Abstract
Purpose of Review
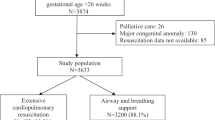
In this manuscript, we will review core noncardiac medical management principles for the preterm infant with congenital heart disease (CHD). We describe common respiratory diseases of the newborn period, apnea of prematurity, the significance of thermoregulation, and management of hyperbilirubinemia. Taken together, these management considerations optimize neurodevelopment and growth of the infant with CHD while minimizing significant neonatal comorbidities.
Recent Findings
The comorbidities of prematurity affect both neonates with and without CHD. Respiratory distress syndrome can be a significant consequence of premature birth, and early surfactant administration is associated with decreased air leak, bronchopulmonary dysplasia (BPD), and mortality. If invasive mechanical ventilation is necessary, volume-targeted ventilation is preferred in preterm neonates with associated shorter duration of mechanical ventilation and decreased comorbidities. Recommendations for the management of hypoglycemia in infants exist, but are dependent on enteral feeding; thus, these recommendations may not be applicable to the neonate with CHD who cannot tolerate enteral feeding. Hypothermia is a common problem in premature infants and can result in high tissue oxygen demand and consumption with subsequent metabolic acidosis. Such effects can be exacerbated in the infant with CHD and may increase the risk for morbidities and mortality.
Summary
Though there have been many medical and surgical advancements in the care of preterm infants with CHD, the rates of morbidity and mortality remain high. Understanding key principles related to common complications of prematurity can be critical to improving long-term outcomes.


Similar content being viewed by others
Data Availability
No datasets were generated or analysed during the current study.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Reddy RK, McVadon DH, Zyblewski SC, Rajab TK, Diego E, Southgate WM, et al. Prematurity and congenital heart disease: a contemporary review. NeoReviews. 2022;23(7):e472–85.
Norman M, Håkansson S, Kusuda S, Vento M, Lehtonen L, Reichman B, et al. Neonatal outcomes in very preterm infants with severe congenital heart defects: an international cohort study. J Am Heart Assoc. 2020;9(5):e015369.
Clark RH. The epidemiology of respiratory failure in neonates born at an estimated gestational age of 34 weeks or more. J Perinatol. 2005;25(4):251–7.
Ekhaguere OA, Okonkwo IR, Batra M, Hedstrom AB. Respiratory distress syndrome management in resource limited settings-current evidence and opportunities in 2022. Front Pediatr. 2022;10: 961509.
Karnati S, Kollikonda S, Abu-Shaweesh J. Late preterm infants - changing trends and continuing challenges. Int J Pediatr Adolesc Med. 2020;7(1):36–44.
Htun ZT, Hairston JC, Gyamfi-Bannerman C, Marasch J, Duarte Ribeiro AP. Antenatal corticosteroids: extending the practice for late-preterm and scheduled early-term deliveries? Children. 2021;8(4):272. https://doi.org/10.3390/children8040272.
Yadav S, Lee B, Kamity R. Neonatal respiratory distress syndrome. StatPearls Publishing; 2023.
•• Ng EH, Shah V. Guidelines for surfactant replacement therapy in neonates. Paediatr Child Health. 2021;26(1):35–49. Systematic review demonstrates early surfactant administration within the first 2 hours of life is associated with decreased air leak, bronchopulmonary dysplasia (BPD), and mortality.
Schmolzer GM, Kumar M, Pichler G, Aziz K, O’Reilly M, Cheung PY. Non-invasive versus invasive respiratory support in preterm infants at birth: systematic review and meta-analysis. Centre for Reviews and Dissemination (UK); 2013.
Bronicki RA, Benitz WE, Buckley JR, Yarlagadda VV, Porta NFM, Aganga DO, et al. Respiratory care for neonates with congenital heart disease. Pediatrics. 2022;150(Supplement 2):e2022056415H.
•• Klingenberg C, Wheeler KI, McCallion N, Morley CJ, Davis PG. Volume-targeted versus pressure-limited ventilation in neonates. Cochrane Database Syst Rev. 2017;10(10):CD003666. Volume-targeted ventilation is associated with shorter duration of mechanical ventilation and decreased comorbidities in preterm infants and is the preferred mode of ventilation when possible.
Peng W, Zhu H, Shi H, Liu E. Volume-targeted ventilation is more suitable than pressure-limited ventilation for preterm infants: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2014;99(2):F158–65.
Eichenwald EC, Watterberg KL, Aucott S, Benitz WE, Cummings JJ, Goldsmith J, et al. Apnea of prematurity. Pediatrics. 2016;137(1):e20153757.
Williamson M, Poorun R, Hartley C. Apnoea of prematurity and neurodevelopmental outcomes: current understanding and future prospects for research. Front Pediatr. 2021;9:755677.
Pergolizzi J, Kraus A, Magnusson P, Breve F, Mitchell K, Raffa R, et al. Treating apnea of prematurity. Cureus. 2022;14(1):e21783.
