Abstract
The occurrence of a major medical event usually leads to a surge in the generation of medical waste. If the waste generated is not disposed of in a timely manner, it can pose a great threat to humans and the surrounding environment. Based on the large volume and hazardous nature of medical waste, this research explores the social value and importance of establishing a professional network for medical waste reverse logistics. A three-tier recycling network model consisting of recycling centres, testing and processing centres, reprocessing centres, power plants and landfill plants has been developed based on the special characteristics of medical waste. A mixed integer linear programming (MILP) model was developed with the goal of minimizing costs. Genetic algorithm, MILP solver and Lingo solver are used to solve the problem of node selection and waste recycling volume allocation in the network. Several datasets were utilized to verify the effectiveness, demonstrating better solutions for problems of varying sizes. The results of the case study show that genetic algorithm can show good results in solving problems of different sizes. The solver's ability to solve the problem decreases as it grows in size. By comparing the methods used, choosing an efficient and accurate approach to the reverse logistics recovery problem has become more achievable. The results of the case study show the stability of the reverse logistics optimization model at different scales. The construction of the reverse logistics network optimization model resulted in lower total recycling costs and higher recycling efficiency. Finally, some insights are given based on the obtained results.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
With the pace of socialist modernization, China's national economy and people's living standards have improved tremendously, and healthcare has also developed greatly. The rapid development of medical care has led to more people becoming involved in medical research and more people are using medical technology to change their quality of life (e.g. vaccines, beauty treatments, massages, etc.). More and more medical activities are generating more medical waste. Improperly handled and disposed medical waste poses a potential risk of infection or injury to healthcare workers and the surrounding community. How to manage as well as dispose of the increasing amount of medical waste has become a major issue in medical waste research. If discarded or disposed of at will without implementing strict recycling procedures, it will certainly endanger people's lives and health, and can have a significant negative impact on the ecological environment (Wang et al. 2013). The worldwide outbreak of the coronavirus in 2020 has exposed many problems of inadequate medical waste disposal capacity. The sudden surge of medical waste has made it difficult for medical waste disposal facilities to meet the disposal efforts of various hospitals. Various outstanding issues such as the lack of space reserved for responding to sudden large-scale public health events, inadequate construction of facilities and gaps in transfer capacity need to be addressed (Yu et al. 2020).
In the early 1990s, China's medical waste agenda called for better management and disposal of medical waste to prevent public health problems and environmental pollution caused by improper disposal of medical waste. In 2003, for the first time, China put forward relevant methods and regulations on how to manage and dispose of medical waste, requiring medical units at all levels to dispose of their medical waste to professional treatment enterprises according to the principle of centralised waste disposal in the vicinity. At the same time, research into environmental pollution and management has yielded many results that have made it possible to maximize the value of medical waste recycling in China, and some modern cities in China have begun to research and make some progress in the treatment of medical waste recycling. China is a late starter in the study of medical waste recycling and its recycling technology lags behind that of other developed countries, so there has been no uniform recycling standard for medical waste. Properly understanding and evaluating the current state of management of urban medical waste reverse logistics networks, addressing the lack of efficiency in the disposal of medical waste, reducing the hoarding of medical waste, and providing reasonable countermeasures for the possible surge of medical waste caused by the epidemic in the post-epidemic period, is of great significance in promoting sustainable urban development and ensuring the circular development of the social economy.
Research into the volume and composition of medical waste can help to better manage it. The amount of waste generated and the components of waste are complex, but in a previous statistical study of health care waste in Canadian health care facilities, it was found that the type of health services provided by the facility played a key role in the generation and composition of waste. The study found that as much as 52% of overall in-fectious medical waste production comes from short-term patients in rehabilitation service, followed in descending order by analytical laboratories (23%), surgeries (14%), dialyses (7%) and first aid (4%). A similar study done in Taiwan found the dialysis unit to generate the greatest amount of infectious medical waste (23%), flowed by the intensive care unit (17%), the emergency care unit and the outpa- tient clinic (12% each).
Apart from the logistics of recycling medical waste, managing the recycling network for medical waste is another key issue in handling medical waste. During the COVID-19 pandemic, there has been a significant increase in the amount of medical waste generated, leading to a major environmental challenge. The emergence of the COVID-19 epidemic has been a wake-up call. Responses need to be developed to prevent the environmental damage and human harm caused by medical waste. Medical waste management, as a waste supply chain network design issue, falls under the umbrella of reverse supply chain networks. The medical waste reverse supply chain network has a number of unique characteristics that set it apart from other waste management networks, some of which are as follows:
-
The amount of medical waste generated cannot be determined and may increase or decrease as a result of social events.
-
Medical waste needs to be disposed of in a timely manner after it is generated, and prolonged stockpiling may directly lead to environmental pollution.
-
Concentrated sources of medical waste generation. During major epidemics, epidemic-related medical waste is mainly generated in designated hospitals, centralised.
Therefore, there is a need to provide a different management framework and to design a special reverse supply chain network to address the uncertain challenges posed by medical waste. The main contributions and components of this work can be summarised as follows:
-
A new mixed integer mathematical model is proposed for designing a reverse logistics network for medical waste recycling under uncertainty. The model allows medical waste recycling methods at different scales to be considered to determine the optimal decision for the network such that the total cost of the system is minimized.
-
Multiple methods are provided to solve the problems in the model. In order to be further efficient, the most efficient and least costly method should be adopted to design the network at different recycling scales.
-
Computer simulations of multiple data sets are used to verify the stability of the model and to demonstrate that the model has some optimization effects and can be applied to the optimization of actual medical waste recycling networks.
-
Analysis of medical waste recycling data at different scales to validate model performance and provide management insights into the whole process of medical waste recycling.
Building a reasonable model of medical waste reverse logistics can help the authorities to achieve efficient and safe recycling of medical waste. Setting up multi-stage recycling facilities can help improve the treatment capacity of municipal medical waste and the recycling capacity of waste resources.
