Opinion statement
While there have been significant technical advances in the provision of health care to children, there remains ongoing challenges in develo** a culture of safety in pediatrics and child health. In many health systems, quality and safety programs are fragmented and the results variable. Health leaders need to ensure that care remains compassionate, child centered, and reliable across the systems in which they work. In order to transform our health system, we need to build and spread a culture of safety and reliability. Understanding the challenges and opportunities required to develop a culture of safety in pediatrics is best explored at three different levels. This paper aims to explore opportunities to build a culture of safety in pediatrics and child health at three levels. The first is the ward or unit base, the second is the hospital or heath system at large, and the third is whole system transformation at state, national, and global level.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The last 20 years has seen dramatic changes to the way medicine is practiced. Community expectations are significantly increased. Pediatrics and child health is no different. Children in our care deserve the right care every time [1••]. It is the obligation of health professionals to provide safe and reliable care. Develo** a culture of safe care that is patient centered remains a challenge for many health systems that are steeped in outdated, hierarchical, doctor-centric practices that put the needs of the patient behind the system and the professionals that work in it [2••]. Iatrogenic harm continues to contribute to preventable deaths with a number of studies in Europe and the USA showing alarming statistics. Newer harm detection techniques show that national rates of harm are four times greater than originally thought [3••]. In the USA, 15–35 % of children in hospital were found to have health care-associated harm [4]. A new study has shown that 26 % of child deaths in the UK have identifiable failures in care and that significant safety incidents occurs in the primary care setting [5].
Despite significant improvements in the provision of the technical care for children, there remains an urgent need to transform health care to ensure that it remains patient and person centered and compassionate and not overwhelmed by the technology. Care today remains fragmented and variable with little regard to established guidelines and protocols [6]. For the health system to change, we need a new breed of clinical pediatric leaders with a system-wide approach [1••]. They will have to be outcome focused, data driven, and passionate about the need for a safe and reliable system that cares for our children.
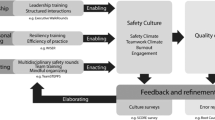
In order to transform our health system, we need to build a culture of safety. Understanding the challenges and opportunities required to develop a culture of safety in pediatrics is best explored at three different levels. This paper aims to explore opportunities to build a culture of safety in pediatrics and child health at three levels. The first is the ward or unit base, the second is the hospital or health system at large, and the third is whole system transformation at a state, national, or global level.
Care at bedside—the micro-system level
The key to good, high-quality, reliable care is still at the bedside (Table 1). That is where the children are and it is where care is delivered. The cornerstone of develo** a culture of safe care at the unit level is the ability to monitor and mitigate adverse events. The most well-known mechanism is the mortality and morbidity meeting. However, new strategies such as standardized chart review are emerging. They can enhance the traditional mortality and morbidity meetings by picking up more safety events [7]. There are different methodologies to investigate poor outcomes and adverse events. Root cause analysis (RCA) can be used to investigate significant adverse events, explore system issues in the department, and develop a set of recommendations to help prevent the significant event from happening again [8].
Strong local leadership remains the key to develo** effective and safe systems at the local unit level [9••]. However, strong clinical leadership needs to be augmented by empowering local clinicians to develop improvement capability at the front line [10•]. A key factor in develo** a safe culture is finding, nurturing, and mentoring clinical champions. Engage clinicians in local improvement activities and assist them with QI training opportunities, skilled teachers as part of the QI faculty, and a focused training curriculum for quality and patient safety [11]. The best way to progress improvement at the local, clinical micro-system level is to find a local clinical problem worth solving. The head of department should encourage their clinical champions to develop an appropriate multi-disciplinary team and ensure that the team has the support of the hospital executive to progress the quality improvement work. Key to success is to ensure that the local quality improvement project align with hospital and departmental priorities. The suggested model for improvement is the well-known PDSA cycle. Plan-Do-Study-Act cycles allow clinicians to introduce small-scale changes and then test the effect of the change and refine the changes further as required [8]. It is important to make involvement in QI, a key part of the unit culture. Aim for early wins and celebrate success as a unit. Encourage QI activities by tying them to academic promotion and career progression in the unit.
