Abstract
Purpose
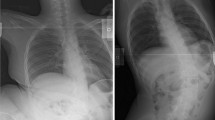
This study aimed to determine whether Cobb and pelvic obliquity corrections can be predicted using supine traction radiographs in patients with cerebral palsy (CP) who underwent posterior spinal fusion (PSF) from T2/3 to L5.
Methods
From January 2010 to January 2020, 167 non-ambulatory patients with CP scoliosis underwent PSF using pedicle screws in two quaternary centers with a minimum of 2 years follow-up (FU). Radiological measurements and chart reviews were performed.
Results
A total of 106 patients aged 15.6 ± 0.4 years were included. All patients had significant correction of the Cobb angle (MC), pelvic obliquity (PO), thoracic kyphosis (TK), and lumbar lordosis (LL) without loss of correction at the last FU (LFU). Curve flexibility was significantly correlated with Cobb correction (δMC) immediately postoperatively (p < 0.0001, r = 0.8950), followed by the amount of correction in pelvic obliquity under traction (δPOT) (p = 0.0252, r = 0.2174). For correction in PO (δPO), the most significant variable was δPOT (p < 0.0001, r = 0.7553), followed by curve flexibility (p = 0.0059, r = 0.26) and the amount of correction in Cobb under traction (p = 0.0252, r = 0.2174).
Conclusions
Cobb and PO corrections can be predicted using supine traction films for non-ambulatory CP patients treated with PSF from T2/3 to L5. The variables evaluated were interconnected, reinforcing preoperative planning for these patients. Comparative large-scale studies on patient-related clinical outcomes are required to determine whether this predicted correction is associated with improved surgical outcomes and reduced complication rates.
Level of evidence
IV


Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the corresponding author.
References
Hagglund G et al (2018) Incidence of scoliosis in cerebral palsy. Acta Orthop 89(4):443–447
Ilharreborde B et al (2020) Spinal sagittal alignment and head control in patients with cerebral palsy. J Child Orthop 14(1):17–23
Loughenbury PR, Tsirikos AI (2022) Current concepts in the treatment of neuromuscular scoliosis: clinical assessment, treatment options, and surgical outcomes. Bone Jt Open 3(1):85–92
Kim HS, Kwon JW, Park KB (2022) Clinical issues in indication, correction, and outcomes of the surgery for neuromuscular scoliosis narrative review in pedicle screw era. Neurospine 19:177–187
Chaudry Z, Anderson JT (2017) Curve flexibility in cerebral palsy-related neuromuscular scoliosis: does the intraoperative prone radiograph reveal more flexibility than preoperative radiographs? Scoliosis Spinal Disord 12:15
Miller DJ et al (2020) Improving health-related quality of life for patients with nonambulatory cerebral palsy: who stands to gain from scoliosis surgery? J Pediatr Orthop 40(3):e186–e192
Nordon DG et al (2017) Correlation between the degree of correction of neuromuscular scoliosis and patient quality of life. Clinics (Sao Paulo) 72(2):71–80
Nielsen E et al (2019) Don’t you wish you had fused to the pelvis the first time: a comparison of reoperation rate and correction of pelvic obliquity. Spine 44(8):E465–E469
Buckland AJ et al (2021) Residual lumbar hyperlordosis is associated with worsened hip status 5 years after scoliosis correction in non-ambulant patients with cerebral palsy. Spine Deform 9(4):1125–1136
Howard R et al (2022) Definitive fusion for scoliosis in late juvenile cerebral palsy patients is durable at 5 years postoperatively. Spine Deform 10:1423–1428
Beckmann K et al (2016) Surgical correction of scoliosis in patients with severe cerebral palsy. Eur Spine J 25(2):506–516
Weigl DM (2019) Scoliosis in non-ambulatory cerebral palsy: challenges and management. Isr Med Assoc J 21(11):752–755
Strom SF et al (2022) Is it necessary to fuse to the pelvis when correcting scoliosis in cerebral palsy? World J Orthop 13(4):365–372
Farshad M et al (2022) Pelvic fixation in surgical correction of neuromuscular scoliosis. N Am Spine Soc J 10:100123
Tondevold N et al (2020) Should instrumented spinal fusion in nonambulatory children with neuromuscular scoliosis be extended to L5 or the pelvis? Bone Joint J. https://doi.org/10.1302/0301-620X.102B2.BJJ-2019-0772.R2
Stiel N et al (2020) Pedicle screw instrumentation with or without pelvic fixation in neuromuscular scoliosis: outcome and complications in a series of 37 patients with a minimum 2-year follow-up. Surgeon 18(5):e7–e12
Shrader MW et al (2018) Inter- and intraobserver reliability of pelvic obliquity measurement methods in patients with cerebral palsy. Spine Deform 6(3):257–262
Castellvi AE, Goldstein LA, Chan DP (1984) Lumbosacral transitional vertebrae and their relationship with lumbar extradural defects. Spine 9(5):493–495
Vora V et al (2007) A pedicle screw construct gives an enhanced posterior correction of adolescent idiopathic scoliosis when compared with other constructs: myth or reality. Spine 32(17):1869–1874
Agha RA et al (2018) The process 2018 statement: updating consensus preferred reporting of case series in surgery (process) guidelines. Int J Surg 60:279–282