2 Literature review
2.1 Medical Waste
2.1.1 Definition
The United States Congress' 1988 publication "The United States Medical Waste Tracking" contains the earliest official definition of medical waste. This defined medical waste as any solid waste generated in the course of the diagnosis, treatment, immunization of humans or animals and the production or testing of biological products(Windfeld and Brooks , 2015). Due to the lack of a uniform definition of medical waste in the early stages of research, Almuneef et al.(Almuneef and Memish , 2003) argued that the lack of a universally accepted definition had led to the emergence of many infectious waste problems. In order to avoid health care problems caused by the lack of uniformity in the definition of healthcare waste, many countries and regions had given clear guidelines for the management of healthcare waste for reference purposes(Insa et al. , 2010).
With the advancement of health care and technology, the US Environmental Protection Agency had provided a clear definition of medical waste. It stated that all waste generated by any healthcare or healthcare-related facility are medical waste (Epa 2012a). Medical waste mainly comes from medical waste sites such as hospitals, clinics, laboratories, etc., where the activities of these sites result in the generation of medical waste, and likewise the institutions associated with these sites also generate a portion of medical waste, such as dental clinics, drug rehabs, nursing homes, etc.[7~8]. Having a clear definition of medical waste can assist relevant personnel in effectively classifying such waste and minimizing potential risks that may arise as a result of unclear definitions.
2.1.2 Management
Due to the increase in healthcare and people's efforts to eliminate health hazards and solve health problems, more and more waste is inevitably generated. However, if such waste is not properly managed, it can pose great harm to both human health and the environment[9~12]. In the early stages of research on medical waste management, comprehensive waste management plans were proposed, including ideological education, on-the-job training and written policies on waste management to reduce the generation of medical waste and the cost of disposal[13~15].
The research of medical waste management networks helps the relevant authorities to better reduce the negative impact of medical waste on the lives of residents and healthcare facilities. One of the first to propose a medical waste management network was Shi et al. who argued that the only way to minimize disposal costs was to construct a specially structured logistics model for recycling medical waste (Shi et al. 2009). However, the problem with the early research was that the model was more idealistic and lacked actual data for comparison. The level of medical waste networks at that time could not meet the conditions of the model, so there was still more room for improvement. Research in recent years has focused on practical aspects of how improving existing recycling models can help to better address the management of medical waste. Mantzaras et al.(Mantzaras and Voudrias , 2017) used Geographic Information Systems (GIS) to specify candidate sites for treatment facilities, transfer stations and landfill plants, and applied this to an actual recycling network to demonstrate the reliability of the optimization model. The model developed by Kargar et al.(Kargar et al. , 2020), who argued that the mismanagement of medical waste must pose serious risks to humans and the environment, is based on a linear programming model with multi-objective uncertainty that considers sustainability criteria and environmental issues, and has sufficient potential and scope to be exploited. The global outbreak of COVID-19 in 2020 has led to an extremely high level of medical waste generation in various countries and has led to a new direction of research into medical waste. Monserrate and Khaled et al.[19~20] argued that the decrease in recyclable medical waste and the increase in the amount generated will further increase the environmental impact and damage, and more measures need to be taken to improve the management of medical waste during an epidemic. Other scholars have argued that in the face of the burgeoning amount of medical waste, successful management of medical waste can only be achieved if multiple disposal vendors work together(Valizadeh and Mozafari , 2021). Meanwhile, the government should also provide some assistance at the appropriate management level to jointly address the environmental problems caused by the accumulation of medical waste.
Due to the specific type of medical waste, the study of routes and collection points for recycling medical waste had also become a hot topic. Govindan and Tirkolaee [22~24] have developed a medical waste management network for medical waste disposal routes to minimize the damage caused by medical waste to the living environment during recycling and disposal, with the implementation of appropriate algorithms to maximize the efficiency of the health hazards of medical waste. A number of forecasting experts have joined the study of medical waste management networks to prevent the occurrence of accidents that could lead to the breakdown of disposal facilities in advance. Hao et al.(Hao et al. , 2019) developed an improved grey neural network model using single variable grey model and triple exponential smoothing to predict the factors affecting the amount of recycling and selected the better predictions to train a particle swarm optimization optimized back propagation (BP) neural network to be used to predict the recycling of medical waste. **n et al.(**n et al. 2023) used time-varying and lagging factors to construct models to predict waste volumes and adopt optimized models for their recycling, achieving early warning and safe waste management with significant positive impact on epidemic stability and lifelong health.
Although the management protocols for medical waste are relatively mature, the sudden surge in waste production may still result in delayed or inadequate processing. So the future research should focus on enhancing the compatibility of medical waste management networks.
2.1.3 Recycle
Early research into the recycling of medical waste was guided by circular economics for a single type of waste. However, after years of research progress, scholars have found that in addition to controlling the costs of the recycling process, the safety aspects of it should also be considered, considering that medical waste is an extremely dangerous category of waste product. Ganghe et al.(Zheng Gang He, Sha Liu. The Research on Recovery Network Optimization of Medical Waste[J] , 2015) developed a medical waste recycling network considering load balancing and solved it using a genetic algorithm, through which the model was constructed to effectively reduce transport risk. Mustafa et al.[28~29] considered the economic value of waste in their study of medical waste recycling and used energy value analysis to assess the true economic potential of recycling medical waste. The study of the value of recycling has shown that the value of useful medical waste is higher if it is fully recycled, which has had a significant positive impact on reducing recycling costs. Gao et al.(Optimisation and of Urban Medical Waste Recycling Network considering Differentiated Collection Strategy and Time Windows[J]. , 2021) studied a comprehensive optimization problem for urban medical waste recycling networks and proposed a compact mixed integer linear programming model that considers differentiated aggregation strategies and time windows, which works well for large-scale medical waste recycling systems, and the method provides sufficient management impact on recycling companies. Zhang et al.(Wanting et al. , 2022) proposed a multi-loop path problem for medical waste recycling vehicles and used a neighbourhood search algorithm to ensure efficiency when processing large problems, and the proposed method played a positive role in studying the path of medical waste recycling vehicles. Snyanta et al.(Sayanta and Kumar , 2022) proposed a new group decision making process from a manager's perspective combining AHP and WASPAS and applied it to medical waste recycling technology, through which it can help managers to provide the best decision making options when managing medical waste recycling in their region.
