stiehl, J. B. (2003). Multicenter determination of in vivo kinematics after total knee arthroplasty. Clinical Orthopaedics & Related Research, 416, 37–57. https://doi.org/10.1097/01.blo.0000092986.12414.b5
Dennis, D. A., Komistek, R. D., Stiehl, J. B., Walker, S. A., & Dennis, K. N. (1998). Range of motion after total knee arthroplasty: The effect of implant design and weight-bearing conditions. Journal of Arthroplasty, 13, 748–752. https://doi.org/10.1016/S0883-5403(98)90025-0
McEwen, P., Balendra, G., & Doma, K. (2019). Medial and lateral gap laxity differential in computer-assisted kinematic total knee arthroplasty. The Bone & Joint Journal, 101, 331–339. https://doi.org/10.1302/0301-620X.101B3.BJJ-2018-0544.R1
Azukizawa, M., Kuriyama, S., Nakamura, S., Nishitani, K., Lyman, S., Morita, Y., et al. (2018). Intraoperative medial joint laxity in flexion decreases patient satisfaction after total knee arthroplasty. Archives of Orthopaedic and Trauma Surgery, 138, 1143–1150. https://doi.org/10.1007/s00402-018-2965-2
Hungerford, D. S., & Krackow, K. A. (1985). Total joint arthroplasty of the knee. Clinical Orthopaedics and Related Research. https://doi.org/10.1097/00003086-198501000-00004
Massin, P. (2017). How does total knee replacement technique influence polyethylene wear? Orthopaedics & Traumatology, Surgery & Research, 103, S21–S27. https://doi.org/10.1016/j.otsr.2016.06.024
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
SKP: manuscript preparation, manuscript editing; MS: data collection, subject allocation, manuscript preparation; AAS: supervision, manuscript editing, statistical analysis; PT: manuscript editing, statistical analysis, data collection; RKG: manuscript editing, data collection; RA: data collection and analysis. JC: manuscript editing, statistical analysis. AS: data collection, manuscript editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Ethical approval
This article does not contain any studies with human or animal subjects performed by any of the authors.
Informed consent
For this type of study informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pathak, S.K., Sethi, M., Salunke, A.A. et al. Is Flexion Gap Rectangular in Native Indian Knees? Results of an MRI Study. JOIO 55, 1127–1134 (2021). https://doi.org/10.1007/s43465-021-00418-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-021-00418-1