Abstract
Purpose
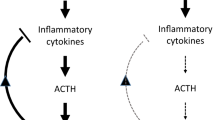
Alpha-melanocyte-stimulating hormone (alpha-MSH) has proven cardiovascular effects and plays a significant role as an endogenous countermeasure to ischemia-reperfusion injury. The aim of the current study was to examine the response of alpha-MSH during exercise in patients diagnosed with coronary artery disease (CAD) and evaluate its value in the assessment of severity and prognosis.
Methods
Forty subjects with documented CAD (i.e., lesions on coronary angiography ≥ 50%) were included. Cardiopulmonary exercise testing (CPET) on a treadmill (TM) and recumbent ergometer (RE) were performed on two visits, 2–4 days apart, during 2 months of coronary angiography; subsequently, the subjects were followed up for 32 ± 10 months. At rest, at peak CPET, and after 3 min of recovery, plasma levels of alpha-MSH were measured by enzyme-linked immunosorbent assay technique.
Results
Mean ejection fraction was 56.7 ± 9.6%. Alpha-MSH similarly increased from rest to peak CPET on both modalities. There were no significant differences in alpha-MSH values during testing in patients with 1,2- and 3-vesel CAD, nor in patients with a SYNTAX score </≥ 23 (p > 0.05). Among CPET and hormonal parameters, ∆alpha-MSH recovery/peak during RE CPET was the best predictor of cardiac event occurrence (chi-square 6.67, HR = 0.51, CI = 0.25–1.02, p = 0.010).
Conclusion
∆alpha-MSH recovery/peak during RE CPET has predictive value for CAD prognosis, demonstrating involvement of alpha-MSH in CAD and a link between stress hormones and cardiac events.
Similar content being viewed by others
Abbreviations
- CABG:
-
Coronary artery bypass graft
- CAD:
-
Coronary artery disease
- CPET:
-
Cardiopulmonary exercise test
- EF:
-
Left ventricular ejection fraction,
- HR:
-
Heart rate
- MI:
-
Myocardial infarction
- MSH:
-
Melanocyte-stimulating hormone
- SCA:
-
Number of stenotic coronary arteries
- O2 pulse:
-
Oxygen pulse
- PCI:
-
Percutaneous coronary intervention
- RE:
-
Recumbent ergometer
- RER:
-
Respiratory exchange ratio
- VCO2 :
-
Carbon dioxide output
- VE:
-
Ventilation
- VO2 :
-
Oxygen consumption
- ∆VO2/∆WR:
-
Work efficiency
- WR:
-
Work rate
References
Dutia R, Meece K, Dighe S, Kim AJ, Wardlaw SL (2012) β-Endorphin antagonizes the effects of α-MSH on food intake and body weight. Endocrinology. 153(9):4246–4255. https://doi.org/10.1210/en.2012-1166
Vecsernyes M, Szokol M, Bombicz M et al (2017) Alpha-melanocyte-stimulating hormone induces vasodilation and exerts cardioprotection through the heme-oxygenase pathway in rat hearts. J Cardiovasc Pharmacol 69(5):286–297. https://doi.org/10.1097/FJC.0000000000000472
Rinne P, Tikka S, Makela S et al (2012) Hemodynamic actions and mechanisms of systemically administered alpha-MSH analogs in mice. Peptides. 38:150–158
Catania A, Airaghi L, Garofalo L, Cutuli M, Lipton JM (1998) The neuropeptide alpha-MSH in HIV infection and other disorders in humans. Ann N Y Acad Sci 840:848–856. https://doi.org/10.1111/j.1749-6632.1998.tb09622.x
Catania A, Lipton JM (1994) The neuropeptide alpha-melanocyte-stimulating hormone: a key component of neuroimmunomodulation. Neuroimmunomodulation. 1(2):93–99. https://doi.org/10.1159/000097096
Vecsernyes M, Juhasz B, Der P et al (2003) The administration of alphamelanocyte-stimulating hormone protects the ischemic/reperfused myocardium. Eur J Pharmacol 470:177–183
Getting SJ, Di Filippo C, Christian HC et al (2004) MC-3 receptor and the inflammatory mechanisms activated in acute myocardial infarct. J Leukoc Biol 76(4):845–853. https://doi.org/10.1189/jlb.0306175
Airaghi L, Lettino M, Manfredi MG, Lipton JM, Catania A (1995) Endogenous cytokine antagonists during myocardial ischemia and thrombolytic therapy. Am Heart J 130(2):204–211. https://doi.org/10.1016/0002-8703(95)90430-1
Ottani A, Giuliani D, Neri L et al (2015) NDP-α-MSH attenuates heart and liver responses to myocardial reperfusion via the vagus nerve and JAK/ERK/STAT signaling. Eur J Pharmacol 769:22–32. https://doi.org/10.1016/j.ejphar.2015.10.022
Colombo G, Gatti S, Turcatti F et al (2005) Gene expression profiling reveals multiple protective influences of the peptide alpha-melanocyte-stimulating hormone in experimental heart transplantation. J Immunol 175(5):3391–3401. https://doi.org/10.4049/jimmunol.175.5.3391
American Thoracic Society; American College of Chest Physicians. ATS/ACCP Statement on cardiopulmonary exercise testing. Am J Respir Crit Care Med 2003; 167(2):211-277.