In past studies on the recycling of medical waste, the recycling network was often regarded as a two-tier system. However, such a system may not fully realize the maximum residual value of medical waste. In this research, we propose a three-tier recycling network for medical waste, which can effectively reduce recycling costs by extracting additional residual value compared to a two-tier system.
2.2 Reverse Logistics
In the history of reverse logistics research, the first person to propose the concept of reverse logistics was Stock, who defined reverse logistics as a network activity that includes the process of returning products, reusing items, reprocessing and remanufacturing(Stock 1998). With the development of research on reverse logistics and people's increased awareness of environmental protection, many scholars have begun to study green and circular economy reverse logistics networks in reverse logistics systems, so that the value of recycled products can be maximized and the economic value of recyclables can be reduced to waste. Xu et al.(**aofeng et al. , 2021) for the Green Vehicle Path Problem (GVRP) study designed a three-level coded NSGA-III algorithm which proved to be a superior optimization algorithm. Ghezavati et al.(Ghezavati and Beigi , 2016) designed a multi-echelon reverse logistics network with a meta-heuristic process with a time window. The study considers environmental and social pressures and is optimising and reliable for real cases. While considering the efficiency of reverse logistics recycling, the value stream of reverse logistics also needs to be considered. Zhou et al.(Zhou et al. , 2018) used value stream analysis to construct a reverse logistics costing and optimization model for how enterprises can optimize their costs and achieve coordinated social, economic and environmental development, and made generic recommendations for enterprises. Zamani et al.(Zamani et al. , 2020) designed a reverse logistics network that considers pricing and uncertainty so that the final reverse logistics recycling system can achieve the lowest cost and lowest risk. The use of robust optimization models for uncertainty influences is also a very accurate solution (**aofeng et al. , 2022).
In a reverse logistics network, the timeliness of recovery is also an important evaluation indicator. The punctuality of recycling networks is an important factor in people's satisfaction and in ensuring environmental health, so Emadedin(Hashemi Seyed Emadedin 2021) constructed a sustainable recycling network that takes into account customer needs to reduce emissions, and Xu et al.(**aofeng et al. 2022) used a knowledge-corrected data-driven model for trajectory prediction for traffic subjects, providing an adequate reference for the study of the timeliness of reverse logistics. In addition, long-distance recycling networks can bring high levels of customer satisfaction, while short-distance recycling networks are a question worth looking into (**aofeng and Zhifei 2023). Reverse logistics, as an important part of the logistics network, plays an important role in addressing the environment and promoting sustainable development.
3 Problem statement
3.1 Problem definition
3.1.1 Network design
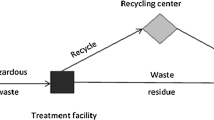
Medical waste is mainly collected and transferred before entering the recycling network. Medical waste is collected from major medical waste generators such as hospitals and outpatient clinics. Medical waste is packed, boxed and vacuumed by local regulations and delivered to a designated location for temporary storage on a daily basis, mainly in the form of mobile collection by waste collection vehicles and temporary storage in medical waste bins. The disposal of temporarily stored medical waste consists of two main forms: professionals who take it to the disposal point themselves and recycling organizations who go for active collection. Once the medical waste is in the recycling network, it is sorted and processed accordingly. The specific collection process is shown in Fig. 1 below.
The objective of the problem is to determine the optimal distribution route, the optimal amount of recycling and how to dispose of the medical waste in a reverse logistics network. Within this reverse logistics network, there are five main facilities including (1) recycling centres, (2) testing and processing centres, (3) reprocessing centres, (4) landfill plants, and (5) power plants. For recycling centres, the size of different recycling centres may vary significantly, so the difference in the volume of medical waste generated by each centre may be large, which also poses a higher challenge to the model calculation. The testing and processing centre is responsible for testing and sorting out hazardous substances from the various recycling centres to prevent any additional negative impact on the next level of waste. Tertiary facilities are reprocessing centres, landfill plants and power plants. The reprocessing centre focuses on the reprocessing of medical waste from upstream where there is still residual value to be extracted to utilize its full value. Power plant is used to dispose of medical waste that has no residual value but can be used for thermal power generation. Landfill plant is for the disposal of hazardous medical waste that can only be disposed of in landfills.
The large amount of medical waste piling up during the epidemic and the problem of infected medical waste require us to dispose of medical waste in a timely and expeditious manner. The question of how to recycle all the medical waste generated by the city at the lowest cost is the subject of this study. The number of recycling facilities at each level is considered to be multiple, so not all recycling facilities are necessarily used in the recycling network. Accordingly this study constructs an optimized reverse logistics network structure for medical waste based on the existing facilities, as shown in Fig. 2 below.
The aim of the network is to dispose of the medical waste generated in each cycle with the minimum amount of resources to the maximum extent possible. The whole process of handling medical waste is as follows: (1)All medical waste generated at the recycling centres is transferred from the recycling centres to the various testing and processing centres. (2) The testing and processing centres carries out the first step of processing and sorting of waste from the recycling centres and after completion sends it to the next level of treatment facility. The classification at this stage mainly includes residual value extractable medical waste and non-residual value non-extractable medical waste, which can be divided into medical waste that can be used for power generation and medical waste that can only be landfilled. The testing and processing centres complete the environmentally sound treatment of medical waste and then move on to the next level of the network. (3) Each treatment facility carries out the treatment of this facility and the medical waste treatment is completed.
3.1.2 Model assumption
The model for optimizing the reverse logistics network for medical waste is based on specific requirements.
Due to the uncertainty of the data and the inaccuracy of the environment, we need to make some assumptions about the model, and the assumptions required for this model are as follows:
-
Because the recycling rules for medical waste require timely processing and no storage, the total amount of recycling within the designated period is selected as the research object to determine the recycling period. The research examines the total recycling cost within one or more recycling periods.
