Abstract
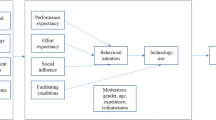
The CloudIoT paradigm has profoundly transformed the healthcare industry, providing outstanding innovation and practical applications. However, despite its many advantages, the adoption of this paradigm in healthcare settings remains limited. There is a lack of comprehensive understanding of the factors that ensure successful implementation. To address this issue, we have used the Analytic Hierarchy Process to prioritize 26 factors that could potentially influence the adoption of CloudIoT-based healthcare. These factors were derived from existing literature and categorized into four main groups: personal-specific, technology-specific, environment-specific, and organization-specific factors. Our findings revealed that performance expectancy, trust, facilitating conditions, task complexity, and perceived security are the top five critical factors influencing CloudIoT-based healthcare adoption. Interestingly, our results indicated that environmental factors were less influential than those in the other categories, with personal, technological, and organizational factors dominating the top ten significant factors. The insights from this study can help policymakers, CloudIoT service providers, healthcare providers, designers, and developers better understand the factors contributing to the successful implementation of CloudIoT-based healthcare. This understanding can guide decision-making and inform the development of strategies to promote the broader adoption of this innovative technology.



Similar content being viewed by others
References
Mutlag AA, Abd Ghani MK, al Arunkumar N, Mohammed MA, Mohd O (2019) Enabling technologies for fog computing in healthcare IoT systems. Future Gener Comput Syst 90:62–78
Thilakarathne NN, Kagita MK, Gadekallu TR, Maddikunta PKR (2020) The adoption of ict powered healthcare technologies towards managing global pandemics. ar**v Prepr. ar**v:2009.05716
A. Higher H. C. of J. Hiasat (2019) The Hashemite Kingdom of Jordan The Higher Health Council. World Health Organisation, p 109
Madae S, Adeinat M (2018) The health sector in Jordan: effectiveness and efficiency. Mod Appl Sci 12(12):234. https://doi.org/10.5539/mas.v12n12p234
Shah JL, Bhat HF, Khan AI (2021) Integration of cloud and IoT for smart e-healthcare. In: Healthcare paradigms in the internet of things ecosystem. Elsevier, pp 101–136
Uncovska M, Freitag B, Meister S, Fehring L (2023) Patient acceptance of prescribed and fully reimbursed mHealth Apps in Germany: an UTAUT2-based online survey study. J Med Syst 47(1):14
Bahbouh NM, Compte SS, Valdes JV, Sen AAA (2023) An empirical investigation into the altering health perspectives in the internet of health things. Int J Inf Technol 15(1):67–77
Meri A et al (2019) Modelling the utilization of cloud health information systems in the Iraqi public healthcare sector. Telemat Inform 36:132–146
Aceto G, Persico V, Pescapé A (2020) Industry 4.0 and health: internet of things, big data, and cloud computing. J Ind Inf Integr 18:100129. https://doi.org/10.1016/j.jii.2020.100129
Darwish A, Hassanien AE, Elhoseny M, Sangaiah AK, Muhammad K (2019) The impact of the hybrid platform of internet of things and cloud computing on healthcare systems: opportunities, challenges, and open problems. J Ambient Intell Humaniz Comput 10(10):4151–4166. https://doi.org/10.1007/s12652-017-0659-1
Kumar A, Krishnamurthi R, Nayyar A, Sharma K, Grover V, Hossain E (2020) A novel smart healthcare design, simulation, and implementation using healthcare 4.0 processes. IEEE Access 8:118433–118471
Fox GC, Kamburugamuve S, Hartman RD (2012) Architecture and measured characteristics of a cloud based internet of things. In: 2012 international conference on Collaboration Technologies and Systems (CTS). IEEE, pp 6–12
Shah JL, Bhat HF, Khan AI (2022) CloudIoT‐driven healthcare: review, architecture, security implications, and open research issues. In: Adv. Healthc. Syst. Empower. Physicians with IoT‐Enabled Technol., pp 173–253
Altawaiha I, Atan R, Yaakob RB, Abdullah RBHJ, Sneesl R (2022) CloudIoT-based healthcare adoption by healthcare professionals: a conceptual model. J Theor Appl Inf Technol 100(23):1–19