Belardinelli R, Lacalaprice F, Carle F, Minnucci A, Cianci G, Perna GP, D’Eusanio G (2003) Exercised-induced myocardial ischaemia detected by cardiopulmonary exercise testing. Eur Heart J 24:1304–1313
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, Lancellotti P, Muraru D, Picard MH, Rietzschel ER, Rudski L, Spencer KT, Tsang W, Voigt JU (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 16(3):233–270
Scanlon PJ, Faxon DP, Audet AM et al (1999) ACC/AHA guidelines for coronary angiography. A report of the American College of Cardiology/American Heart Association Task Force on practice guidelines (Committee on Coronary Angiography). Developed in collaboration with the Society for Cardiac Angiography and Interventions. J Am Coll Cardiol 33(6):1756–1824. https://doi.org/10.1016/s0735-1097(99)00126-6
Sianos G, Morel MA, Kappetein AP et al (2005) The SYNTAX Score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention. 1(2):219–227
Lightman SL (2008) The neuroendocrinology of stress: a never ending story. J Neuroendocrinol 20(6):880–884. https://doi.org/10.1111/j.1365-2826.2008.01711.x
Schnohr P, Marott JL, Kristensen TS et al (2015) Ranking of psychosocial and traditional risk factors by importance for coronary heart disease: the Copenhagen City Heart Study. Eur Heart J 36(22):1385–1393. https://doi.org/10.1093/eurheartj/ehv027
Nijm J, Kristenson M, Olsson AG, Jonasson L (2007) Impaired cortisol response to acute stressors in patients with coronary disease. Implications for inflammatory activity. J Intern Med 262(3):375–384. https://doi.org/10.1111/j.1365-2796.2007.01817.x
Popovic D, Damjanovic S, Djordjevic T et al (2017) Stress hormones at rest and following exercise testing predict coronary artery disease severity and outcome. Stress. 20(5):523–531. https://doi.org/10.1080/10253890.2017.1368488
Kotsis V, Nilsson P, Grassi G et al (2015) New developments in the pathogenesis of obesity-induced hypertension. J Hypertens 33(8):1499–1508. https://doi.org/10.1097/HJH.0000000000000645
Duclos M, Gouarne C, Bonnemaison D. Acute and chronic effects of exercise on tissue sensitivity to glucocorticoids. J Appl Physiol (1985). 2003;94(3):869–875. doi:10.1152/japplphysiol.00108.2002
Thompson DL Jr, Valencia NA, Walker NL, Oberhaus EL (2019) Melanocyte-stimulating hormone response to exercise, twitching, epinephrine injection, substance P injection, and prostaglandin-F2α administration in mares. J Equine Vet Sci 77:114–120. https://doi.org/10.1016/j.jevs.2019.03.002
Hiramoto K, Kobayashi H, Sekiyama A (2013) F Sato E, Tsuruta D, Ishii M. Mild exercise suppresses exacerbation of dermatitis by increasing cleavage of the β-endorphin from proopiomelanocortin in NC/Nga mice. J Clin Biochem Nutr 52(1):58–63. https://doi.org/10.3164/jcbn.12-51
Popovic D, Guazzi M, Jakovljevic DG et al (2019) Quantification of coronary artery disease using different modalities of cardiopulmonary exercise testing. Int J Cardiol 285:11–13. https://doi.org/10.1016/j.ijcard.2019.03.012
Korzeniewski B, Rossiter HB (2015) Each-step activation of oxidative phosphorylation is necessary to explain muscle metabolic kinetic responses to exercise and recovery in humans. J Physiol 593(24):5255–5268
Hoshi RA, Vanderlei LC, de Godoy MF, Bastos FD, Netto J Jr, Pastre CM (2016) Temporal sequence of recovery-related events following maximal exercise assessed by heart rate variability and blood lactate concentration. Clin Physiol Funct Imaging. https://doi.org/10.1111/cpf.12339 [Epub ahead of print]
Popovic D, Martic D, Djordjevic T et al (2017) Oxygen consumption and carbon-dioxide recovery kinetics in the prediction of coronary artery disease severity and outcome. Int J Cardiol 248:39–45. https://doi.org/10.1016/j.ijcard.2017.06.107
Kravchychyn ACP, Campos RMDS, Corgosinho FC et al (2018) The long-term impact of high levels of alpha-melanocyte-stimulating hormone in energy balance among obese adolescents. Ann Nutr Metab 72(4):279–286. https://doi.org/10.1159/000488005
Fletcher GF, Ades PA, Kligfield P, Arena R, Balady GJ, Bittner VA, Coke LA, Fleg JL, Forman DE, Gerber TC, Gulati M, Madan K, Rhodes J, Thompson PD, Williams MA; on behalf of the American Heart Association Exercise, Cardiac Rehabilitation, and Prevention Committee of the Council on Clinical Cardiology, Council on Nutrition, Physical Activity and Metabolism, Council on Cardiovascular and Stroke Nursing, and Council on Epidemiology and Prevention. Exercise standards for testing and training: a scientific statement from the American Heart Association. Circulation 2013;128:873–934.
Funding
The study is supported by Projects Number iii 41022 and 175036 Ministry of Education, Science and Technological Development.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The publication of this manuscript has been approved by all coauthors and responsible authorities from the University Clinical Center Serbia where the work has been carried out. The local Ethical Committee approved the study.
Informed consent
All participants provided written informed consent for participation in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vidojevic, D., Seman, S., Lasica, R. et al. Alpha-melanocyte-stimulating hormone during exercise recovery has prognostic value for coronary artery disease. Hormones 20, 381–387 (2021). https://doi.org/10.1007/s42000-020-00270-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42000-020-00270-2