Clinical leaders need to be visible and to lead for safety. Safety walk rounds in neonatal or pediatric intensive care units or general children’s wards have been shown to be highly effective in promoting a safer place to deliver and receive care [12, 13]. The walk rounds are an excellent opportunity to improve communication between the unit leaders and front line staff. It allows for open, real-time discussion about potential adverse events and promotes a transparent, safer culture in the local unit. The culture or climate of a unit has been shown to influence patient safety outcomes (http://www.health.org.uk/publications/measuring-safety-culture/).
At a local unit level, medication errors remain the most likely adverse event to occur. Children are at a much greater risk of medication errors than adults. A large-scale review found medication errors in children’s units to range from 5 to 27 % with an average of 10 %. Errors occurred in prescribing, dispensing, and administration of medication [14]. It would be difficult to develop a culture of safety at a local pediatric level without focusing on medication safety and develo** strategies to reduce medications errors, especially those that result in harm to children. There are many strategies that can be employed at the local unit level to reduce medication errors; however, a novel concept showing promise is that of the consultant led ward round checklist to improve pediatric prescribing [15]. Early results show that the check and correct checklist leads to an improvement in the quality of prescribing. Insisting on a consultant led check and correct ward round sends a clear message to front line clinicians that safe prescribing is a clear priority of the unit leadership and an essential component of a safe and reliable local unit culture.
Clinical handover is a well-established tool that improves communication and reduces error. It will be addressed further in section two. However, a newer concept in health care is that of situational awareness. This is about mindfulness of the environment and anticipating potential future problems such as deteriorating patients. In health care, this situational awareness can be implemented via the unit-based huddle. Recent research has shown that huddles can increase clinical accountability, enhance collective awareness of harm, and improve collegiality among staff from different clinical backgrounds [16].
Care at the hospital macro-system level
Pediatric units and wards do not exist in isolation (Table 2). They are clinical micro-systems that coexist as part of a bigger hospital and health system [17]. In order to transform a hospital macro-system, it is essential to have high-functioning micro-systems at the unit level. There is only so much that they can achieve at a local unit level to develop a safe culture. In the absence of a broad hospital organizational culture that strives for safety and reliability, local units will not progress to their full safety and quality potential. Hospital executives, board members, and clinical leaders need to develop a governance structure that has system-wide oversight and accountability for all patient safety matters [18–20].
The hospital executive should set up a serious incident review committee where all serious events across the entire hospital or health system are reviewed, trended, and graded according to severity. It should take accountability for ensuring that the actions and recommendations arising from the various investigations are implemented in a timely manner. Membership should not be limited to senior doctors. The committee needs to have broad skill mix including nursing, allied health, and junior medical staff to ensure that incidents are reviewed from a multi-disciplinary framework. Engaging with clinical staff is crucial in develo** a safer culture. Hospital executives need to develop an appropriate range of relevant data to drive change. The data should be meaningful outcome-based data. It should also be easy to interpret by clinical staff without an advanced degree in statistics. Too many executives focus on access metrics and process measures. These are important but are over-emphasized in relation to clinical outcome measures. Child health professionals care about the clinical outcomes of the children they look after. A culture of safety should ensure that they should have robust, timely data that can act as a feedback loop on their performance [21].
Communication errors are common in the complex health systems in which we work. Many staff now work in shifts which means that clinical handover is vital to ensure that a patient’s care is not compromised by a change in staff or team. While huddles and situational awareness should be unit based, hospital and health systems should ensure that there is a highly reliable hospital-wide handover process. The handover is critical, as it requires transfer of clinical information and responsibility between teams. A recent study in 23 US hospitals [21] showed that a standardized handover process could significantly reduce handover failures from a baseline of 25 % to just fewer than 8 %. Ideally, the handover process or bundle needs to be embedded within the electronic medical record.
