Abstract
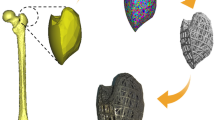
The rise of additive manufacturing gave hope to the design of orthopedic implants with comparable performance to natural human bone. The current research provides a numerical evaluation of the mechanical performance of three different Ti6Al4V cellular tibia implant designs. The investigated structures are face-centered cubic with vertical Z strut (FCCZ), reentrant and rhombic dodecahedron. Porous structures were designed with a pore size of 800 µm for bone ingrowth which improves implant fixation and osseo-integration. Porous stems were found to increase stress on the bone surface under the tibia tray accompanied by reducing both shear stress at the stem–bone interface and stress at the stem tip. Finally, proof-of-concept porous models 3D printed using Phrozen Shuffle XL demonstrated the manufacturability. A scanning electron microscope was used to measure the average pore sizes and the average strut sizes of the cellular microstructure to verify conformance to design.








Similar content being viewed by others
References
Enab TA, Bondok NE (2013) Material selection in the design of the tibia tray component of cemented artificial knee using finite element method. Mater Des 44:454–460. https://doi.org/10.1016/j.matdes.2012.08.017
AJRR (2020) The Seventh Annual Report of the AJRR on hip and knee arthroplasty. aaos.org/AJRRannualreport
Yao C, Lu J, Webster TJ (2010) Titanium and cobalt-chromium alloys for hips and knees. Biomaterials for Artificial Organs. Elsevier, Netherlands, pp 34–55. https://doi.org/10.1533/9780857090843.1.34
Burton HE, Eisenstein NM, Lawless BM et al (2018) The design of additively manufactured lattices to increase the functionality of medical implants. Mater Sci Eng C 2019(94):901–908. https://doi.org/10.1016/j.msec.2018.10.052
Kamath S, Chang W, Shaari E, Bridges A, Campbell A, McGill P (2008) Comparison of peri-prosthetic bone density in cemented and uncemented total knee arthroplasty. Acta Orthop Belg 74(3):354–359
Arabnejad S, Johnston B, Tanzer M, Pasini D (2017) Fully porous 3D printed titanium femoral stem to reduce stress-shielding following total hip arthroplasty. J Orthop Res 35(8):1774–1783. https://doi.org/10.1002/jor.23445
Han C, Li Y, Wang Q et al (2017) Continuous functionally graded porous titanium scaffolds manufactured by selective laser melting for bone implants. J Mech Behav Biomed Mater 2018(80):119–127. https://doi.org/10.1016/j.jmbbm.2018.01.013
Ran Q, Yang W, Hu Y et al (2018) Osteogenesis of 3D printed porous Ti6Al4V implants with different pore sizes. J Mech Behav Biomed Mater 84:1–11. https://doi.org/10.1016/j.jmbbm.2018.04.010
Wang L, Kang J, Sun C, Li D, Cao Y, ** Z (2017) Map** porous microstructures to yield desired mechanical properties for application in 3D printed bone scaffolds and orthopaedic implants. Mater Des 133:62–68. https://doi.org/10.1016/j.matdes.2017.07.021
Pałka K, Pokrowiecki R (2018) Porous titanium implants: a review. Adv Eng Mater 20(5):1–18. https://doi.org/10.1002/adem.201700648
Yuan L, Ding S, Wen C (2019) Additive manufacturing technology for porous metal implant applications and triple minimal surface structures: a review. Bioact Mater 4(1):56–70. https://doi.org/10.1016/j.bioactmat.2018.12.003
Gao C, Wang C, ** H et al (2018) Additive manufacturing technique-designed metallic porous implants for clinical application in orthopedics. RSC Adv 8(44):25210–25227. https://doi.org/10.1039/c8ra04815k