-
Each process has a correspondingly selectable number of options between them, including testing and processing centres, reprocessing centres, landfill plants and power plants, otherwise the study would be meaningless..
-
Assuming that there are capacity limits for the testing and processing centers, reprocessing centers, landfill plants, and power plants. Only medical waste that can be transported within the limit of each facility's capacity can be stored and processed.
-
All process costs should be calculated and no transgressions should occur, i.e. cost calculations should be based on the direction of the path in the medical waste recycling network structure and no cost calculations should be made for structures that are not connected through.
-
We should consider the operation and maintenance costs of the recycling centres, testing and processing centres, reprocessing centres, landfill plants, power plants in addition to the basic transport costs when carrying out cost calculations, thus preventing a design approach that optimizes the network based on unit transport costs alone.
-
Consideration should be given to the value generated by medical waste with residual value that is treated in reprocessing centres and medical waste without residual value but is incinerated for power generation, but not as a reduction in cost.
-
Not all facilities in the recycling network will be used. Some processing facilities can be shut down if it keeps costs down.
-
More value is created by power generation activities versus reprocessing activities, so it is considered that reprocessing costs are less than the residual value of the waste and that the value of the resources generated by power generation is greater than the costs required to generate the electricity. Therefore, the cost of reprocessing is not considered in relation to the cost of generating electricity.
3.2 Mathematical modeling
3.2.1 Notation list
The definitions of the relevant symbols, parameters and variables in the medical waste reverse logistics network model are as follows.
Fixed parameters
-
R: Set of locations for recycling centres; r ∈ {1,…,R}.
-
S: Set of locations for testing and processing centres; s ∈ {1,…,S}.
-
D: Set of locations for reprocessing centres; d ∈ {1,…,D}.
-
P: Set of locations for power plants; p ∈ {1,…,P}.
-
L: Set of locations for landfill plants; l ∈ {1,…,L}.
-
T: Set of periods: t ∈ {1,…,T}.
-
MOSs: Maximum handling capacity of the testing and processing centre s.
-
MODd: Maximum handling capacity of the reprocessing centre d.
-
MOPp: Maximum handling capacity of the power plant p.
-
MOLl: Maximum handling capacity of the landfill plant l.
-
FCRr: Fixed costs for recycling centre r.
-
FCSs: Fixed costs for testing and processing centre s.
-
FCDd: Fixed costs for reprocessing centre d.
-
FCPp: Fixed costs for power plant p.
-
FCLl: Fixed costs for landfill plant l.
-
UCRr: Unit operating costs of recycling centre r.
-
UCSs: Unit operating costs of testing and processing centre s.
-
UCDd: Unit operating costs of reprocessing centre d.
-
UCPp: Unit operating costs of power plant p.
-
UCLl: Unit operating costs of landfill plant l.
-
LRSrs: transport distance of medical waste from recycling centre r to testing and processing centre s.
-
LSDsd: transport distance of medical waste from testing and processing centre s to reprocessing centre d.
-
LSPsp: transport distance of medical waste from testing and processing centre s to power plant p.
-
LSLsl: transport distance of medical waste from testing and processing centre s to landfill plant l.
-
RTSrst: Unit transportation cost of medical waste from recycling centre r to testing and processing centre s in period t.
-
STDsdt: Unit transportation cost of medical waste from testing and processing centre s to reprocessing centre d in period t.
-
STPdpt: Unit transportation cost of medical waste from testing and processing centre s to power plant p in period t.
-
STLdlt: Unit transportation cost of medical waste from testing and processing centre s to landfill plant l in period t.
-
LD: Unit landfill cost of medical waste.
-
P: Proportion of hazardous medical waste in testing and processing centre
-
β: Proportion of recyclable medical waste in testing and processing centre
-
ω: Unit disposal cost for hazardous medical waste
Uncertain parameters
-
VORrt: Volume of medical waste collected by recycling centre r in period t.
Decision variables
-
vrsrst: Volume of medical waste transported from recycling centre r to testing and processing centre s in period t
-
vsdsdt: Volume of medical waste transported from testing and processing centre s to reprocessing centre d in period t
-
vspspt: Volume of medical waste transported from testing and processing centre s to power plant p in period t
-
vslslt: Volume of medical waste transported from testing and processing centre s to landfill plant l in period t
-
rxr: 1 if medical waste is generated at this recycling centre r, 0 otherwise
-
sxs: 1 if the testing and processing centre s is used, 0 otherwise
-
dxd: 1 if the reprocessing centre d is used, 0 otherwise
-
pxp: 1 if the power plant p is used, 0 otherwise
-
lxl: 1 if the landfill plant l is used, 0 otherwise
The model
The objective function aims to minimize the total cost of the reverse logistics network, including:
-
Fixed costs for recycling centres:
$$TFR={\textstyle\sum_{r=1}^R}{rx}_r{\times FCR}_r$$(1)
Fixed costs for testing and processing centres:
Fixed costs for reprocessing centres:
Fixed costs for power plants:
Fixed costs for landfill plants:
Unit operating costs of recycling centres:
-
Unit operating costs of testing and processing centres:
$$AOS={\textstyle\sum_{t=1}^T}{\textstyle\sum_{S=1}^S}{\textstyle\sum_{r=1}^R}{vrs}_{rst}\times{UCS}_s$$(7)
Unit operating costs of reprocessing centres:
Unit operating costs of power plants:
Unit operating costs of landfill plants:
Transportation costs from recycling centres to testing and processing centres:
Transportation costs from testing and processing centres to reprocessing centres:
Transportation costs from testing and processing centres to power plants:
Transportation costs from testing and processing centres to landfill plants:
Cost of disposal of hazardous medical waste:
Cost of landfilling medical waste:
Considering the above terms, the total cost objective function can becalculated as follows:
The constraints of the problem are as follows:
Constraints (18)—(22) represent equal inflow and outflow at all levels of the facility and balanced logistics transport during the recycling process of medical waste.
Constraints (23)—(26) indicate that the inflow at each level of the facility does not exceed the maximum capacity of that level of the facility.