Shah STU, Yar H, Khan I, Ikram M, Khan H (2019) Internet of things-based healthcare: recent advances and challenges. In: Appl. Intell. Technol. Healthc., pp 153–162
Ramalho F, Neto A, Santos K, Agoulmine N (2015) Enhancing ehealth smart applications: a fog-enabled approach. In: 2015 17th international conference on E-health networking, application & services (HealthCom). IEEE, pp 323–328
Belli L, Cirani S, Davoli L, Melegari L, Mónton M, Picone M (2015) An open-source cloud architecture for big stream IoT applications. In: Interoperability and open-source solutions for the internet of things. Springer, pp 73–88
Ahmid M, Kazar O (2021) A cloud-IoT health monitoring system based on smart agent for cardiovascular patients. In: 2021 International Conference on Information Technology (ICIT). IEEE, pp 1–6
Kamalam GK, Anitha S (2022) Cloud‐IoT secured prediction system for processing and analysis of healthcare data using machine learning techniques. In: Adv. Healthc. Syst. Empower. Physicians with IoT‐Enabled Technol., pp 137–172
Nancy AA, Ravindran D, Raj-Vincent PMD, Srinivasan K, Gutierrez-Reina D (2022) IoT-cloud-based smart healthcare monitoring system for heart disease prediction via deep learning. Electronics 11(15):2292
Nilashi M, Ahmadi H, Ahani A, Ibrahim O, Almaee A (2015) Evaluating the factors affecting adoption of hospital information system using analytic hierarchy process. J Soft Comput Decis Support Syst 3(1):8–35
Pal D, Papasratorn B, Chutimaskul W, Funilkul S (2019) Embracing the smart-home revolution in Asia by the elderly: an end-user negative perception modeling. IEEE Access 7:38535–38549
Zhang X, Han X, Dang Y, Meng F, Guo X, Lin J (2017) User acceptance of mobile health services from users’ perspectives: the role of self-efficacy and response-efficacy in technology acceptance. Informat Health Soc Care 42(2):194–206. https://doi.org/10.1080/17538157.2016.1200053
Shahbaz M, Gao C, Zhai LL, Shahzad F, Hu Y (2019) Investigating the adoption of big data analytics in healthcare: the moderating role of resistance to change. J Big Data. https://doi.org/10.1186/s40537-019-0170-y
Panicker RO, Sabu MK (2020) Factors influencing the adoption of computerized medical diagnosing system for tuberculosis. Int J Inf Technol 12:503–512
Song C (2022) A hybrid SEM and ANN approach to predict the individual cloud computing adoption based on the UTAUT2. Int J Inf Technol 14(7):3539–3553
Ben Arfi W, Ben Nasr I, Kondrateva G, Hikkerova L (2021) The role of trust in intention to use the IoT in eHealth: Application of the modified UTAUT in a consumer context. Technol Forecast Soc Change 167:120688. https://doi.org/10.1016/j.techfore.2021.120688
Shiferaw KB, Mehari EA (2019) Modeling predictors of acceptance and use of electronic medical record system in a resource limited setting: using modified UTAUT model. Inform Med Unlocked 17:1001820. https://doi.org/10.1016/j.imu.2019.100182
Alaiad A (2017) Patients ’ adoption of WSN-based smart home healthcare systems : an integrated model of facilitators and barriers. IEEE Trans Prof Commun 60(1):1–20
Alaiad A, Alsharo M, Alnsour Y (2019) The determinants of M-health adoption in develo** countries: an empirical investigation. Appl Clin Inform 10(5):820–840. https://doi.org/10.1055/s-0039-1697906
Alam MZ, Hu W, Kaium MA, Hoque MR, Alam MMD (2020) Understanding the determinants of mHealth apps adoption in Bangladesh: a SEM-Neural network approach. Technol Soc 61:101255. https://doi.org/10.1016/j.techsoc.2020.101255
Alsahafi YA, Gay V, Khwaji AA (2020) The acceptance of national electronic health records in Saudi Arabia: healthcare consumers ’ perspectives. In: Australas. Conf. Inf. Syst., pp 1–12
Alan M, Hu W, Barua Z (2018) Using the UTAUT model to determine factors affecting acceptance and use of mobile health (mHealth) services in Bangladesh Mohammad. J Stud Soc Sci 17(2):137–172
Rabaa’i AA, Zhu X (2021) Understanding the determinants of wearable payment adoption: an empirical study. Interdiscip J Inf Knowl Manag. 16(1):173–211. https://doi.org/10.28945/4746