Children in acute care settings deteriorate in a predictable manner for the most part. Careful examination of their observation chart will almost always show a stepwise deterioration in their clinical parameters. This is the thinking behind a clinical emergency response system that includes standardized track and trigger age appropriate observation charts and a well-resourced and trained rapid response team (www.cec.health.nsw.gov.au/programs/betweentheflags) [22]. Rapid response teams are still controversial for some pediatricians. Part of the difficulty is in measuring their success in improving outcomes and reducing harm to children. In adults out of ICU, arrests are thought to be a useful measure; however, given that there are so few cardiac arrests in children, this measure has far less usefulness in pediatrics.
A funded, equipped, and embedded appropriate clinical emergency response system is a cornerstone of a safe culture. However, the rapid response team should also be able to be activated by members of the child’s family. Parents know their child best and can recognize signs of potential deterioration. A recent study on family-activated rapid response teams showed that families activating the rapid response team were not a burden on responders. Families, like clinicians, most commonly called the rapid response team as a result of concerns of clinical deterioration. Another reason for activating the team was poor communication between the teams and the family or a perceived dismissive response from the team towards a family’s concerns [23].
The understanding of a patient’s (parents’ and the child’s) perspective of patient safety is absolutely critical. After all, they are at the very forefront of care and their perceptions can provide valuable real-time feedback on the safety culture of a hospital or health system [24]. However, develo** a safe culture in pediatrics has to be more than just addressing patient feedback about their perceptions of care or adhering to a so-called “child centered care” philosophy. Families and children have to be at the center of the care process and many of the components of care that we provide will have to be redesigned to be child friendly so that they truly meet the needs of the child and their family [10•, 25]. In a safe culture, patient feedback on their experience of care and their perspective on safety will provide a highly useful complement to traditional patient safety outcomes and indicators that we measure. Health care is complex and sometimes we, as clinicians, make mistakes. In the past, these mistakes were often ignored and a culture of secrecy prevailed. A hospital or health system has to ensure that when a mistake leads to harm, a clinician is trained and willing to apologize and make a full open disclosure to the family. The disclosure has to be accompanied by an explanation of how the incident or adverse event occurred and how it will be investigated and mitigated. Open disclosure is designed to provide a framework that assists clinicians and managers in having open discussions with patients and their families. Only an open and honest atmosphere can contribute to a safe culture in pediatrics [26]. In NSW, the Clinical Excellence Commission has recently updated its open disclosure policy. The new program builds on the existing experience and increases the focus on improving communication between children, their family, and health care staff. A new CEC open disclosure handbook has been formulated, and a novel, simulation-based education program using actors has been introduced for health care staff (www.cec.health.nsw.gov.au/programs/open-disclosure).
The appropriate use of antimicrobials is an essential part of a hospital’s patient safety program. Hospital executives should ensure that a robust program of antimicrobial stewardship is implemented across the system, which they manage. Such a program should use clinical champions to drive an evidence-based program that enhance appropriate selection, duration, and timely cessation of antimicrobial therapy [27, 28]. A key strategy in reducing antibiotic resistance and toxicity in children is to have a comprehensive nosocomial surveillance program supported by well-developed antimicrobial and anti-fungal stewardship principles.
Care at the system-wide level
The final part of this paper will review a number of exciting and innovative programs that extend beyond hospitals and health systems to state and national large-scale transformation (Table 3). These programs offer a glimpse of the potential that programs spread at scale can contribute to a national and global culture of safety in pediatrics and child health. A recent study [29] has highlighted some of the essential characteristics required for successful large-scale transformation. The key components compromise effective leadership, engaging clinicians, and close collaboration with children and their families.