Kumaresan T, Gandhinathan R, Ramu M, Ananthasubramanian M (2015) Conceptual design and fabrication of porous structured scaffold for tissue engineering applications. Biomed Res 26(4):S42–S48
Taniguchi N, Fujibayashi S, Takemoto M et al (2016) Effect of pore size on bone ingrowth into porous titanium implants fabricated by additive manufacturing: an in vivo experiment. Mater Sci Eng C 59:690–701. https://doi.org/10.1016/j.msec.2015.10.069
Mazur M, Leary M, Sun S, Vcelka M, Shidid D, Brandt M (2016) Deformation and failure behaviour of Ti-6Al-4V lattice structures manufactured by selective laser melting (SLM). Int J Adv Manuf Technol 84(5–8):1391–1411. https://doi.org/10.1007/s00170-015-7655-4
Eldesouky I, Harrysson O, West H, Elhofy H (2017) Electron beam melted scaffolds for orthopedic applications. Addit Manuf 17:169–175. https://doi.org/10.1016/j.addma.2017.08.005
Cheng XY, Li SJ, Murr LE et al (2012) Compression deformation behavior of Ti-6Al-4V alloy with cellular structures fabricated by electron beam melting. J Mech Behav Biomed Mater 16(1):153–162. https://doi.org/10.1016/j.jmbbm.2012.10.005
Arabnejad Khanoki S, Pasini D (2013) Fatigue design of a mechanically biocompatible lattice for a proof-of-concept femoral stem. J Mech Behav Biomed Mater 22:65–83. https://doi.org/10.1016/j.jmbbm.2013.03.002
Eltlhawy B, Fouda N, Eldesouky I (2021) Numerical Evaluation of a Porous Tibial-Knee Implant using Gyroid Structure. J Biomed Phys Eng. https://doi.org/10.31661/jbpe.v0i0.2005-1116
Tawakol AE, Noha Fouda IE (2021) Comparison of functionally graded hip stem implants with various second-generation titanium alloys. J Appl Comput Mech. https://doi.org/10.22055/JACM.2020.32964.2115
Fouda N, Eltlhawy B, El-Midany T (2015) The effect of using PLA-HA coating on uncemented tibia prosthesis to decrease aseptic loosening and stress shielding. Int J Mech Mechatron Eng 15(6):76–83
Harrysson OLA, Cansizoglu O, Marcellin-Little DJ, Cormier DR, West HA (2008) Direct metal fabrication of titanium implants with tailored materials and mechanical properties using electron beam melting technology. Mater Sci Eng C 28(3):366–373. https://doi.org/10.1016/j.msec.2007.04.022
Moiduddin K, Al-Ahmari A, Kindi MA, Nasr ESA, Mohammad A, Ramalingam S (2016) Customized porous implants by additive manufacturing for zygomatic reconstruction. Biocybern Biomed Eng 36(4):719–730. https://doi.org/10.1016/j.bbe.2016.07.005
Lai YS, Chen WC, Huang CH, Cheng CK, Chan KK, Chang TK (2015) The effect of graft strength on knee laxity and graft in-situ forces after posterior cruciate ligament reconstruction. PLoS ONE 10(5):1–11. https://doi.org/10.1371/journal.pone.0127293
Bahraminasab M, Sahari BB, Edwards KL, Farahmand F, Hong TS, Naghibi H (2013) Material tailoring of the femoral component in a total knee replacement to reduce the problem of aseptic loosening. Mater Des 52:441–451. https://doi.org/10.1016/j.matdes.2013.05.066
Asiri S, Fouda N, Hedia H (2016) Functionally graded coating material of cementless knee prosthesis. Br J Appl Sci Technol 15(5):1–12. https://doi.org/10.9734/bjast/2016/25618
Navarro M, Michiardi A, Castaño O, Planell JA (2008) Biomaterials in orthopaedics. J R Soc Interface 5(27):1137–1158. https://doi.org/10.1098/rsif.2008.0151
Chahine G, Atharifar H, Smith P, Kovacevic R (2009) Design optimization of a customized dental implant manufactured via Electron Beam Melting®. 20th Annu Int Solid Free Fabr Symp SFF 2009. Published online. p 631–640
Completo A, Fonseca F, Simões JA (2008) Strain shielding in proximal tibia of stemmed knee prosthesis: experimental study. J Biomech 41(3):560–566. https://doi.org/10.1016/j.jbiomech.2007.10.006
