Abstract
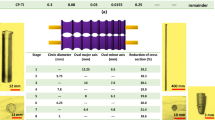
In this study, different conditions of sandblasting on dental implant fixtures were investigated to achieve the best sandblasting conditions. 18 different sandblasting conditions (Using 152 implant fixture samples) were examined, including parameters such as particle size, particle blasting pressure, and particle blasting angle. The surface treatment of the samples was performed using the SLA + Anodizing method. AFM testing was performed for each of the 18 different states, and the average surface roughness of each of these was compared with each other. Then, a bone layer was placed on the sample with the closest average surface roughness to the standard and the least amount of aluminum oxide on its surface among the 18 different states, to confirm the accuracy and quality of the desired surface roughness by examining the bone formation process and speed. The results showed that state No. 4 (sandblast particle size: 75 µm, spraying pressure of sandblast particles: 4 bar, sandblast particle spraying angle: 30 degrees), which was prepared using the SLA + Anodizing method and had a surface roughness of 1.989 µm (The percentage of Al2O3 on the surface = 6%), had the best sandblasting conditions and showed 95% cell viability and accelerated the treatment and bone formation process for about a week. The simulation results, using Abaqus software, indicated that the stress distribution on the surface of the implant fixture in contact with the bone surface has increased by approximately 4.3% for state No. 4. This will help prevent loosening of the dental implant fixture over time.





















Similar content being viewed by others
Availability of data and materials
The authors confirm that the data supporting the findings of this study are available within the article and/or its supplementary materials as requested.
Abbreviations
- SLA:
-
Sandblasted large grit acid etched
- SLA + Anodizing:
-
Sandblasted large grit acid etched + anodizing
- AFM:
-
Atomic force microscope
- EDAX:
-
Energy dispersive analysis X-ray
- MTT:
-
Molecular cytotoxicity test
- FESEM:
-
Field emission scanning electron microscopy
References
Mohammadi, B., Abdoli, Z., & Anbarzadeh, E. (2021). Investigation of the effect of abutment angle tolerance on the stress created in the fixture and screw in dental implants using finite element analysis. Journal of Biomimetics, Biomaterials and Biomedical Engineering, 51, 63–76. https://doi.org/10.4028/www.scientific.net/JBBBE.51.63
Pedrinaci, I., Sun, T. C., Sanz-Alonso, M., Sanz-Esporrin, J., Hamilton, A., & Gallucci, G. O. (2023). Implant survival in the anterior mandible: A retrospective cohort study. Clinical Oral Implants Research, 34(5), 463–474. https://doi.org/10.1111/clr.14052
Awaja, F., Bax, D. V., Zhang, S., James, N., & McKenzie, D. R. (2012). Cell adhesion to PEEK treated by plasma immersion ion implantation and deposition for active medical implants. Plasma Processes and Polymers, 9(4), 355–362. https://doi.org/10.1002/ppap.201100034
Kowar, J., Lund, H., & Stenport, V. F. (2023). Long-term performance of implants with moderately rough anodized surface supporting single-tooth restorations: A retrospective analysis with an up to 15-year follow-up. Clinical Oral Implants Research, 34(4), 367–377. https://doi.org/10.1111/clr.14048
Kruse, H. V., Lewin, W. T., Suchowerska, N., Al Maruf, D. A., Cheng, K., Clark, J. R., & McKenzie, D. R. (2022). Plasma immersion ion-implanted 3D-printed PEEK bone implants: In vivo sheep study shows strong osseointegration. Plasma Processes and Polymers, 19(7), 2100244. https://doi.org/10.1002/ppap.202100244
Garabetyan, J., Malet, J., Kerner, S., Detzen, L., Carra, M. C., & Bouchard, P. (2019). The relationship between dental implant papilla and dental implant mucosa around single-tooth implant in the esthetic area: A retrospective study. Clinical Oral Implants Research, 30(12), 1229–1237. https://doi.org/10.1111/clr.13536
Van Oirschot, B. A., Zhang, Y., Alghamdi, H. S., Cordeiro, J. M., Nagay, B. E., Barao, V. A., et al. (2022). Surface engineering for dental implantology: favoring tissue responses along the implant. Tissue Engineering Part A, 28(11–12), 555–572. https://doi.org/10.1089/ten.tea.2021.0230