As mentioned earlier, a key component of a safe hospital culture is a robust clinical emergency response system that is able to recognize and respond to deteriorating patients. In New South Wales, Australia, the Clinical Excellence Commission has pioneered a large state-wide program named “Between the Flags.” The Pediatric BTF program (www.cec.health.nsw.gov.au/programs/betweentheflags) [22] was launched in 2011. It consisted of six age appropriate track and trigger observation charts and a locally trained and resourced rapid response team. The exact composition of the team varies in kee** with the size and complexity of each facility. The program is now deeply embedded across all 220 facilities in NSW, and as a result, every child has their observations plotted on the same color-coded observation chart. This reduced variation is a great bonus for rotating junior medical staff and nursing staff. It also allows for large-scale evaluation across the state. A program based on the same set of principles called VICTOR has now also been rolled out in the state of Victoria, Australia. Other states in Australia as well as overseas are looking to the principles and lessons learned from BTF and VICTOR as they go about implementing their own deteriorating patient programs.
Another promising program being rolled out across 12 hospitals in England is the SAFE Program—Situational Awareness for Everyone. It has recently launched under the auspices of the Royal College of Pediatrics and Child Health. Over the course of 2 years, it aims to transform care by reducing preventable deaths and harm in pediatric facilities in England [30]. The program will aim to introduce new models of care as well as embed the previously discussed huddle concept. The huddle technique allows frank discussions between clinical and non-clinical staff with the aim of recognizing and preventing deteriorating patients. The SAFE program hopes to embed a safety culture in England so that pediatric safety outcomes are similar to the best performing countries in Europe.
The RCPCH is also involved in another exciting initiative involving medication safety. As documented, earlier medication errors in children represents a significant cause of harm. Meds IQ (www.medsiq.org) is a new website that aims to share best practice in medication safety by bringing together improvement projects and quality tools as a free online educational resource. By pooling resources and sharing lessons learned, MEDS IQ has the potential to reduce medication errors across the UK and indeed the world.
The Pediatric National Inpatient Medication chart in Australia (www.safetyandquality.gov.au/ourwork/medication) is another example of a national initiative contributing to a safer pediatric culture at scale. The PNIMC was developed 6 years ago under the guidance and leadership of the Australian Commission on Safety and Quality in Health Care. It aimed to reduce variation among pediatric prescribers as prior to the introduction of the PNIMC, all hospitals and states had their own suite of medication charts. The chart has resulted in national standardization of medication charts across an entire country regardless of whether the charts are used electronically or are paper based. It means that every child has their medication charted on the same chart regardless of which hospital they are admitted to or state that they reside in.
Pediatric collaborative networks are multi-site clinical networks that allow clinical teams to learn from each other in a non-competitive, supportive environment. The aim is to test changes that improve quality and safety, learn from each others collective experience, and implement and spread successful changes that work [31]. The Solutions for Patient Safety collaborative in the USA is a network of 80 hospitals that share a vision that no child will be harmed while under their care. Competition between hospitals is put aside so that successes and failures are shared openly by all participants allowing them all to become safer (www.solutionsforpatientsafety.org). Another current example of collaboration is the Making it Safer Together—“MIST” pediatric patient safety collaborative. The collaborative is an open form among an alliance of hospitals in the UK that aims to share ideas for caring for children in a safer way (www.mist.org). Each unit collects data on a certain aspect of care with the aim for each organization to improve their own safety scores year on year.
Learning from adverse events is crucial to develo** a safe culture. In NSW, the Clinical Excellence Commission has recently set up a children and young person’s RCA committee. The committee mirrors the highly successful NSW state RCA committee [32]. It reviews all RCA investigations that have resulted from high level significant harm in children. The aim is to classify, aggregate, and disseminate the trends arising from serious adverse events. In this way, clinicians can be close to real-time feedback on the key emerging safety trends in children’s health care across the state of NSW. Safety programs can then be designed to meet the needs of the most pressing safety concerns.