Nambu SN, Lewis G (2004) Influences of the temporal nature of the applied load and the tibial baseplate material on the stress distribution in a three-dimensional model of the human knee joint containing a prosthetic replacement. Biomed Mater Eng 14(2):203–217
Enab TA (2012) A comparative study of the performance of metallic and FGM tibia tray components in total knee replacement joints. Comput Mater Sci 53(1):94–100. https://doi.org/10.1016/j.commatsci.2011.09.032
Mangado N, Quevedo C, Lozano L, Suso S, Cerrolaza M (2015) To what extent the combination of stem length and stem inclination do affect the performance of the tibial component in knee implants? Biomed Eng - Appl Basis Commun 27(2):1–11. https://doi.org/10.4015/S1016237215500180
Chong DYR, Hansen UN, Amis AA (2010) Analysis of bone-prosthesis interface micromotion for cementless tibial prosthesis fixation and the influence of loading conditions. J Biomech 43(6):1074–1080. https://doi.org/10.1016/j.jbiomech.2009.12.006
Mattila RH, Laurila P, Rekola J et al (2009) Bone attachment to glass-fibre-reinforced composite implant with porous surface. Acta Biomater 5(5):1639–1646. https://doi.org/10.1016/j.actbio.2009.01.020
El-Zayat BF, Heyse TJ, Fanciullacci N, Labey L, Fuchs-Winkelmann S, Innocenti B (2016) Fixation techniques and stem dimensions in hinged total knee arthroplasty: a finite element study. Arch Orthop Trauma Surg 136(12):1741–1752. https://doi.org/10.1007/s00402-016-2571-0
Barrack RL, Stanley T, Burt M, Hopkins S (2004) The effect of stem design on end-of-stem pain in revision total knee arthroplasty. J Arthroplasty 19(7 SUPPL):119–124. https://doi.org/10.1016/j.arth.2004.06.009
Eldesouky I, Harrysson O, Marcellin-Little DJ, West H, El-Hofy H (2017) Pre-clinical evaluation of the mechanical properties of a low-stiffness cement-injectable hip stem. J Med Eng Technol 41(8):681–691. https://doi.org/10.1080/03091902.2017.1394391
Buechel FF, Pappas MJ (2015) Principles of human joint replacement. Springer, Cham. https://doi.org/10.1007/978-3-319-15311-7
Wang X, Xu S, Zhou S et al (2016) Topological design and additive manufacturing of porous metals for bone scaffolds and orthopaedic implants: a review. Biomaterials 83:127–141. https://doi.org/10.1016/j.biomaterials.2016.01.012
Ataee A, Li Y, Fraser D, Song G, Wen C (2018) Anisotropic Ti-6Al-4V gyroid scaffolds manufactured by electron beam melting (EBM) for bone implant applications. Mater Des 137:345–354. https://doi.org/10.1016/j.matdes.2017.10.040
Ataee A, Li Y, Brandt M, Wen C (2018) Ultrahigh-strength titanium gyroid scaffolds manufactured by selective laser melting (SLM) for bone implant applications. Acta Mater 158:354–368. https://doi.org/10.1016/j.actamat.2018.08.005
Acknowledgements
The authors acknowledge the support of Egypt-Japan University of Science and Technology (E-JUST) for providing the software used in this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Data availability
The datasets generated and analyzed during the current study are not publicly available but may be obtained from the corresponding author at reasonable request.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Eltlhawy, B., Fouda, N., El-Midany, T. et al. Numerical assessment of advanced porous tibia implant designs based on different cellular structures. Prog Addit Manuf 8, 807–817 (2023). https://doi.org/10.1007/s40964-022-00358-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40964-022-00358-8