Abstract
Background
Frailty is a significant concern among hospitalized older adults, influenced by multiple factors. Understanding the complex interactions between these variables can be facilitated through a network perspective.
Aim
This study aimed to identify the core factor and physiological indicator of frailty in hospitalized elderly patients and visualize their interactions within the network structure.
Methods
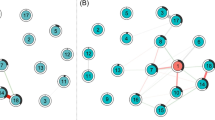
Frailty was assessed using the Tilburg Frailty Indicators, with a score of 5 or higher indicating frailty. Additional variables related to sociodemographic, physical and clinical, psychological and cognitive aspects, as well as physiological indicators, were extracted from electronic health records. A partial correlation network analysis was conducted using an adaptive LASSO algorithm, based on univariate correlation and logistic regression, to examine the network structure and identify influential nodes.
Results
The average age of participants was 70.74 ± 7.52 years, with 24.27% classified as frail. Frailty was associated with 38 of 145 initially included variables (P < 0.05). The network analysis revealed depression as the most central node, followed by drugs used, sleep disorders, loneliness, masticatory obstacles, drinking, and number of teeth missing. Hemoglobin emerged as the most central biochemical indicator in the network, based on network center index analysis (Strength = 4.858, Betweenness = 223, Closeness = 0.034).
Conclusions
Frailty in hospitalized older adults is influenced by various social, physical, and psychological factors, with depression as the core factor of utmost importance. Changes in hemoglobin levels could serve as an essential indicator. This innovative network approach provides insights into the multidimensional structure and relationships in real-world settings.



Similar content being viewed by others
Availability of data and materials
The data that support the findings of this study are not openly available due to reasons of sensitivity and are available from the corresponding author upon reasonable request.
References
Padeiro M, Santana P, Grant M (2023) Global aging and health determinants in a changing world. In: Oliveira PJ, Malva JO (eds) Aging. Academic Press, pp 3–30
Howlett SE, Rutenberg AD, Rockwood K (2021) The degree of frailty as a translational measure of health in aging. Nat Aging 1:651–665. https://doi.org/10.1038/s43587-021-00099-3
Hoogendijk EO, Afilalo J, Ensrud KE et al (2019) Frailty: implications for clinical practice and public health. Lancet 394:1365–1375. https://doi.org/10.1016/S0140-6736(19)31786-6
Ethun CG, Bilen MA, Jani AB (2017) Frailty and cancer: implications for oncology surgery, medical oncology, and radiation oncology. CA Cancer J Clin 67:362–377. https://doi.org/10.3322/caac.21406
Cesari M, Calvani R, Marzetti E (2017) Frailty in older persons. Clin Geriatr Med 33:293–303. https://doi.org/10.1016/j.cger.2017.02.002
Rockwood K (2005) Frailty and its definition: a worthy challenge. J Am Geriatr Soc 53:1069–10670. https://doi.org/10.1111/j.1532-5415.2005.53312.x
Satake S, Arai H (2020) Chapter 1 frailty: definition, diagnosis, epidemiology. Geriatr Gerontol Int 20:7–13. https://doi.org/10.1111/ggi.13830
The Lancet (2019) Bringing frailty into all realms of medicine. Lancet 394:1298. https://doi.org/10.1016/S0140-6736(19)32279-2
He B, Ma Y, Wang C et al (2019) Prevalence and risk factors for frailty among community-dwelling older people in China: a systematic review and meta-analysis. J Nutr Health Aging 23:442–450. https://doi.org/10.1007/s12603-019-1179-9