3.3 The solution approaches
The problem proposed in this research is a mixed-integer mathematical programming model. The scale of medical waste recycling varies, and different regions have different recycling rules. To further improve the compatibility of the model, we adopt three methods in this section to solve the problem. We simulated multiple sets of data with different sizes according to the set parameters and compared the results obtained from various methods. By intuitively comparing the results, we can select the optimal solution method for each problem scale.
3.3.1 Genetic Algorithm
Genetic algorithm is the algorithm proposed by John holland in the 1970s that find optimal solutions by mimicking the mechanisms of selection and heredity in nature. Genetic algorithm can be used to achieve smaller and smaller satisfactory solutions to minimal value objective function problems by iterating over and over again to get closer and closer to the optimal solution. Traditional optimization algorithms can only find local optimal solutions for optimization problems, and the results obtained are highly dependent on the initial values. Genetic algorithm offers better convergence than traditional optimization algorithms, less computational time and higher robustness when computational accuracy is required. The problem to be solved in this research is a mixed integer linear programming problem with minimal total cost. The application of genetic algorithm with global search capability and the ability to escape from local optimal solutions can help to obtain satisfactory results for the proposed problem more quickly. Therefore, this research begins with the optimal solution of a reverse logistics network for medical waste using genetic algorithm. The flow chart of the genetic algorithm is shown in Fig. 3.
A genetic algorithm is used to solve the problem and achieve the output of the optimal network, with the following algorithmic framework.
-
1.
Read in test instance data.
-
2.
Encode the recall centre sort into chromosomes and initialise a population at random.
-
3.
Calculate fitness values for individuals.
-
4.
Design genetic operators:
-
5.
Selection: selecting the chromosome with the better fitness by means of roulette wheel.
-
6.
Crossover: randomly crossing over some genes of two chromosomes using the sub-path crossing method.
-
7.
Mutation: reverse sequencing of selected segments of random chromosomes using chromosome segment reversal methods.
-
8.
Sets the maximum number of iterations of the algorithm. When the maximum number of iterations is reached, the calculation stops and the current optimization result is output.
In the specific application of the genetic algorithm, the chromosome framework should be constructed first after determining the input parameters, and the chromosome generation process should be carried out after the construction is completed, with the following coding process.

This is followed by a selection process in which the chromosomes in each generation of the population are selected for later crossover and variation, using a roulette wheel to select the more adapted chromosomes. The selection process is as follows.

The chromosome crossover operation was then performed, using the sub-pathway crossover method to randomly crossover parts of the genes of both chromosomes, with the chromosome crossover proceeding as follows.

The next step proceeds with the chromosome mutation operation and the process of chromosome mutation is shown below.

Different problems will have different termination judgment conditions. At a specified maximum number of iterations, the chromosome that produces the maximum fitness function value within the maximum number of iterations is recorded using the maximum fitness value as the judgement criterion, and the optimal chromosome is obtained after comparison, i.e. the site selection point and the optimal path combination that minimizes the total cost.
In practical cases, the process of using genetic algorithms to solve problems typically involves the following steps:
-
1.
Chromosome Encoding. Based on the model developed, a four-layer coding design approach was adopted. The first layer is the testing and processing centre, the second layer is the reprocessing centre, the third layer is the power plant and the fourth layer is the landfill plant. The length of each layer code is the number of units available for that facility. The coding structure is shown in Fig. 4 below.
-
2.
Generating Initial Population. Generating a 0 matrix of (R*max(S, D, P, L),4). The overall framework of the chromosome is constructed based on the number of recycling centres. Where the length of the overall chromosome frame is the product of the maximum number of recycling centres and the maximum number of testing and processing centres, reprocessing centres, landfill plants and power plants. The width is 4.
When generating the initial solution, assume that there are 10 recycling centres and max(S, D, P, L)=5. If the first recycling centre is selected as the 2nd testing and processing centre, the 1st reprocessing centre, the 3rd power plant and the 1st landfill plant, the representation of the population at this point is shown in Fig.5 below.
-
3.
Chromosome adaptation calculation. Construct the fitness function f = z. Select the chromosome with the smaller adaptation in the search for the optimal chromosome.
-
4.
Selection. Adopting roulette wheel method to calculate the fitness of individuals, selecting individuals with excellent characteristics as parents for inheritance. The fitness of the offspring in inheritance is lower than that of the parents.
-
5.
Mutation. After several experiments, the probability of chromosome variation was chosen to be 0.05 based on the convergence of the model. For each individual in the parent population, a random number is generated. If this random number is less than the mutation probability, the individual will undergo mutation. The mutation principle is to discard the current processing facility and select another processing facility of the same level for replacement. The mutation process is shown in below.
-
6.
Crossover. Set the crossover probability to 0.7. If the random value of chromosome 1 and chromosome 2 is less than 0.7, the values on the corresponding positions of the two chromosomes are exchanged.
-
7.
Termination condition judgement. Set the number of iterations of the genetic algorithm to stop when the optimal solution is found. The iterations were plotted using Python based on the case data as shown in below. The model has converged when the number of iterations is 2500 and can be terminated to obtain the least cost solution.
Therefore, in this research, we choose a variance probability of 0.05, a crossover probability of 0.7 and a number of iterations of 2500(Fig. 6).
3.3.2 MILP solver
MILP (mixed integer linear programming) is one of many types of optimization problems: problems with equational or inequality constraints, decision variables that are continuous or integer variables, and objective functions and constraints that are linear to the decision variables.The general mathematical form of MILP is:
The modelling and solution of MILP incorporates a number of interesting algorithms, such as row generation/column generation algorithms for large-scale problems, branch-and-bound (B&B) methods for integer variables, cut-plane methods for reducing the feasible domain of linear relaxation problems, simplex and interior point methods for solving linear programming, and a range of preprocessing, branching, bounding and pruning strategy algorithms to improve the efficiency of B&B solutions. Although the full extent of optimization cannot be understood from these algorithms, they do cover the algorithmic ideas and strategies we use for most of our problems. It is possible to try to apply the solver to the process of solving our problems (Fig. 7).