Almegbel H, Aloud M (2021) Factors influencing the adoption of mHealth services in Saudi Arabia: a patient-centered study. Int J Comput Sci Netw Secur 21(4):313–324
Baudier P, Kondrateva G, Ammi C (2020) The future of Telemedicine Cabin? The case of the French students’ acceptability. Futures 122:102595. https://doi.org/10.1016/j.futures.2020.102595
Riana D, Hidayanto AN, Hadianti S, Napitupulu D (2021) Integrative factors of E-health laboratory adoption: a case of Indonesia. Future Internet 13(2):26
Rho MJ, young Choi I, Lee J (2014) Predictive factors of telemedicine service acceptance and behavioral intention of physicians. Int J Med Inform 83(8):559–571
Baudier P, Kondrateva G, Ammi C, Chang V, Schiavone F (2021) Patients’ perceptions of teleconsultation during COVID-19: a cross-national study. Technol Forecast Soc Change 163:120510. https://doi.org/10.1016/j.techfore.2020.120510
Tsai J-M, Cheng M-J, Tsai H-H, Hung S-W, Chen Y-L (2019) Acceptance and resistance of telehealth: the perspective of dual-factor concepts in technology adoption. Int J Inf Manag 49:34–44
Hartono IK, Della TK, Kawi YA, Yuniarty (2021) Determinants factor affecting user continuance usage and intention to recommend of mobile telemedicine. IOP Conf Ser Earth Environ Sci 794(1):012079. https://doi.org/10.1088/1755-1315/794/1/012079
Li J, Ma Q, Chan AHS, Man SS (2019) Health monitoring through wearable technologies for older adults: smart wearables acceptance model. Appl Ergon 75:162–169
**a J-J, Gao M, Qiu S, Sang X-X, Ma X-L, Lee C-Y (2019) Research on patient acceptance behavior of online medical APP based on UTAUT improved model. DEStech Trans Econ Bus Manag. https://doi.org/10.12783/dtem/icem2019/31155
Kim TB, Ho CTB (2021) Validating the moderating role of age in multi-perspective acceptance model of wearable healthcare technology. Telemat Inform 61:101603. https://doi.org/10.1016/j.tele.2021.101603
Enaizan O, Eneizan B, Almaaitah M, Al-Radaideh AT, Saleh AM (2020) Effects of privacy and security on the acceptance and usage of EMR: the mediating role of trust on the basis of multiple perspectives. Inform Med Unlocked 21:100450
Shiferaw KB et al (2021) Healthcare providers’ acceptance of telemedicine and preference of modalities during COVID-19 pandemics in a low-resource setting: an extended UTAUT model. PLoS ONE 16(4):1–15. https://doi.org/10.1371/journal.pone.0250220
Mo O, Emuoyibofarhe JO, Oladosu JB (2019) A modified unified theory of acceptance and use of technology (Utaut) model For E-health services. J Exp 7(3):30–36
Fan W, Liu J, Zhu S, Pardalos PM (2020) Investigating the impacting factors for the healthcare professionals to adopt artificial intelligence-based medical diagnosis support system (AIMDSS). Ann Oper Res 294(1–2):567–592. https://doi.org/10.1007/s10479-018-2818-y
Dai B, Larnyo E, Tetteh EA, Aboagye AK, Musah AAI (2019) Factors affecting caregivers’ acceptance of the use of wearable devices by patients with dementia: an extension of the unified theory of acceptance and use of technology model. Am J Alzheimers Dis Other Demen 35:1–11. https://doi.org/10.1177/1533317519883493
Hennemann S, Beutel ME, Zwerenz R (2017) Ready for eHealth? Health professionals’ acceptance and adoption of eHealth interventions in inpatient routine care. J Health Commun 22(3):274–284. https://doi.org/10.1080/10810730.2017.1284286
Hoque R, Sorwar G (2017) Understanding factors influencing the adoption of mHealth by the elderly: an extension of the UTAUT model. Int J Med Inform 101:75–84. https://doi.org/10.1016/j.ijmedinf.2017.02.002
Tavares J, Goulão A, Oliveira T (2018) Electronic health record portals adoption: empirical model based on UTAUT2. Inform Health Soc Care 43(2):109–125. https://doi.org/10.1080/17538157.2017.1363759
Binyamin SS, Hoque MR (2020) Understanding the drivers of wearable health monitoring technology: an extension of the unified theory of acceptance and use of technology. Sustain 12(22):1–20. https://doi.org/10.3390/su12229605
A. T. Al-Radaideh and M. Alazzam, “Critical successful factors affecting adoption of e-health system in develo** countries,” Available SSRN 3522884, 2020.