Mamalis, A. A., & Silvestros, S. S. (2011). Analysis of osteoblastic gene expression in the early human mesenchymal cell response to a chemically modified implant surface: An in vitro study. Clinical Oral Implants Research, 22(5), 530–537. https://doi.org/10.1111/j.1600-0501.2010.02049.x
Abu Kasim, N. A., Nor, N. H. M., Ismail, M. H., & Saedon, J. (2017). Development of porous Ti-6Al-4V dental implant by metal injection molding with palm stearin binder system. Materials Science Forum, 889, 79–83. https://doi.org/10.4028/www.scientific.net/MSF.889.79
Buser, D., Von Arx, T., Ten Bruggenkate, C., & Weingart, D. (2000). Basic surgical principles with ITI implants Note. Clinical Oral Implants Research: Chapter, 3(11), 59–68. https://doi.org/10.1034/j.1600-0501.2000.011S1059.x
Cochran, D. L., Buser, D., Ten Bruggenkate, C. M., Weingart, D., Taylor, T. M., & Bernard, J. P., et al. (2002). The use of reduced healing times on ITI® implants with a sandblasted and acid‐etched (SLA) surface: Early results from clinical trials on ITI® SLA implants. Clinical Oral Implants Research, 13(2), 144–153. https://doi.org/10.1034/j.1600-0501.2002.130204.x
Le Guehennec, L., Goyenvalle, E., Aguado, E., Pilet, P., Spaethe, R., & Daculsi, G. (2007). Influence of calcium chloride and aprotinin in the in vivo biological performance of a composite combining biphasic calcium phosphate granules and fibrin sealant. Journal of Materials Science: Materials in Medicine, 18, 1489–1495. https://doi.org/10.1007/s10856-006-0086-x
Rosa, M. B., Albrektsson, T., Francischone, C. E., & Wennerberg, A. (2013). Micrometric characterization of the implant surfaces from the five largest companies in Brazil, the second largest worldwide implant market. International Journal of Oral & Maxillofacial Implants. https://doi.org/10.11607/jomi.2791
De Bruyn, H., Christiaens, V., Doornewaard, R., Jacobsson, M., Cosyn, J., Jacquet, W., & Vervaeke, S. (2017). Implant surface roughness and patient factors on long‐term peri‐implant bone loss. Periodontology 2000, 73(1), 218–227. https://doi.org/10.1111/prd.12177
Hao, C. P., Cao, N. J., Zhu, Y. H., & Wang, W. (2021). The osseointegration and stability of dental implants with different surface treatments in animal models: A network meta-analysis. Scientific Reports, 11(1), 13849. https://doi.org/10.1038/s41598-021-93307-4
Zhang, Y., Li, S., Lin, Y., Di, P., & Liu, Y. (2023). Macro to micro: Surface modification of titanium dental implants. In Surface Modification of Titanium Dental Implants. https://doi.org/10.1007/978-3-031-21565-0_3
Croitoru, S. M., & Inţă, M. (2019). Study on shape of dental implants. In Advanced Engineering Forum, 34, 183–188.
Almassri, H. N., Ma, Y., Dan, Z., Ting, Z., Cheng, Y., & Wu, X. (2020). Implant stability and survival rates of a hydrophilic versus a conventional sandblasted, acid-etched implant surface: Systematic review and meta-analysis. The Journal of the American Dental Association, 151(6), 444–453. https://doi.org/10.1016/j.adaj.2020.03.002
Savadi, R. C., Agarwal, J., Agarwal, R. S., & Rangarajan, V. (2011). Influence of implant surface topography and loading condition on stress distribution in bone around implants: A comparative 3D FEA. The Journal of Indian Prosthodontic Society, 11, 221–231. https://doi.org/10.1007/s13191-011-0105-6
Kunrath, M. F., Muradás, T. C., Penha, N., & Campos, M. M. (2021). Innovative surfaces and alloys for dental implants: What about biointerface-safety concerns? Dental Materials, 37(10), 1447–1462. https://doi.org/10.1016/j.dental.2021.08.008
Rasouli, R., Barhoum, A., & Uludag, H. (2018). A review of nanostructured surfaces and materials for dental implants: Surface coating, patterning and functionalization for improved performance. Biomaterials science, 6(6), 1312–1338. https://doi.org/10.1039/C8BM00021B
Alécio, A. B. W., Ferreira, C. F., Babu, J., Shokuhfar, T., Jo, S., Magini, R., & Garcia-Godoy, F. (2019). Doxycycline release of dental implants with nanotube surface, coated with poly lactic-co-glycolic acid for extended pH-controlled drug delivery. Journal of Oral Implantology, 45(4), 267–273. https://doi.org/10.1563/aaid-joi-D-18-00069
Koo, K. T., Khoury, F., Keeve, P. L., Schwarz, F., Ramanauskaite, A., Sculean, A., & Romanos, G. (2019). Implant surface decontamination by surgical treatment of periimplantitis: A literature review. Implant dentistry, 28(2), 173–176. https://doi.org/10.1097/ID.0000000000000840