Murphy RF, Mooney JF 3rd (2019) Current concepts in neuromuscular scoliosis. Curr Rev Musculoskelet Med 12(2):220–227
Cloake T, Gardner A (2016) The management of scoliosis in children with cerebral palsy: a review. J Spine Surg 2(4):299–309
Vandendriessche E et al (2021) Complication rate after scoliosis surgery in children with cerebral palsy. Acta Orthop Belg 87(2):255–261
Yaszay B et al (2020) Major complications following surgical correction of spine deformity in 257 patients with cerebral palsy. Spine Deform 8(6):1305–1312
Turturro F et al (2017) Rate of complications due to neuromuscular scoliosis spine surgery in a 30-years consecutive series. Eur Spine J 26(Suppl 4):539–545
Menga EN et al (2020) Evaluating trends and outcomes of spinal deformity surgery in cerebral palsy patients. Int J Spine Surg 14(3):382–390
Adams AJ et al (2019) Surgeon and caregiver agreement on the goals and indications for scoliosis surgery in children with cerebral palsy. Spine Deform 7(2):304–311
Jain A et al (2018) Caregiver perceptions and health-related quality-of-life changes in cerebral palsy patients after spinal arthrodesis. Spine. https://doi.org/10.1097/BRS.0000000000002508
Arima H et al (2021) Combination of side-bending and traction radiographs do not influence selection of fusion levels compared to either one alone in adolescent idiopathic scoliosis. Global Spine J. https://doi.org/10.1177/21925682211015193
Malik S et al (2021) Preoperative supine traction radiographs often result in higher lenke classifications than supine bending radiographs in adolescent idiopathic scoliosis. Spine Deform 9(4):1049–1052
Siribumrungwong K, Dhanachanvisith N (2022) A comparative study of supine traction, supine side-bending radiographs, and supine mri to determine coronal flexibility in degenerative lumbar scoliosis patients. Spine Deform. https://doi.org/10.1007/s43390-022-00615-4
Koop SE (2009) Scoliosis in cerebral palsy. Dev Med Child Neurol 51(Suppl 4):92–98
Liu RW et al (2010) Comparison of supine bending, push-prone, and traction under general anesthesia radiographs in predicting curve flexibility and postoperative correction in adolescent idiopathic scoliosis. Spine. https://doi.org/10.1097/BRS.0b013e3181b3564a
Keeler KA et al (2010) Spinal fusion for spastic neuromuscular scoliosis: is anterior releasing necessary when intraoperative halo-femoral traction is used? Spine. https://doi.org/10.1097/BRS.0b013e3181d9527e
Takeshita K et al (2006) Analysis of patients with nonambulatory neuromuscular scoliosis surgically treated to the pelvis with intraoperative halo-femoral traction. Spine. https://doi.org/10.1097/01.brs.0000238964.73390.b6
Tondevold N et al (2021) Intraoperative traction in neuromuscular scoliosis surgery improves major curve correction when fusing to L5. Spine Deform 9(3):769–776
Badin D et al (2023) When to perform fusion short of the pelvis in patients with cerebral palsy?: indications and outcomes. JBJS Open Access. https://doi.org/10.2106/JBJS.OA.22.00123
Funding
The authors did not received support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
Ruben Alejandro Morales Ciancio: Made substantial contributions to the conception, design, analysis, and interpretation of data. Drafted and critically revised the work, approved the version to be published and agree to be accountable for all aspects of the work. Jonathan Lucas: Made substantial contributions to the analysis and interpretation of data. Drafted and revised the work, approved the version to be published and agree to be accountable for all aspects of the work. Stewart Tucker: Made substantial contributions to the analysis and interpretation of data. Revised the work, approved the version to be published and agree to be accountable for all aspects of the work. Thomas Ember: Made substantial contributions to the analysis and interpretation of data. Revised the work, approved the version to be published and agree to be accountable for all aspects of the work. Mark Harris: Made substantial contributions to the analysis and interpretation of data. Revised the work, approved the version to be published and agree to be accountable for all aspects of the work. Edel Broomfield: Made substantial contributions to the design, analysis, and interpretation of data. Revised the work, approved the version to be published and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose. The authors have no competing interests to declare relevant to the content of this article.
Ethical approval
Ethical approval was waived by the local Ethics Committee of Great Ormond Street Hospital under the number GOSH3357 in view of the retrospective nature of the study, and all the procedures being performed were part of routine care.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Morales Ciancio, R.A., Lucas, J., Tucker, S. et al. Can postoperative Cobb and pelvic obliquity corrections be predicted using supine traction X-rays in non-ambulatory patients with cerebral palsy fused to L5? A case series study. Spine Deform (2024). https://doi.org/10.1007/s43390-024-00880-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s43390-024-00880-5