Zhang XM, Jiao J, Cao J et al (2022) The association between the number of teeth and frailty among older nursing home residents: a cross-sectional study of the CLHLS survey. BMC Geriatr 22:1007. https://doi.org/10.1186/s12877-022-03688-y
Vu HT, Nguyen TX, Nguyen TN et al (2017) Prevalence of frailty and its associated factors in older hospitalised patients in Vietnam. BMC Geriatr 17:216. https://doi.org/10.1186/s12877-017-0609-y
Ozturk ZA, Ozdemir S, Turkbeyler IH et al (2017) Quality of life and fall risk in frail hospitalized elderly patients. Turk J Med Sci 47:1377–1383. https://doi.org/10.3906/sag-1610-107
Hao Q, Zhou L, Dong B et al (2019) The role of frailty in predicting mortality and readmission in older adults in acute care wards: a prospective study. Sci Rep 9:1207. https://doi.org/10.1038/s41598-018-38072-7
Nguyen AT, Nguyen TX, Nguyen TN et al (2019) The impact of frailty on prolonged hospitalization and mortality in elderly inpatients in Vietnam: a comparison between the frailty phenotype and the reported Edmonton frail scale. Clin Interv Aging 14:38–388. https://doi.org/10.2147/CIA.S189122
Sikder T, Sourial N, Maimon G et al (2019) Postoperative recovery in frail, pre-frail, and non-frail elderly patients following abdominal surgery. World J Surg 43:415–424. https://doi.org/10.1007/s00268-018-4801-9
Gilbert T, Neuburger J, Kraindler J et al (2018) Development and validation of a Hospital Frailty Risk Score focusing on older people in acute care settings using electronic hospital records: an observational study. Lancet 391:1775–1782. https://doi.org/10.1016/S0140-6736(18)30668-8
Oliveira DR, Bettinelli LA, Pasqualotti A et al (2013) Prevalence of frailty syndrome in old people in a hospital institution. Rev Lat Am Enfermagem 21:891–898. https://doi.org/10.1590/S0104-11692013000400009
Pilotto A, Custodero C, Maggi S et al (2020) A multidimensional approach to frailty in older people. Ageing Res Rev 60:101047. https://doi.org/10.1016/j.arr.2020.101047
Leme DEDC, Alves EVDC, Fattori A (2020) Relationships between social, physical, and psychological factors in older persons: frailty as an outcome in network analysis. J Am Med Dir Assoc 21:1309–1315. https://doi.org/10.1016/j.jamda.2020.02.005
Rezaei-Shahsavarloo Z, Atashzadeh-Shoorideh F, Gobbens RJ et al (2020) The impact of interventions on management of frailty in hospitalized frail older adults: a systematic review and meta-analysis. BMC Geriatr 20:1–7. https://doi.org/10.1186/s12877-020-01935-8
Holman MS, Williams MN (2022) Suicide risk and protective factors: a network approach. Arch Suicide Res 26:137–154. https://doi.org/10.1080/13811118.2020.1774454
Blanchard MA, Roskam I, Mikolajczak M et al (2021) A network approach to parental burnout. Child Abuse Negl 111:104826. https://doi.org/10.1016/j.chiabu.2020.104826
Epskamp S, Borsboom D, Fried EI (2018) Estimating psychological networks and their accuracy: a tutorial paper. Behav Res Methods 50:195–212. https://doi.org/10.3758/s13428-017-0862-1
Kalgotra P, Sharda R, Croff JM (2017) Examining health disparities by gender: a multimorbidity network analysis of electronic medical record. Int J Med Inform 108:22–28. https://doi.org/10.1016/j.ijmedinf.2017.09.014
Zhu Z, **ng W, Hu Y et al (2021) Paradigm shift: moving from symptom clusters to symptom networks. Asia Pac J Oncol Nurs 9:5–6. https://doi.org/10.1016/j.apjon.2021.12.001.26
Dong L, Liu N, Tian X et al (2017) Reliability and validity of the Tilburg Frailty Indicator (TFI) among Chinese community-dwelling older people. Arch Gerontol Geriatr 73:21–28. https://doi.org/10.1016/j.archger.2017.07.001
Gobbens RJ, van Assen MA, Luijkx KG et al (2010) The Tilburg Frailty Indicator: psychometric properties. J Am Med Dir Assoc 11:344–355. https://doi.org/10.1016/j.jamda.2009.11.003