Zhao J, Gonzalez F, Mu D. Apnea of prematurity: from cause to treatment. Eur J Pediatr. 2011;170(9):1097–105.
Henderson-Smart DJ, De Paoli AG. Methylxanthine treatment for apnoea in preterm infants. Cochrane Database Syst Rev. 2010;(12):CD000140.
Kumar VHS, Lipshultz SE. Caffeine and clinical outcomes in premature neonates. Children. 2019;6(11):118. https://doi.org/10.3390/children6110118.
• Moschino L, Zivanovic S, Hartley C, Trevisanuto D, Baraldi E, Roehr CC. Caffeine in preterm infants: where are we in 2020? ERJ Open Res. 2020;6(1). https://doi.org/10.1183/23120541.00330-2019. Review of the causes and management of apnea of prematurity.
Puia-Dumitrescu M, Smith PB, Zhao J, Soriano A, Payne EH, Harper B, et al. Dosing and Safety of off-label use of caffeine citrate in premature infants. J Pediatr. 2019;211:27-32.e1.
Abdel-Hady H, Nasef N, Shabaan AE, Nour I. Caffeine therapy in preterm infants. World J Clin Pediatr. 2015;4(4):81–93.
Schmidt B, Roberts RS, Davis P, Doyle LW, Barrington KJ, Ohlsson A, et al. Caffeine therapy for apnea of prematurity. N Engl J Med. 2006;354(20):2112–21.
Singh Y, Mikrou P. Use of prostaglandins in duct-dependent congenital heart conditions. Arch Dis Child Educ Pract Ed. 2018;103(3):137–40.
Ohara T, Ogata H, Fujiyama J, Murata Y, Abe J, Kakuta K, et al. Effects of prostaglandin E1 infusion in the pre-operative management of critical congenital heart disease. Tohoku J Exp Med. 1985;146(2):237–49.
Abramowski A, Ward R, Hamdan AH. Neonatal hypoglycemia. StatPearls Publishing; 2023.
• Thompson-Branch A, Havranek T. Neonatal hypoglycemia. Pediatr Rev. 2017;38(4):147–57. AAP recommendations on the management of infant hypoglycemia emphasize oral feeding as treatment; these recommendations may be of limited utility in the neonate with congenital heart disease who is not able to tolerate enteral feeding.
Güemes M, Rahman SA, Hussain K. What is a normal blood glucose? Arch Dis Child. 2016;101(6):569–74.
Committee on Fetus and Newborn, Adamkin DH. Postnatal glucose homeostasis in late-preterm and term infants. Pediatrics. 2011;127(3):575–9.
Sharma A, Davis A, Shekhawat PS. Hypoglycemia in the preterm neonate: etiopathogenesis, diagnosis, management and long-term outcomes. Transl Pediatr. 2017;6(4):335–48.
Stanescu A, Stoicescu SM. Neonatal hypoglycemia screening in newborns from diabetic mothers--arguments and controversies. J Med Life. 2014;7 Spec No. 3(Spec Iss 3):51–2.
Rozance PJ. Hypoglycemia in the newborn and neurodevelopmental outcomes in childhood. JAMA. 2022;327(12):1135–7.
Lucas A, Morley R, Cole TJ. Adverse neurodevelopmental outcome of moderate neonatal hypoglycaemia. BMJ. 1988;297(6659):1304–8.
Rozance PJ, Wolfsdorf JI. Hypoglycemia in the newborn. Pediatr Clin North Am. 2019;66(2):333–42.
Thornton PS, Stanley CA, De Leon DD, Harris D, Haymond MW, Hussain K, et al. Recommendations from the pediatric endocrine society for evaluation and management of persistent hypoglycemia in neonates, infants, and children. J Pediatr. 2015;167(2):238–45.
Kutamba E, Lubega S, Mugalu J, Ouma J, Mupere E. Dextrose boluses versus burette dextrose infusions in prevention of hypoglycemia among preterms admitted at Mulago Hospital: an open label randomized clinical trial. Afr Health Sci. 2014;14(3):502–9.
Kaiser JR, Bai S, Gibson N, Holland G, Lin TM, Swearingen CJ, et al. Association between transient newborn hypoglycemia and fourth-grade achievement test proficiency: a population-based study. JAMA Pediatr. 2015;169(10):913–21.
McKinlay CJD, Alsweiler JM, Anstice NS, Burakevych N, Chakraborty A, Chase JG, et al. Association of neonatal glycemia with neurodevelopmental outcomes at 4.5 years. JAMA Pediatr. 2017;171(10):972–83.
Shah R, Dai DWT, Alsweiler JM, Brown GTL, Geoffrey Chase J, Gamble GD, et al. Association of neonatal hypoglycemia with academic performance in mid-childhood. JAMA. 2022;327(12):1158–70.