This research uses Python's built-in PulP solver, a linear programming library for the Python programming language, which can be used to call external MIP solvers to solve MILP problems. PuLP has a simple and user-friendly interface, which makes linear programming modeling easy. In PuLP, users only need to define the objective function and constraints, and then the model can be solved through the internal functions of the PuLP library. Compared to genetic algorithms, its coding difficulty is lower.
3.3.3 Lingo solver
For the process of optimising the reverse logistics of medical waste recycling, the decision variables involved are the delivery volume of each treatment facility, the treatment volume and the 0–1 variable problem of whether or not to site each point. The objective function of the proposed solution is a mixed-integer linear programming problem. By introducing parameters such as the total amount of generated medical waste, distance, and unit transportation cost for each transportation route, a minimum-cost satisfactory solution can be obtained. Lingo Solver, the "Linear and general optimizer solver," can be used to solve linear programming problems and is a very powerful and suitable choice for solving optimization models.
The Lingo solver has over a dozen built-in internal functions that allow the decision variables to be integers (i.e. integer programming, including 0–1 integer programming), making it convenient and flexible, fast to solve, and allowing data interaction with databases such as Excel and Navicat. Problem solving using the Lingo solver can be carried out in two main steps as follows.
-
1
Identify the objectives and develop a mathematical model based on the medical waste recycling problem under study and use mathematical modelling methods to develop an optimization model.
-
2
Based on the optimization model, the Lingo model is used to build the solution model, transforming the mathematical modelling language into the Lingo computer language and solving the problem through autonomous computer learning.
The main advantages of the Lingo solution approach to solving are as follows.
-
Simple model representation: Lingo allows mathematical models to be expressed in simple formulas that are easy to understand and modify, making model building intuitive and easy to understand.
-
Data input, selection and export are more accurate; Lingo can obtain data directly from external data tables and Lingo can also export calculations directly to data carriers, making it easier to analyse optimization results accurately.
-
Autonomous learning capability. Based on the imported parameters and the model, Lingo automatically selects the most suitable method to solve the problem based on the data and the complexity of the model, without the need for independent selection.
-
Interactive model building is possible. The DLL and OLE functions in Lingo make it easier to use the Lingo terminal interactively with applications.
4 Case studies
4.1 Performance assessment
In order to be in a better position to distinguish between the different methods and to find the advantages of each method, several sets of examples with random values of different sizes were designed to test the performance of the models and methods. Six sets of parameters were designed for this problem and the data were classified into small-scale, medium-scale and large-scale problems based on their size. For each set of parameters, the parameters were generated by random number method according to the same criteria, except for the number of different facility sizes at each level. The random number method reflects the different sizes of waste recycling systems. The parameters for each group are shown in Tables 1 and 2 below.
Three methods were used to solve for each group of parameters, and the solution time and objective function value of each method for each group of parameters were recorded. Table 3 shows the summary information of the results using each of the three methods.
As shown in Table 3, the solution quality and solution speed embodied by the genetic algorithm is more stable across problems of different sizes; comparing the results obtained by the genetic algorithm with those obtained by the solver, although the cost is lower through the solver, all times are longer. And when the size of the data increases, the solver approach is likely to get stuck in a local optimum solution unable to obtain a global optimum solution.
4.2 Case description
Just to be in a position to demonstrate that the model in this research can be applied to practical medical waste reverse logistics optimization, but given that it was not possible to find an identical case to study at the moment, we took the case of **chang, Shaanxi Province, China, for the study and approximated the fit to some of the parameters involved. The data used are from those referred to by Xukun Z in his master's thesis(Xukun 2021).
After the simulation case study in the previous section, it was found that a more satisfactory solution could be obtained faster using genetic algorithm. We apply the more efficient genetic algorithm to the solution of our practical problem and analyze the results against the optimal solution obtained by the MILP solver. We set the number of iterations of the genetic algorithm to 2500, and after the corresponding number of iterations the model has converged at a faster rate and a relatively satisfactory solution has been obtained for the model.
The figures in Table 4 below show the construction costs as well as the operation and maintenance costs of the infrastructure. In this case, the construction costs of the recycling centre and the power plant are not taken into account as they are existing functional institutions that are not exclusively used for.
Recycling and treatment of clinical waste, while the rest of the construction and operation and maintenance costs are taken into account.
In this case, there are 13 fixed recycling centres, of which the coordinates of each centre are shown in Table 5, and the amount of medical waste generated by each centre during the one-year cycle is shown in Table 6.
The confirmation of the values of the remaining parameters, such as freight and handling charges, can be determined according to the local situation, and fixed values are not very informative.
4.3 Case results
In the case of this study, the specific parameters for the iterations performed by the genetic algorithm were a chromosome crossover variation rate of 0.7 and a variation probability of 0.1. The results obtained by the solution of the genetic algorithm and a comparison of the results are shown in Table 7 below.
Since in this case it is assumed that all recycling centres can be used as locations for other facilities in the recycling network, the relevant locations of all levels of facilities are the same as the coordinates of the recycling centres.
As a result of the calculations for the model, the final testing and processing centres are opened at recycling centres 1, 4, 6, 7 and 12; the reprocessing centres are opened at recycling centres 1 and 7; the landfill plant is opened at recycling centre 7; and the power plant is opened at recycling centre 1. The location of specific levels of facilities is shown in Table 8 below. According to the data source, the recycling network spent $2.67 million on waste disposal in that cycle, so the comparison shows that the model has a certain optimization effect. Analysis of its reduced optimization effect may be due to the lower accuracy of the data and the large difference in the amount of medical waste recycled at each recycling centre leading to poor iterative effects.
The analysis results show that the genetic algorithm can find a better solution when the scale of reverse logistics recycling is large, and the optimal solution obtained by the iteration of the algorithm can be approximated to be the global optimal solution, so the model is effective in solving the recycling problem of medical waste.