Adverse event reporting only captures a small percentage of actual safety events. Pediatric trigger tools have been found to be more effective than traditional incident management systems [3••, 4, 33, 34]. In the UK, the UK Pediatric Trigger Tool (UKPTT) has been developed as a way to measure harm in admitted pediatric patients [35]. The study, although retrospective, showed that there is a significant and measurable level of harm occurring to pediatric patients in the UK. The challenge going forward is for all countries to adopt similar trigger tool methodology to obtain a clearer sense of the levels of harm experienced by children admitted to hospitals in their countries. It is difficult to build a global culture of pediatric safety without a robust mechanism for measuring harm, collaborating on data, and sharing solutions and lessons learned.
One such organization that is taking up the challenge of global collaboration is PIPSQC. The Pediatric International Patient Safety and Quality Community is an informal international collaborative of professionals who share a passion for pediatric safety and quality (www.pipsqc.org). The aim of PIPSQC is to allow interaction across organizational, geographical, and international boundaries. Its mission is to hasten the delivery of safe health care to children worldwide. In order to achieve this mission, PIPSQC aims to stimulate interaction among members and member institutions and enable members to learn from one another through the sharing of best practice and generate tangible, measurable improvements in global patient safety.
Conclusion
The challenge to build a culture of safety in pediatrics and child health continues. To date, significant progress at a unit, hospital, national, and global level has been made. This paper has highlighted some key emerging themes and successes to date. It is up to the new generation of pediatric leaders to collaborate to ensure that the many challenges are met. The focus must always remain on the children that we care for as they deserve the very best and safest care possible.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Lachman P, Runnacles J, Dudley J. Equipped: overcoming barriers to change to improve quality of care. Arch Dis Child Educ Pract Ed. 2015;100(1):13–8. This paper highlights the obligation that health professionals need to provide reliable and safe care to all children all of the time. The key is develo** systems to do this.
Lachman P. Redefining the clinical gaze. BMJ Qual Saf. Online first 2 August 2014. Healthcare can be made safer by making child centered care and the safety of patients the key to develo** a high reliable systems approach.
Stockwell D, Bisarya H, Claasen D, et al. A trigger tool to detect harm in pediatric inpatient settings. Pediatrics. 2015;135(6):1593–4. Harm occurs at high rates in children and the trigger tool methodology provides the best way to understand how much harm is happening to children in hospital.
Carson Stevens A, Edwards A, Panesar S, et al. Reducing the burden of iatrogenic harm in children. Lancet. 2015;385(9978):1593–4.
Rees P, Edwards A, Panesar S, et al. Safety incidents in the primary care setting. Pediatrics. 2015;135(6):1027–35.
Collins A. http://www.health.org.uk/publications/measuring-what-really-matters/. Accessed April 2014.
Cilfra C, Jones K, Ascenzi J, et al. The morbidity and mortality conference as an adverse event surveillance tool in a pediatric intensive care unit. BMJ Qual Saf. 2014;23:930–8.
Scheifer J, Leonard D. Patient safety and quality improvement: an overview of QI. Paediatr Rev. 2012;33(8):353–9.
Runnucles J, Moult B, Lachman P. Develo** future clinical leaders for quality improvement: an experience from a London children’s hospital. BMJ Qual Saf. 2013;22(11):956–63. Strong clinical leadership is e key to develo** safe, effective microsystems for clinicians to work in.
Woodhead P, Lachman P, Mountford J, et al. From harm to hope and purposeful action: what could we do after Francis? BMJ Qual Saf. 2014;23:619–23. Up skilling and capacity building of front line clinical staff can lead to a sustainable benefit for patients and staff.
Lannon C, Levy F, Moyer C. The need to build capability and capacity in quality improvement and patient safety. Pediatrics. 2015;135(6):e1371–3.
Sexton J, Sharek P, Thomas E, et al. Exposure to leadership walk rounds in neonatal intensive care units is associated with a better patient safety culture and less caregiver burnout. BMJ Qual Saf. 2014;23:814–22.
Abrahamson E, Hyman D, Osorio S, Kaushal R. Implementing a patient safety and quality program across two merged pediatric institutions. Jt Comm J Qual Patient Saf. 2009;35(1):43–8.
