Abstract
Background
Data from diverse populations are needed to inform interventions for maternal health equity. However, research recruitment of postpartum individuals is challenging, especially in minoritized and structurally marginalized populations.
Materials and Methods
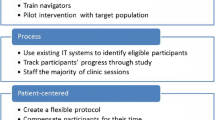
We developed a recruitment strategy for a cross-sectional survey among postpartum individuals at an urban safety-net hospital in New England, inclusive of those with a language preference other than English (LPOE) and those not attending scheduled postpartum visits. Recruitment was primarily conducted before, during, and after clinic visits in obstetrics or pediatrics. Surveys could be completed in-person, over the phone, or online. All study materials were trilingual (English, Spanish, Haitian Creole). After reaching our recruitment goal of 120 individuals, we analyzed our recruitment efforts to identify key recruitment strategies.
Results
From April to June 2022, 245 individuals were invited to participate, and 120 (49%) completed the survey, of whom 119 contributed recruitment data to the present analysis. Most participants (83.1%) self-identified as Black or Hispanic, and 30.2% had an LPOE. Compared with the overall sample, participants with an LPOE were more likely to have been recruited in-person (73% versus 78%), while those not attending postpartum visits required more outreach attempts (mean 2.3 versus 2.6). We identified 4 key strategies contributing to recruitment success: multilingual materials, frequent assessment and adjustment of our recruitment approach, pediatrics-based recruitment, and multiple timings and modes of outreach.
Conclusions
Using a multi-stage, multilingual, and multi-method recruitment strategy including pediatrics-based outreach, we recruited a diverse postpartum sample with > 80% individuals of color and > 30% with an LPOE. Our experience can inform more inclusive postpartum research.


Similar content being viewed by others
Data availability
Aggregated or de-identified data and code availability are available from the authors upon reasonable request.
References
Trost S, Beauregard J, Chandra G, Njie F, Berry J, Harvey A, et al. Pregnancy-related deaths: data from maternal mortality review committees in 36 US states, 2017–2019. Centers for Disease Control and Prevention: US Department of Health and Human Services. Atlanta, GA; 2022. Available from: https://www.cdc.gov/reproductivehealth/maternal-mortality/erase-mm/data-mmrc.html
Daw JR, Hatfield LA, Swartz K, Sommers BD. Women in the United States experience high rates of coverage ‘churn’ in months before and after childbirth. Health Aff (Millwood). 2017;36:598–606.
Cohen JL, Daw JR. Postpartum cliffs—missed opportunities to promote maternal health in the United States. JAMA Health Forum. 2021;2:e214164.
Nicklas JM, Skurnik G, Zera CA, Reforma LG, Levkoff SE, Seely EW. Employing a multi-level approach to recruit a representative sample of women with recent gestational diabetes mellitus into a randomized lifestyle intervention trial. Matern Child Health J. 2016;20:261–9.
Klerman JA, Daley K, Pozniak A. Family and medical leave in 2012: technical report. Contract #GS10F0086K. Abt Associates (US). Cambridge (MA) 2014; p 174. Available from: https://www.dol.gov/sites/dolgov/files/OASP/legacy/files/FMLA-2012-Technical-Report.pdf
American College of Obstetricians and Gynecologists. Optimizing postpartum care Committee Opinion No. 736. Obstet Gynecol. 2018;131:e140-50.
Vaughan SE, Misra DP, Wong AC, Rengers B, Jablonski S, Price M, et al. Successful recruitment strategies for engaging pregnant African American women in research. West J Nurs Res. 2022;44:94–100.
Murray Horwitz ME, Prifti CA, Battaglia TA, Ajayi A, Edwards CV, Benjamin EJ, et al. Pre-pregnancy cardiovascular disease risk factors and adverse pregnancy outcomes in a safety-net hospital. J Womens Health. 2023;32(4):401–8.
Placek CD, Place JM, Wies J. Reflections and challenges of pregnant and postpartum participant recruitment in the context of the opioid epidemic. Matern Child Health J. 2021;25:1031–5.
Grosser AM, Höller-Holtrichter C, Doyle I-M, Schmitz J, Hoffmann R, Ergin-Akkoyun E, et al. Strategies for recruiting women with migration history using the example of the BaBi-Birth Cohort Study. Gesundheitswesen Bundesverb Arzte Offentlichen Gesundheitsdienstes Ger. 2019;81:621–8.
Peindl KS, Wisner KL. Successful recruitment strategies for women in postpartum mental health trials. J Psychiatr Res. 2003;37:117–25.
Beasley LO, Ciciolla L, Jespersen JE, Chiaf AL, Schmidt M, Shreffler KM, et al. Best practices for engaging pregnant and postpartum women at risk of substance use in longitudinal research studies: a qualitative examination of participant preferences. Advers Resil Sci. 2020;1:235–46.
Wolf ER, Hochheimer CJ, Sabo RT, DeVoe J, Wasserman R, Geissal E, et al. Gaps in well-child care attendance among primary care clinics serving low-income families. Pediatrics. 2018;142:e20174019.
Acknowledgements
The authors gratefully acknowledge the individuals who were recruited for the survey.
Funding
MEMH was supported by Boston University Chobanian and Avedisian School of Medicine, Boston University Chobanian and Avedisian School of Medicine Department of Medicine Career Investment Award, and the American Heart Association Career Development Award 937987. TAB was supported by Boston University Clinical and Translational Science Institute through a grant from the National Institutes of Health 1UL1TR001430. The funders had no role in the survey’s design, implementation, or analysis. The funders had no role in the survey’s design, implementation, or analysis.
Author information
Authors and Affiliations
Contributions
M.E.M.H.: conceptualization; methodology; investigation; formal analysis; writing, original draft and review and editing; visualization; project administration; and funding acquisition. G.S.B.: investigation; resources; writing, review and editing; visualization; and project administration. J.A.S.: investigation and writing, original draft and review and editing. T.A.B.: conceptualization; methodology; writing, review and editing; and supervision.
Corresponding author
Ethics declarations
Ethics Approval
The research was conducted in accord with prevailing ethical principles and was deemed exempt by the Boston University Institutional Review Board (Application H-43387) based on its use of secondary and de-identified data.
Consent to Participate
All persons gave their informed consent prior to their inclusion in the survey; however, it was not feasible to obtain informed consent prior to recruitment nor was it feasible to obtain informed consent prior to this secondary data analysis.
Consent for Publication
Not applicable.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Murray Horwitz, M.E., Saradjha Brédy, G., Schemm, J.A. et al. Strategies for Recruiting a Diverse Postpartum Survey Sample. J. Racial and Ethnic Health Disparities (2023). https://doi.org/10.1007/s40615-023-01886-x
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40615-023-01886-x