4.4 Discussion
In this study, we examine a reverse logistics network for medical waste with the aim of minimising total costs. The use of a three-tier recycling network for medical waste is more logical because it allows for dedicated management of medical waste and minimizes the costs incurred in the disposal of medical waste as well as maximising the utilization of residual costs. In the past, there has been more research into the recycling of healthcare waste that has considered direct landfill from recycling centres, with only a small number of studies considering the constraints of multiple treatment facilities on the recycling network. The model and network structure constructed in this study may have some positive impact on the relevant units.
5 Conclusion and outlook
5.1 Conclusion
The research in this paper hopes to provide more references to relevant organizations and functional departments by constructing a more reasonable model for medical waste. It is hoped that the problem can be solved more quickly in the face of the explosion of medical waste production. The work done in this research is to design a corresponding reverse logistics network structure for medical waste, construct a reverse logistics network model and solution algorithm with the objective of minimizing the total cost of medical waste recycling, and prove the feasibility of optimizing the model through computer simulation and case analysis.
-
(1)
This research constructs a three-tier medical waste reverse logistics optimization network, which includes five main recycling-related facilities: recycling centres, testing and treatment centres, reprocessing centres, landfill plants and power plants. This network structure can solve a series of problems that may arise in the process of medical waste recycling and treatment in a more efficient and professional manner. It prevents the accumulation of medical waste and its untimely disposal due to a small number of recycling facilities and a single recycling structure. And to a certain extent, it prevents the spread of diseases and recycling by unscrupulous traders due to the untimely collection of medical waste.
-
(2)
Through the calculation of various scale problems, the model was shown to be effective in optimising medical waste recycling networks of all levels. Stakeholders can refer to some of the observations in recycling problems at different levels such as county and municipal levels.
-
(3)
Using medical waste as an example, it is hoped that the network, which can be used directly or with simple adaptations to each level of the network facilities based on existing models when undertaking specialized recycling of other types of waste, will provide some design insights when looking at various types of waste networks..
5.2 Outlook
This research focuses on a series of problems arising from the uncertainty of the amount of medical waste generated, and the planning and study of the design of a reverse logistics recycling network capable of meeting the recycling volumes used in different scales. As the model design is more ideal, some idealised conditions are added to the model construction process, simplifying the setting of the relevant parameters, which may deviate from the actual, but also equally reducing the difficulty of the model and the solution, and improving the practicality of the model. This paper is still in the initial stage of research on the reverse logistics of medical waste, and further research is needed in the following work.
-
(1)
In addition to the amount of medical waste recycling, there are also uncertainties in the medical waste reverse logistics network such as transportation time and traffic conditions. By considering more uncertainties, we can improve the rationality of the network model and better help relevant enterprises to complete the construction and planning of infrastructure and transportation routes.
-
(2)
With the development of information technology, a variety of cutting-edge technologies, such as cloud management, are combined to build a medical waste reverse logistics network, design a corresponding management information system, strengthen the supervision and management of medical waste in the process of disposal in each link, and standardise the medical waste disposal process.
-
(3)
In this research, only the location and path planning of each node have been studied in the course of the study of medical waste reverse logistics network, but the treatment technology and process of each node for medical waste have not been discussed in detail. The next step will be to carry out research on specific medical waste reverse logistics and treatment methods according to the nature of medical waste, and to optimize the parameters related to the specific disposal process in the model.
Data Availability
The authors confirm that the data supporting the findings of this study are available within the article and references materials.
References
Abdulla F, Qdais HA, Rabi A (2008) Site investigation on medical waste management prac-tices in northern Jordan. Waste Manage 28:450–458
Moazzam Ali, Chushi Kuroiwa (2009) Status and challenges of hospital solid waste management: case studies from Thailand, Pakistan, and Mongolia[J]. J. Mater. Cycles Waste Manag. 11(3)
Maha Almuneef, Ziad A, Memish (2003) Effective medical waste management: It can be done[J]. AJIC: Am. J. Infect. Control 31(3)
U.S. EPA, 2012a. Medical Waste. Retrieved February 24, 2015, from: http://www.epa. gov/osw/nonhaz/industrial/medical/
Deok Ryun Kim,Mohammad Ali,Vu Dinh Thiem,**-Kyung Park,Lorenz von Seidlein,John Clemens. (2007) Geographic analysis of shigellosis in Vietnam[J]. Health and Place ,14(4)
Ghezavati VR, Beigi M (2016) Solving a bi-objective mathematical model for location-routing problem with time windows in multi-echelon reverse logistics using metaheuristic procedure[J]. J. Ind. Eng. Int. 12(4)
Hao Hao, Ji Zhang, Qian Zhang, Li Yao, Yichen Sun (2019), Improved gray neural network model for healthcare waste recycling forecasting[J]. J. Comb. Optim. 42(4)
Hashemi Seyed Emadedin. A fuzzy multi-objective optimization model for a sustainable reverse logistics network design of municipal waste-collecting considering the reduction of emissions [J]. Journal of Cleaner Production, 2021, 318.