Edwards T, Alsweiler JM, Crowther CA, Edlin R, Gamble GD, Hegarty JE, et al. Prophylactic oral dextrose gel and neurosensory impairment at 2-year follow-up of participants in the hPOD randomized trial. JAMA. 2022;327(12):1149–57.
Abiramalatha T, Ramaswamy VV, Bandyopadhyay T, Pullattayil AK, Thanigainathan S, Trevisanuto D, et al. Delivery room interventions for hypothermia in preterm neonates: a systematic review and network meta-analysis. JAMA Pediatr. 2021;175(9):e210775.
Bhatt DR, White R, Martin G, Van Marter LJ, Finer N, Goldsmith JP, et al. Transitional hypothermia in preterm newborns. Adv Neonatal Care. 2010;10(5 Suppl):S15–7.
Medoff Cooper B, Holditch-Davis D, Verklan MT, Fraser-Askin D, Lamp J, Santa-Donato A, et al. Newborn clinical outcomes of the AWHONN late preterm infant research-based practice project. J Obstet Gynecol Neonatal Nurs. 2012;41(6):774–85.
Dang R, Patel AI, Weng Y, Schroeder AR, Lee HC, Aby J, et al. Incidence of neonatal hypothermia in the newborn nursery and associated factors. JAMA Netw Open. 2023;6(8):e2331011.
Demtse AG, Pfister RE, Nigussie AK, McClure EM, Ferede YG, Tazu Bonger Z, et al. Hypothermia in preterm newborns: impact on survival. Glob Pediatr Health. 2020;7:2333794X20957655.
Ringer SA. Core concepts: thermoregulation in the newborn, part ii: prevention of aberrant body temperature. NeoReviews. 2013;14(5):e221–6.
Wyckoff MH, Wyllie J, Aziz K, de Almeida MF, Fabres JW, Fawke J, et al. Neonatal life support 2020 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation. 2020;156:A156–87.
Miller SS, Lee HC, Gould JB. Hypothermia in very low birth weight infants: distribution, risk factors and outcomes. J Perinatol. 2011;31(Suppl 1):S49-56.
•• Ting JY, Synnes AR, Lee SK, Shah PS, Canadian Neonatal Network and Canadian Neonatal Follow-Up Network. Association of admission temperature and death or adverse neurodevelopmental outcomes in extremely low-gestational age neonates. J Perinatol. 2018;38(7):844–9. Hypothermia triggers a hypermetabolic state to break down brown fat stores to create heat and maintain body temperature. This results in high oxygen tissue and nutrient consumption, metabolic acidosis, hypoglycemia, and additional fluid and electrolyte imbalances that can lead to multiorgan dysfunction and even death.
Mank A, van Zanten HA, Meyer MP, Pauws S, Lopriore E, Te Pas AB. Hypothermia in preterm infants in the first hours after birth: occurrence, course and risk factors. PLoS ONE. 2016;11(11):e0164817.
Liu H, Li J, Guo J, Shi Y, Wang L. A prediction nomogram for neonatal acute respiratory distress syndrome in late-preterm infants and full-term infants: a retrospective study. eClinicalMedicine. 2022;50:101523. https://doi.org/10.1016/j.eclinm.2022.101523.
Sarici SU, Serdar MA, Korkmaz A, Erdem G, Oran O, Tekinalp G, et al. Incidence, course, and prediction of hyperbilirubinemia in near-term and term newborns. Pediatrics. 2004;113(4):775–80.
American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics. 2004;114(1):297–316.
Ansong-Assoku B, Shah SD, Adnan M, Ankola PA. Neonatal jaundice. Stat Pearls Publishing; 2023.
Fawaz R, Baumann U, Ekong U, Fischler B, Hadzic N, Mack CL, et al. Guideline for the evaluation of cholestatic jaundice in infants: joint recommendations of the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition and the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition. J Pediatr Gastroenterol Nutr. 2017;64(1):154–68.
Mitra S, Rennie J. Neonatal jaundice: aetiology, diagnosis and treatment. Br J Hosp Med. 2017;78(12):699–704.
Shapiro SM. Definition of the clinical spectrum of kernicterus and bilirubin-induced neurologic dysfunction (BIND). J Perinatol. 2005;25(1):54–9.
Bhutani VK, Stark AR, Lazzeroni LC, Poland R, Gourley GR, Kazmierczak S, et al. Predischarge screening for severe neonatal hyperbilirubinemia identifies infants who need phototherapy. J Pediatr. 2013;162(3):477-482.e1.
Author information
Authors and Affiliations
Contributions
P.V. and J.K. both wrote the manuscript text and prepared the figures.
Corresponding author
Ethics declarations
Conflict of Interest
Pavika Varma declares that she has no conflict of interest. John S. Kim declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Cardiology/CT Surgery
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Varma, P., Kim, J.S. Medical Management Considerations of Premature Infants with Congenital Heart Disease. Curr Treat Options Peds 10, 39–51 (2024). https://doi.org/10.1007/s40746-024-00294-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40746-024-00294-5