Chang YT, Chao CM, Yu CW, Lin FC (2021) Extending the utility of UTAUT2 for hospital patients’ adoption of medical apps: moderating effects of e-health literacy. Mob Inf Syst 2021:1–10. https://doi.org/10.1155/2021/8882317
Agyei DD, Adzobu P (2020) Factors influencing professional nurses’ acceptance and use of mobile medical apps in Ghana. J Inf Technol Manag 12(1):27–42. https://doi.org/10.22059/JITM.2020.286522.2389
Gu D et al (2021) Assessing the adoption of e-health technology in a develo** country: an extension of the UTAUT model. SAGE Open. https://doi.org/10.1177/21582440211027565
Dhiman N, Arora N, Dogra N, Gupta A (2020) Consumer adoption of smartphone fitness apps: an extended UTAUT2 perspective. J Indian Bus Res 12(3):363–388. https://doi.org/10.1108/JIBR-05-2018-0158
Srivastava M, Raina M (2020) Consumers’ usage and adoption of e-pharmacy in India. Int J Pharm Healthc Mark 15(2):235–250. https://doi.org/10.1108/IJPHM-01-2020-0006
Damberg S (2021) Predicting future use intention of fitness apps among fitness app users in the United Kingdom: the role of health consciousness. Int J Sport Mark Spons. https://doi.org/10.1108/IJSMS-01-2021-0013
Yuan S, Ma W, Kanthawala S, Peng W (2015) Keep using my health apps: discover users’ perception of health and fitness apps with the UTAUT2 model. Telemed e-Health 21(9):735–741. https://doi.org/10.1089/tmj.2014.0148
Ahmed MH et al (2020) Intention to use electronic medical record and its predictors among health care providers at referral hospitals, north-West Ethiopia, 2019: using unified theory of acceptance and use technology 2(UTAUT2) model. BMC Med Inform Decis Mak 20(1):1–11. https://doi.org/10.1186/s12911-020-01222-x
Luyten J, Marneffe W (2021) Examining the acceptance of an integrated electronic health records system: insights from a repeated cross-sectional design. Int J Med Inform 150:104450. https://doi.org/10.1016/j.ijmedinf.2021.104450
Wang H, Tao D, Yu N, Qu X (2019) Understanding consumer acceptance of healthcare wearable devices: an integrated model of UTAUT and TTF. Int J Med Inform. https://doi.org/10.1016/j.ijmedinf.2020.104156
Khan IU, Yu Y, Hameed Z, Khan SU, Waheed A (2018) Assessing the physicians’ acceptance of E-prescribing in a develo** country: an extension of the UTAUT model with moderating effect of perceived organizational support. J Glob Inf Manag 26(3):121–142. https://doi.org/10.4018/JGIM.2018070109
Alsyouf A, Ishak AK (2018) Understanding EHRs continuance intention to use from the perspectives of UTAUT: practice environment moderating effect and top management support as predictor variables. Int J Electron Healthc 10(1–2):24–59. https://doi.org/10.1504/IJEH.2018.092175
Zailani S, Iranmanesh M, Nikbin D, Beng JKC (2015) Determinants of RFID adoption in Malaysia’s healthcare industry: occupational level as a moderator. J Med Syst 39(1):1–11
Duarte P, Pinho JC (2019) A mixed methods UTAUT2-based approach to assess mobile health adoption. J Bus Res 102:140–150. https://doi.org/10.1016/j.jbusres.2019.05.022
Palas JU, Sorwar G, Hoque MR, Sivabalan A (2022) Factors influencing the elderly’s adoption of mHealth: an empirical study using extended UTAUT2 model. BMC Med Inform Decis Mak 22(1):1–21
Faloye ST, Ndlanzi SL, Ajayi N (2021) Factors affecting e-health adoption in South African public hospitals: a case of Edendale hospital. In: 2021 IST-Africa Conference (IST-Africa). IEEE, pp. 1–11
Ramdani B, Duan B, Berrou I (2020) Exploring the determinants of mobile health adoption by hospitals in China: empirical study. JMIR Med informatics 8(7):e14795
Ahmad S, Iqbal T (2022) The role of management commitment in adoption of occupational health and safety at higher education institutions. Entrep Sustain Issues 9(3):103
Wolverton CC, Lanier PA (2019) Utilizing the Technology-Organization-Environment framework to examine the adoption decision in a healthcare context. In: Handbook of research on the evolution of IT and the rise of E-society.. IGI Global, pp 401–423