He Zheng Gang, Liu Sha (2015) The Research on Recovery Network Optimization of Medical Waste[J]. Appl. Mech. Mater. 4002:768–768
Vadiati Meysam, Beynaghi Ali, Bhattacharya Prosun, Bandala Erick R, Mozafari Masoud (2021) Indirect effects of COVID-19 on the environment: How deep and how long?[J]. Sci. Total Environ. 810
E Insa, M Zamorano, R López (2010) Critical review of medical waste legislation in Spain[J]. Resources, Conservation & Recycling, 54(12)
Govindan Kannan, Nasr Arash Khalili, Mostafazadeh Parisa, Mina Hassan (2021) Medical waste management during coronavirus disease 2019 (COVID-19) outbreak: A mathematical programming model.[J]. Comput Ind Eng, 162
Saeed Kargar, Mohammad Mahdi Paydar, Abdul Sattar Safaei (2020) A reverse supply chain for medical waste: A case study in Babol healthcare sector[J]. Waste Manag. 113(C)
Gerasimos Mantzaras, Evangelos A, Voudrias (2017) An optimization model for collection, haul, transfer, treatment and disposal of infectious medical waste: Application to a Greek region[J]. Waste Manag. 69
Mato RRAM, Kaseva ME (1999) Critical review of industrial and medical waste prac-tices in Dar es Salaam City. Resour Conserv Recycl 25:271–287
Qingmin Meng, ** Chen, Changsheng Bu, Jiliang Ma (2012) Experimental study on the controlled air oxidation of sawdust in a packed-bed reactor[J]. Korean J Chem Eng KOREAN J CHEM ENG. 29(4)
Mohee R (2005) Medical wastes characterisation in healthcare institutions in Mauritius. Waste Manage 25:575–581
Ali Mustafa, Geng Yong (2018) Accounting embodied economic potential of healthcare waste recycling-a case study from Pakistan.[J]. Environ. Monit. Assess. 190(11)
Gao Jia**g, Li Haolin, Wu **gwen, Lyu Junyan, Tan Zheyi, ** Zhufan (2021) Routing Optimisation of Urban Medical Waste Recycling Network considering Differentiated Collection Strategy and Time Windows [J]. SCIENTIFIC PROGRAMMING, 2021
Chakraborty Sayanta, Saha Apu Kumar (2022) A framework of LR fuzzy AHP and fuzzy WASPAS for health care waste recycling technology[J]. Appl. Soft Comput. 127
Shi L, Fan H, Gao P, et al (2009) Network model and optimization of medical waste reverse logistics by improved genetic algorithm[C]. International symposium on intelligence computation and applications. Springer, Berlin, Heidelberg 40–52
Stock J R. (1998) Development and implementation of reverse logistics programs.[C]. ANNUAL CONFERENCE PROCEEDINGS, COUNCIL OF LOGISTICS MANAGEMENT
Chenglei Sun. (2020) Research on the Recycling of Hazardous Medical Waste[J]. IOP Conference Series: Environ. Earth Sci. 514(3)
Taghipour H, Mosaferi M (2009) Characterization of medical waste from hospital in Tabriz. Iran Sci Total Environ 407:1527–1535
Tirkolaee EB, Abbasian P, Weber GW Sustainable fuzzy multi-trip location-routing problem for medical waste management during the COVID-19 outbreak. Sci. Total Environ. 756 143607 Article
Tirkolaee EB, Goli A, Ghasemi P, Goodarzian F, Designing a sustainable closed-loop supply chain network of face masks during the COVID-19 pandemic:Pareto-based algorithms. J. Clean. Prod. 333, Article 130056
Tudor TL (2007) Towards the development of a standardized measurement unit for healthcare waste generation. Resour Conserv Recycl 50:319–333
Tudor TL, Barr SW, Gilg AW (2007) Linking intended behaviour and actions: a case study of healthcare waste management in the Cornwall NHS. Resour Conserv Recycl 51:1–23
Jaber Valizadeh, Peyman Mozafari (2021) A novel cooperative model in the collection of infectious waste in COVID-19 pandemic[J]. J. Model. Manag. 17(1)
Wang Q, Huang QF, Yan HAI, Li L (2013) The current situation and suggestions of hazardous waste management in China [J]. J Environ Eng 3(01):1–5
Zhang Wanting, Zeng Ming, Guo Peng, Wen Kun (2022) Variable Neighborhood Search for Multi-Cycle Medical Waste Recycling Vehicle Routing Problem with Time Windows[J]. International Int. J. Environ. Res. Public Health INT J ENV RES PUB HE 19(19)
Elliott Steen Windfeld, Marianne Su-Ling Brooks. (2015) Medical waste management – A review[J]. J. Environ. Manage. 163
Xu **aofeng,Wei Zhifei. Dynamic pickup and delivery problem with transshipments and LIFO constraints [J]. Computers & Industrial Engineering, 2023, 175.
Xu **aofeng, Wang Chenglong, Zhou Peng (2021) GVRP considered oil-gas recovery in refined oil distribution: from an environmental perspective [J]. Int. J. Prod. Econ. 235(prepublish)
Xu **aofeng,Lin Ziru,Li **ang,Shang Chang**g,Shen Qiang. Multi-objective robust optimisation model for MDVRPLS in refined oil distribution [J]. International Journal of Production Research,2022, 60(22).
Xu **aofeng,Liu Wenzhi,Yu Lean. Trajectory prediction for heterogeneous traffic-agents using knowledge correction data-driven model [J]. Information Sciences, 2022, 608.
**n L, ** C, Sagir M, Wenbo Z (2023) How can infectious medical waste be forecasted and transported during the COVID-19 pandemic? A hybrid two-stage method. Technol Forecast Soc Change, 187
Zhang Xukun. Research on the design of reverse logistics network for medical waste in small and medium-sized cities [D]. Tian** University of Technology, 2021.000384.
Yu H, Sun X, Solvang WD et al (2020) Reverse logistics network design for effective management of medical waste in epidemic outbreaks: Insights from the coronavirus disease 2019 (COVID-19) outbreak in Wuhan (China)[J]. Int J Environ Res Public Health 17(5):1770
Mohsen Zamani,Mahdi Abolghasemi,Seyed Mohammad Seyed Hosseini,Mir Saman Pishvaee. Considering pricing and uncertainty in designing a reverse logistics network[J]. International Journal of Industrial and Systems Engineering,2020, 35(2).
Manuel A, Zambrano-Monserrate, María Alejandra Ruano, Luis Sanchez-Alcalde (2020) Indirect effects of COVID-19 on the environment[J]. Sci. Total Environ. 728(prepublish)
Zhifang Zhou, Yanfei Cai, Yixuan **ao, **aohong Chen, Huixiang Zeng (2018) The optimization of reverse logistics cost based on value flow analysis – a case study on automobile recycling company in China [J]. J. Intell. Fuzzy Syst. 34(2)
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Qi, P., Wang, Y. & Lin, ·. Optimization of reverse logistics network for medical waste recycling. J. of Data, Inf. and Manag. 5, 71–88 (2023). https://doi.org/10.1007/s42488-023-00090-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42488-023-00090-0