Abstract
Purpose
The purpose of this study was to evaluate the gait posture of patients with adult spinal deformity (ASD) using a 3-dimensional motion analysis system (3DMAS) and to investigate whether it affects gait endurance.
Methods
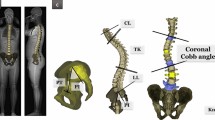
Fifty-one patients with ASD aged 50 years or older who were admitted to our hospital between March 2016 and March 2018 were included in the study. The subjects completed the 6-min walking test, which is an indicator of gait endurance. Static standing posture was assessed by whole-spine x-ray examination (coronal cobb angle, CCA; sagittal vertical axis, SVA; pelvic tilt, PT; and pelvic incidence minus lumbar lordosis, PI–LL). In addition, the gait posture was evaluated by a 3DMAS (dynamic trunk tilt angle, DTA; and dynamic pelvic tilt angle, DPA). The relationship between standing and gait postures and gait endurance was investigated by multivariable analysis.
Results
In univariable analysis, SVA, PI–LL, and DTA were associated with gait endurance. Furthermore, in the multivariable analysis, DTA showed the strongest association among the static and dynamic parameters (R2 = 0.61, β = − 0.35, P < 0.05).
Conclusions
An association was found between gait posture and gait endurance in patients with ASD. These findings can be useful to health care providers treating patients with ASD. It is advisable to assess the gait posture of patients with ASD because they present postural abnormalities during gait.



Similar content being viewed by others
Data availability
The datasets generated and/or analyzed in the current study are available from the corresponding author on reasonable request.
References
Diebo BG, Shah NV, Boachie-Adjei O et al (2019) Adult spinal deformity. Lancet 394(10193):160–172
Kado DM, Browner WS, Palermo L et al (1999) Vertebral fractures and mortality in older women: a prospective study. Study of Osteoporotic Fractures Research Group. Arch Intern Med 159(11):1215–1220
Cutler WB, Friedmann E, Genovese-Stone E (1993) Prevalence of kyphosis in a healthy sample of pre- and postmenopausal women. Am J Phys Med Rehabil 72(4):219–225
Kobayashi T, Atsuta Y, Matsuno T et al (2004) A longitudinal study of congruent sagittal spinal alignment in an adult cohort. Spine (Phila Pa 1976) 29(6):671–676
Glassman SD, Bridwell KH, Dimar JR et al (2005) The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976) 30(18):2024–2029
Schwab FJ, Blondel B, Bess S et al (2013) Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine (Phila Pa 1976) 38(13):E803-812
Engsberg JR, Bridwell KH, Reitenbach AK et al (2001) Preoperative gait comparisons between adults undergoing long spinal deformity fusion surgery (thoracic to L4, L5, or sacrum) and controls. Spine 26(18):2020–2028
Kado DM, Huang MH, Nguyen CB et al (2007) Hyperkyphotic posture and risk of injurious falls in older persons: the Rancho Bernardo Study. J Gerontol A Biol Sci Med Sci 62(6):652–657
Schwab F, Ungar B, Blondel B et al (2012) Scoliosis Research Society-Schwab adult spinal deformity classification: a validation study. Spine (Phila Pa 1976) 37(12):1077–1082
Yilgor C, Sogunmez N, Boissiere L et al (2017) Global alignment and proportion (GAP) Score: development and validation of a new method of analyzing spinopelvic alignment to predict mechanical complications after adult spinal deformity surgery. J Bone Joint Surg Am 99(19):1661–1672
Miyazaki J, Murata S, Horie J et al (2013) Lumbar lordosis angle (LLA) and leg strength predict walking ability in elderly males. Arch Gerontol Geriatr 56(1):141–147
Kondo R, Yamato Y, Nagafusa T et al (2017) Effect of corrective long spinal fusion to the ilium on physical function in patients with adult spinal deformity. Eur Spine J 26(8):2138–2145
Matsuyama Y (2017) Surgical treatment for adult spinal deformity: conceptual approach and surgical strategy. Spine Surg Relat Res 1(2):56–60
Marks MC, Stanford CF, Mahar AT et al (2003) Standing lateral radiographic positioning does not represent customary standing balance. Spine (Phila Pa 1976) 28(11):1176–1182
Lamartina C, Berjano P (2014) Classification of sagittal imbalance based on spinal alignment and compensatory mechanisms. Eur Spine J 23(6):1177–1189
Arima H, Yamato Y, Hasegawa T et al (2017) Discrepancy between standing posture and sagittal balance during walking in adult spinal deformity patients. Spine (Phila Pa 1976) 42(1):E25-30
Shiba Y, Taneichi H, Inami S et al (2016) Dynamic global sagittal alignment evaluated by three-dimensional gait analysis in patients with degenerative lumbar kyphoscoliosis. Eur Spine J 25(8):2572–2579
Miura K, Kadone H, Koda M et al (2020) Thoracic kyphosis and pelvic anteversion in patients with adult spinal deformity increase while walking: analyses of dynamic alignment change using a three-dimensional gait motion analysis system. Eur Spine J 29(4):840–848
Bae J, Theologis AA, Jang JS et al (2017) Impact of fatigue on maintenance of upright posture: dynamic assessment of sagittal spinal deformity parameters after walking 10 minutes. Spine (Phila Pa 1976) 42(10):733–739
von Elm E, Altman DG, Egger M et al (2014) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Sug 12(12):1495–1499
ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories (2002) ATS statement: guidelines for the six-minute walk test. Am J Resp Crit Care Med 166(1):111–117
Weir NA, Brown AW, Shlobin OA et al (2013) The influence of alternative instruction on 6-min walk test distance. Chest 144(6):1900–1905
Naresh-Babu J, Viswanadha AK, Ito M et al (2019) What should an ideal adult spinal deformity classification system consist of? Review of the factors affecting outcomes of adult spinal deformity management. Asian Spine J 13(4):694–703
Nathan ST, Roberts CS, Deliberato D (2012) Lumbar paraspinal compartment syndrome. Int Orthop 36(6):1221–1227
Konno S, Kikuchi S, Nagaosa Y (1994) The relationship between intramuscular pressure of the paraspinal muscles and low back pain. Spine (Phila Pa 1976) 19(19):2186–2189
Takahashi I, Kikuchi S, Sato K et al (2007) Effects of the mechanical load on forward bending motion of the trunk: comparison between patients with motion-induced intermittent low back pain and healthy subjects. Spine (Phila Pa 1976) 32(2):E73-78
Severijns P, Moke L, Overbergh T et al (2021) Dynamic sagittal alignment and compensation strategies in adult spinal deformity during walking. Spine J 21(7):1059–1071
Acknowledgements
The authors wish to acknowledge those who participated in this study and those who assisted in writing and proofreading this paper.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
KS, RT, TE, TM, MI, TI and OS: Made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data; or the creation of new software used in the work. Drafted the work or revised it critically for important intellectual content. Approved the version to be published. Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interest to disclose.
IRB approval
The current study was approved by our institutional review board (IRB No. 29359).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sato, K., Tominaga, R., Endo, T. et al. The association of dynamic spinal alignment on gait endurance of patients with adult spinal deformity: a cross-sectional study. Spine Deform 11, 463–469 (2023). https://doi.org/10.1007/s43390-022-00605-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-022-00605-6