Esfahani MD, Nilashi M, Rahman AA, Ghapanchi AH, Zakaria NH (2019) Psychological factors influencing the managers’ intention to adopt green IS: a review-based comprehensive framework and ranking the factors. In: Green Bus. Concepts, Methodol. Tools, Appl., pp 1386–1419
Suman, Sonia, Jasrotia R, Singh SP (2023) A MCDM-based framework for selection of photovoltaic cell technology using novel information measure under Pythagorean fuzzy environment. Int J Inf Technol 15:4233–4242
Saaty TL (1988) What is the analytic hierarchy process? In: Mathematical models for decision support. Springer, pp 109–121
Singh P, Agrawal R (2021) AHP based network selection scheme for heterogeneous network in different traffic scenarios. Int J Inf Technol 13:2505–2513
Salahshour M, Dahlan HM, Iahad NA, Nilashi M, Ibrahim O (2015) Using a multi-criteria decision making approach for assessing the factors affecting social network sites intention to use. J Soft Comput Decis Support Syst 2(3):20–28
Eriş MB, Sezer EDG, Ocak Z (2022) Prioritization of the factors affecting the performance of clinical laboratories using the AHP and ANP techniques. Netw Model Anal Heal Informat Bioinform 12(1):5
Singh RK (2013) Prioritizing the factors for coordinated supply chain using analytic hierarchy process (AHP). Meas Bus Excell 17:80–97
Zaidan AA, Zaidan BB, Al-Haiqi A, Kiah MLM, Hussain M, Abdulnabi M (2015) Evaluation and selection of open-source EMR software packages based on integrated AHP and TOPSIS. J Biomed Inform 53:390–404
Sharma M, Gupta R, Acharya P (2020) Prioritizing the critical factors of cloud computing adoption using multi-criteria decision-making techniques. Glob Bus Rev 21(1):142–161
Gupta KP, Bhaskar P, Singh S (2017) Prioritization of factors influencing employee adoption of e-government using the analytic hierarchy process. J Syst Inf Technol 19:116–137
Zaidan AA, Zaidan BB, Alsalem MA, Momani F, Zughoul O (2020) Novel multiperspective hiring framework for the selection of software programmer applicants based on AHP and group TOPSIS techniques. Int J Inf Technol Decis Mak 19(03):775–847
Dias A Jr, Ioannou PG (1996) Company and project evaluation model for privately promoted infrastructure projects. J Constr Eng Manag 122(1):71–82
Duke JM, Aull-Hyde R (2002) Identifying public preferences for land preservation using the analytic hierarchy process. Ecol Econ 42(1–2):131–145
Shrestha RK, Alavalapati JRR, Kalmbacher RS (2004) Exploring the potential for silvopasture adoption in south-central Florida: an application of SWOT–AHP method. Agric Syst 81(3):185–199
Saaty TL (1990) How to make a decision: the analytic hierarchy process. Eur J Oper Res 48(1):9–26
Forman E, Peniwati K (1998) Aggregating individual judgments and priorities with the analytic hierarchy process. Eur J Oper Res 108(1):165–169
Ben Arfi W, Ben Nasr I, Khvatova T, Ben Zaied Y (2021) Understanding acceptance of eHealthcare by IoT natives and IoT immigrants: an integrated model of UTAUT, perceived risk, and financial cost. Technol Forecast Soc Change 163:120437. https://doi.org/10.1016/j.techfore.2020.120437
Vichitkraivin P, Naenna T (2021) Factors of healthcare robot adoption by medical staff in Thai government hospitals. Health Technol (Berl) 11(1):139–151. https://doi.org/10.1007/s12553-020-00489-4
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
I declare that there is no conflict of interest regarding the publication of this manuscript. The research conducted and the results presented in this manuscript are unbiased and free from any financial, personal, or professional conflicts of interest that could influence the objectivity, integrity, or interpretation of the findings. Furthermore, I confirm that all sources of financial support for this research are disclosed within the manuscript, and there are no competing interests that could potentially undermine the credibility or validity of the research. If necessary, I am willing to provide additional information or clarification regarding potential conflicts of interest related to this manuscript.