Mohammadi, B., & Anbarzadeh, E. (2022). Evaluation of viability and cell proliferation in bone and gingival on dental implant fixtures with active sandblasted and sandblasted surfaces by the cytotoxicity test method. In Journal of Biomimetics, Biomaterials and Biomedical Engineering, 56, 165–172. https://doi.org/10.4028/p-gmmc8m
Song, Y. W., Park, J. Y., Jung, J. Y., Kim, J. N., Hu, K. S., & Lee, J. S. (2023). Does the fixture thread depth affect the accuracy of implant placement during fully guided immediate implant placement? A human cadaver study. Clinical Oral Implants Research, 34(2), 116–126. https://doi.org/10.1111/clr.14023
Costa-Berenguer, X., García-García, M., Sánchez-Torres, A., Sanz-Alonso, M., Figueiredo, R., & Valmaseda-Castellón, E. (2018). Effect of implantoplasty on fracture resistance and surface roughness of standard diameter dental implants. Clinical Oral Implants Research, 29(1), 46–54. https://doi.org/10.1111/clr.13037
Bahrami, B., Shahrbaf, S., Mirzakouchaki, B., Ghalichi, F., Ashtiani, M., & Martin, N. (2014). Effect of surface treatment on stress distribution in immediately loaded dental implants—A 3D finite element analysis. Dental Materials, 30(4), 89–97. https://doi.org/10.1016/j.dental.2014.01.012
Bok, W. M., Kim, S. Y., Lee, S. J., Shin, G. S., Park, J. M., & Lee, M. H. (2015). Surface characteristics and bioactivation of sandblasted and acid-etched (SLA) Ti-10Nb-10Ta alloy for dental implant. International Journal of Precision Engineering and Manufacturing, 16, 2185–2192. https://doi.org/10.1007/s12541-015-0281-0
Barrak, F., Li, S., Muntane, A., Bhatia, M., Crossthwaite, K., & Jones, J. (2022). Particle release from dental implants immediately after placement—An ex vivo comparison of different implant systems. Dental Materials, 38(6), 1004–1014. https://doi.org/10.1016/j.dental.2022.04.003
El-Hadad, S., Safwat, E. M., & Sharaf, N. F. (2018). In-vitro and in-vivo, cytotoxicity evaluation of cast functionally graded biomaterials for dental implantology. Materials Science and Engineering: C, 93, 987–995. https://doi.org/10.1016/j.msec.2018.09.003
Ganeles, J., Zöllner, A., Jackowski, J., Ten Bruggenkate, C., Beagle, J., & Guerra, F. (2008). Immediate and early loading of Straumann implants with a chemically modified surface (SLActive) in the posterior mandible and maxilla: 1-year results from a prospective multicenter study. Clinical Oral Implants Research, 19(11), 1119–1128. https://doi.org/10.1111/j.1600-0501.2008.01626.x
Junior, J. F. S., Verri, F. R., de Faria Almeida, D. A., de Souza Batista, V. E., Lemos, C. A. A., & Pellizzer, E. P. (2016). Finite element analysis on influence of implant surface treatments, connection and bone types. Materials Science and Engineering: C, 63, 292–300. https://doi.org/10.1016/j.msec.2016.02.061
Li, J. D., Qin, W., Lartey, P. O., Fu, Y. L., & Ma, J. (2023). Hydrothermal desulfurization on porous sulfonated CFR-PEEK surface structure used for implant application. Journal of Bionic Engineering, 20, 748–761. https://doi.org/10.1007/s42235-022-00276-z
Zhang, H. L., Li, D. K., Huang, J. X., Guo, Z. G., & Liu, W. M. (2023). Advance in structural classification and stability study of superamphiphobic surfaces. Journal of Bionic Engineering, 20, 366–389. https://doi.org/10.1007/s42235-022-00270-5
Acknowledgements
The authors thank Dorin Kasht Mana Company, the largest manufacturer of dental implant systems in Iran, and especially Dr. Ali Asgar Malek Altojjari, the founder of the company, for their support and for providing the information and guidance of the brand 3A.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest regarding the manuscript. There is no financial or personal relationship that could have influenced the presented work, and the research is original and has not been submitted or published elsewhere.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Anbarzadeh, E., Mohammadi, B. Improving the Surface Roughness of Dental Implant Fixture by Considering the Size, Angle and Spraying Pressure of Sandblast Particles. J Bionic Eng 21, 303–324 (2024). https://doi.org/10.1007/s42235-023-00422-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42235-023-00422-1