Miller M, Robinson K, Lubomski L, et al. Medication errors in pediatric care: a systemic review of epidemiology and an evaluation of evidence supporting reduction strategy recommendations. Qual Saf Health Care. 2007;16(2):116–26.
Lepee C, Klaber R, Benn J, et al. The use of a consultant led ward round checklist to improve pediatric prescribing: an interrupted time series study. Eur J Paediatr. 2012;171(8):1239–45.
Goldenhar L, Brady P, Sutcliffe K, Mouthing S. Huddling for high reliability care. BMJ Qual Saf. 2013;22:899–906.
Mohr J, Betalden P, Barach P. Integrating patient safety into the clinical microsystem. Qual Saf Health Care. 2004;13 suppl 2:ii34–8.
Pronovost P, Armstrong C, Demski R, et al. Creating a high-reliability health care system: improving performance on core processes of care at John Hopkins Medicine. Acad Med. 2015;90(2):165–72.
Buck D, Kurth C, Varughese A. Perspectives on quality and safety in pediatric anesthesia. Anesthesiol Clin. 2014;32(1):281–94.
Parry G, Horowitz D, Goldmann D. Patient safety attitudes of pediatric trainee physicians. Qual Saf Health Care. 2009;18:462–6.
Bigham M, Logsdon T, Manicone P. Decreasing handoff- related care failures in children’s hospitals. Pediatrics. 2014;134(2):e572–9.
Hughes C, Pain C, Braithwaite J, Hillman K. Between the flags: implementing a rapid response system at scale. BMJ Qual Saf. 2014;23:714–7.
Brady P, Zix J, Brilli R. Develo** and evaluating the sources of a family activated medical emergency team: a quality improvement report. BMJ Qual Saf. 2015;24(3):203–11.
Cox E, Crayon P, Hansen K, et al. Parent perceptions of children’s hospital safety climate. BMJ Qual Saf. 2013;22:664–71.
Lachman P, Linkson L, Evans T, et al. Develo** person- centered analysis of harm in a pediatric hospital: a quality improvement report. BMJ Qual Saf. Online first 30 March 2015.
Bell S, Mann K, Truog R, Lantos J. Should we tell parents that we’ve made an error? Pediatrics. 2015;135(1):159–63.
Newland J, Banerjee R, Gerber J, et al. Antimicrobial stewardship in pediatric care: strategies and future directions. Pharmacotherapy. 2012;32:735–43.
Dellit T, Owens R, McGowan J, et al. Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America guidelines for develo** an institutional program to enhance antimicrobial stewardship. Clin Infect Dis. 2007;44(2):159–77.
Best A, Greenhalgh T, Lewis S, et al. Large-scale transformation in health care: a realist review. Millbank Q. 2012;90(3):421–56.
SAFE program –situational awareness for everyone. www.rcpch.ac.uk/improving-child-health/quality. Accessed May 2015.
Lennon C, Peterson L. Pediatric collaborative networks for quality improvement and research. Acad Pediatr. 2013;13(6):S69–74.
Taitz J, Genn K, Brooks V, et al. Qual Saf Health Care. Online first 29 July 2010.
Stockwell D, Bisarya H, Classen D, et al. Development of an electronic pediatric all-cause harm measurement tool using a modified Delphi method. J Patient S. Online first 26 August 2014.
Matlow A, Cronin C, Flintoft V, et al. Description of the development and validation the Canadian pediatric trigger tool. BMJ Qual Saf. 2011;20:416–23.
Chapman S, Fitzsimmons J, Davey N, Lachman P. Prevalence and severity of pediatric harm in a sample of UK-hospitalized children detected by the pediatric trigger tool. BMJ Open. 2014;4:e005066.
Compliance with Ethics Guidelines
Conflict of Interest
Jonny Taitz declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Patient Safety
Rights and permissions
About this article
Cite this article
Taitz, J. Building a Culture of Safety in Pediatrics and Child Health. Curr Treat Options Peds 1, 253–261 (2015). https://doi.org/10.1007/s40746-015-0032-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40746-015-0032-6