Appendix
Appendix
Q | Factor | Scale | Factor | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
1 | Perceived Risk | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Trust |
2 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Self-efficacy | |
3 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Personal Innovativeness | |
4 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Technology anxiety | |
5 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Price value | |
6 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Awareness | |
7 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Hedonic Motivation | |
8 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Habit | |
9 | Trust | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Self-efficacy |
10 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Personal Innovativeness | |
11 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Technology anxiety | |
12 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Price value | |
13 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Awareness | |
14 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Hedonic Motivation | |
15 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Habit | |
16 | Self-efficacy | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Personal Innovativeness |
17 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Technology anxiety | |
18 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Price value | |
19 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Awareness | |
20 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Hedonic Motivation | |
21 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Habit | |
22 | Personal Innovativeness | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Technology anxiety |
23 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Price value | |
24 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Awareness | |
25 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Hedonic Motivation | |
26 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Habit | |
27 | Technology anxiety | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Price value |
28 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Awareness | |
29 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Hedonic Motivation | |
30 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Habit | |
31 | Price value | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Awareness |
32 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Hedonic Motivation | |
33 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Habit | |
34 | Awareness | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Hedonic Motivation |
35 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Habit | |
36 | Hedonic Motivation | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Habit |
Q | Factor | Scale | Factor | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
1 | Performance expectancy | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Effort expectancy |
2 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Perceived security | |
3 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Perceived privacy | |
4 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Reliability | |
5 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Accessibility | |
6 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Availability | |
7 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Compatibility | |
8 | Effort expectancy | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Perceived security |
9 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Perceived privacy | |
10 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Reliability | |
11 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Accessibility | |
12 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Availability | |
13 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Compatibility | |
14 | Perceived security | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Perceived privacy |
15 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Reliability | |
16 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Accessibility | |
17 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Availability | |
18 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Compatibility | |
19 | Perceived privacy | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Reliability |
20 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Accessibility | |
21 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Availability | |
22 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Compatibility | |
23 | Reliability | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Accessibility |
24 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Availability | |
25 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Compatibility | |
26 | Accessibility | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Availability |
27 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Compatibility | |
28 | Availability | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Compatibility |
Q | Factor | Scale | Factor | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
1 | Social Influence | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Government Support |
2 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | E-health policy | |
3 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | External Pressure | |
4 | Government Support | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | E-health policy |
5 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | External Pressure | |
6 | E-health policy | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | External Pressure |
Q | Factor | Scale | Factor | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
1 | Facilitating conditions | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Resistance to change |
2 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Task Complexity | |
3 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Task technology fit | |
4 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Organizational support | |
5 | Resistance to change | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Task Complexity |
6 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Task technology fit | |
7 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Organizational support | |
8 | Task Complexity | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Task technology fit |
9 | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Organizational support | |
10 | Task technology fit | 9 | 8 | 7 | 6 | 5 | 4 | 3 | 2 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Organizational support |
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Altawaiha, I., Atan, R., Yaakob, R.B. et al. Assessing and prioritizing crucial drivers for CloudIoT-based healthcare adoption: an analytic hierarchy process approach. Int. j. inf. tecnol. (2024). https://doi.org/10.1007/s41870-024-01742-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s41870-024-01742-z