Abstract
Purpose
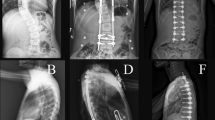
Temporary internal distraction (TID) is a surgical technique used to correct severe scoliosis. We sought to evaluate the long-term outcomes associated with temporary internal distraction (TID) for severe scoliosis.
Methods
Scoliosis patients who underwent TID from 2006 to 2019 at a single institution were identified. Patients with coronal Cobb angles ≥ 90° or congenital scoliosis, and ≥ 2-year follow-up were included. Clinical and imaging data were reviewed for patient and operative characteristics and complications. Patient-reported outcomes were also analyzed.
Results
51 patients (37 female) were included. Mean age at surgery was 14.3 ± 3.5 years. Mean follow-up was 5.8 ± 3.0 years. Eighteen (35%) curves were idiopathic, 24 (47%) were cerebral palsy (CP) related, and 9 (18%) were congenital. Mean Cobb angle was 103° preoperatively and 20° at final follow-up, with an intermediate angle of 55º in staged procedures. Intraoperative neuromonitoring changes occurred in 13 (25.4%) cases, but all returned to baseline with immediate lessening of distraction. Overall, three (5.8%) cases of wound dehiscence, five (9.7%) cases of deep infections, one (2%) case of screw protrusion, and one (2%) case of delayed extremity weakness occurred. Patient-reported outcomes significantly improved at final follow-up.
Conclusion
Our findings suggest that TID is a valuable adjunct for correcting severe scoliosis. The mean Cobb reduction achieved (81%) was higher than that reported for halo-traction and was sustained over long-term follow-up. TID also allowed a shorter a hospital stay. While intraoperative neuromonitoring changes were not uncommon, they were reversible. However, care must always be exercised as major corrections may rarely result in delayed neurologic deficits despite intact neuromonitoring.
Level of evidence
Therapeutic—Level III.



Similar content being viewed by others
References
O’Brien JP, Yau AC, Smith TK et al (1971) Halo pelvic traction. A preliminary report on a method of external skeletal fixation for correcting deformities and maintaining fixation of the spine. J Bone Joint Surg Br 53(2):217–229
Kumar K (1996) Spinal deformity and axial traction. Spine (Phila Pa 1976) 21(5):653–655
Sink EL, Karol LA, Sanders J et al (2001) Efficacy of perioperative halo-gravity traction in the treatment of severe scoliosis in children. J Pediatr Orthop 21(4):519–524
Buchowski JM, Bhatnagar R, Skaggs DL et al (2006) Temporary internal distraction as an aid to correction of severe scoliosis. J Bone Joint Surg Am 88(9):2035–2041
Skaggs DL, Lee C, Myung KS (2014) Neuromonitoring changes are common and reversible with temporary internal distraction for severe scoliosis. Spine Deform 2(1):61–69
Buchowski JM, Skaggs DL, Sponseller PD (2007) Temporary internal distraction as an aid to correction of severe scoliosis. Surgical technique. J Bone Joint Surg Am 89(Suppl 2):297–309
Narayanan U. CPCHILD: Caregiver priorities & child health index of life with disabilities. Available at https://lab.research.sickkids.ca/pscoreprogram/wp-content/uploads/sites/72/2017/09/CPCHILD_English_Parent_5.0_Watermarked.pdf. Accessed 23 Apr 2020
Narayanan UG, Fehlings D, Weir S et al (2006) Initial development and validation of the Caregiver priorities and child health index of life with disabilities (CPCHILD). Dev Med Child Neurol [Internet] 48(10):804–812. https://doi.org/10.1111/j.1469-8749.2006.tb01227.x/pdf
Lewis NDH, Keshen SGN, Lenke LG et al (2015) The deformity angular ratio: does it correlate with high-risk cases for potential spinal cord monitoring alerts in pediatric 3-column thoracic spinal deformity corrective surgery? Spine (Phila Pa 1976) 40(15):E879–E885
Nachemson A, Elfström G (1971) Intravital wireless telemetry of axial forces in Harrington distraction rods in patients with idiopathic scoliosis. J Bone Joint Surg Am 53(3):445–465
Elfström G, Nachemson A (1973) Telemetry recordings of forces in the Harrington distraction rod: a method for increasing safety in the operative treatment of scoliosis patients. Clin Orthop Relat Res 93:158–172
Edgar MA, Chapman RH, Glasgow MM (1982) Pre-operative correction in adolescent idiopathic scoliosis. J Bone Joint Surg Br 64(5):530–535
Letts RM, Palakar G, Bobecko WP (1975) Preoperative skeletal traction in scoliosis. J Bone Joint Surg Am 57(5):616–619
Saifi C, Laratta JL, Petridis P et al (2017) Vertebral Column Resection for Rigid Spinal Deformity. Glob spine J 7(3):280–290
Lenke LG, Newton PO, Sucato DJ et al (2013) Complications after 147 consecutive vertebral column resections for severe pediatric spinal deformity: a multicenter analysis. Spine (Phila Pa 1976) 38(2):119–132
Suk S-I, Chung E-R, Kim J-H et al (2005) Posterior vertebral column resection for severe rigid scoliosis. Spine (Phila Pa 1976) 30(14):1682–1687
Hamzaoglu A, Alanay A, Ozturk C et al (2011) Posterior vertebral column resection in severe spinal deformities: a total of 102 cases. Spine (Phila Pa 1976) 36(5):E340–E344
**e J, Wang Y, Zhao Z et al (2012) Posterior vertebral column resection for correction of rigid spinal deformity curves greater than 100°. J Neurosurg Spine 17(6):540–551
Funding
No funding was received in support of this work.
Author information
Authors and Affiliations
Contributions
Conception and design, analysis of data, manuscript drafting, manuscript revision: DB, AG, DLS, PDS, IRB. Acquisition of data: DB, AG. Interpretation of data: DB, DLS, PDS. We declare that all authors have met all four authorship criteria: (1) Made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data; or the creation of new software used in the work. (2) Drafted the work or revised it critically for important intellectual content. (3) Approved the version to be published. (4) Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
David Skaggs received grants or contracts from NuVasive, royalties or licenses from Wolters Kluwer Health and Zimmer Biomet, consulting fees from ZimmerBiomet, Top Doctors, and Orthobullets, payment or honoraria from ZimmerBiomet, leadership or fiduciary roles in Pediatric Spine Study Group, Pediatric Spine Foundation, Spine Deformity, Orthopedics Today, Journal of Children’s Orthopedics, Stock or Stock option in Zipline Medical, Green Sun Medical, Orthobullets. Paul Sponseller received consulting fees from Orthopediatrics, Johnson and Johnson, and Nuvasive, payment or honoraria from Johnson and Johnson, and Nuvasive, support for attending meetings/travel from Johnson and Johnson, leadership or fiduciary role in Scoliosis Research Society and Marfan Foundation. All other authors have no disclosures.
Ethical approval
This study was approved by the Johns Hopkins Institutional Review Board (IRB).
Informed consent
Informed consent or a waiver of informed consent was obtained where applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Badin, D., Gupta, A., Skaggs, D.L. et al. Temporary internal distraction for severe scoliosis: two-year minimum follow-up. Spine Deform 11, 341–350 (2023). https://doi.org/10.1007/s43390-022-00602-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-022-00602-9