Zheng W, Hu M, Liu Y (2022) Social support can alleviate the fear of cancer recurrence in postoperative patients with lung carcinoma. Am J Transl Res 14:4804–4811
Xu R, Zhou X, Cao S et al (2019) Health status of the elderly and its influence on their activities of daily living in Shangrao, Jiangxi province. Int J Environ Res Public Health 16:1771. https://doi.org/10.3390/ijerph16101771
Bahl V, Hu HM, Henke PK et al (2010) A validation study of a retrospective venous thromboembolism risk scoring method. Ann Surg 251:344–350. https://doi.org/10.1097/SLA.0b013e3181b7fca6
Qiao X, Ji L, Si H et al (2022) Validation and comparison of three short depression screening tools among Chinese community-dwelling older adults. Res Gerontol Nurs 15:283–291. https://doi.org/10.3928/19404921-20220929-01
Katzman R, Zhang MY, Ouang Ya Q et al (1988) A Chinese version of the Mini-mental state examination; impact of illiteracy in a Shanghai dementia survey. J Clin Epidemiol 41:971–978. https://doi.org/10.1016/0895-4356(88)90034-0
Bringmann LF, Elmer T, Epskamp S et al (2019) What do centrality measures measure in psychological networks? J Abnorm Psychol 128:892–903. https://doi.org/10.1037/abn0000446
Heckerman D (2008) A tutorial on learning with Bayesian networks. Innovations in Bayesian networks: theory and applications. Springer, pp 33–82
Zhang Q, Guo H, Gu H et al (2018) Gender-associated factors for frailty and their impact on hospitalization and mortality among community-dwelling older adults: a cross-sectional population-based study. PeerJ 6:e4326. https://doi.org/10.7717/peerj.4326
Miyamura K, Fhon JRS, Bueno AA et al (2019) Frailty syndrome and cognitive impairment in older adults: systematic review of the literature. Rev Lat Am Enfermagem 27:e3202. https://doi.org/10.1590/1518-8345.3189.3202
Auyeung TW, Lee JS, Kwok T et al (2011) Physical frailty predicts future cognitive decline—a four-year prospective study in 2737 cognitively normal older adults. J Nutr Health Aging 15:690–694
Liu W, Puts M, Jiang F et al (2020) Physical frailty and its associated factors among elderly nursing home residents in China. BMC Geriatr 20:294. https://doi.org/10.1186/s12877-020-01695-5
Xu L, Zhang J, Shen S et al (2021) Clinical frailty scale and biomarkers for assessing frailty in elder inpatients in China. J Nutr Health Aging 25:77–83. https://doi.org/10.1007/s12603-020-1455-8
Andrade JM, Duarte YAO, Alves LC et al (2018) Frailty profile in Brazilian older adults: ELSI-Brazil. Rev Saude Publica. https://doi.org/10.11606/S1518-8787.2018052000616
Buttery AK, Busch MA, Gaertner B et al (2015) Prevalence and correlates of frailty among older adults: findings from the German health interview and examination survey. BMC Geriatr 15:22. https://doi.org/10.1186/s12877-015-0022-3. (Published 2015 Mar 8)
Pokorny JJ, Norman A, Zanesco AP et al (2018) Network analysis for the visualization and analysis of qualitative data. Psychol Methods 23:169–183. https://doi.org/10.1037/met0000129
Borsboom D, Cramer AO (2013) Network analysis: an integrative approach to the structure of psychopathology. Annu Rev Clin Psychol 9:91–121. https://doi.org/10.1146/annurev-clinpsy-050212-185608
Buigues C, Padilla-Sánchez C, Garrido JF et al (2015) The relationship between depression and frailty syndrome: a systematic review. Aging Ment Health 19:762–772
Lim EJ (2020) Sex differences in factors affecting depressive symptoms in older people in the prefrailty phase. Int J Environ Res Public Health 17:4207. https://doi.org/10.3390/ijerph17124207
Prina AM, Stubbs B, Veronese N et al (2019) Depression and incidence of frailty in older people from six Latin American Countries. Am J Geriatr Psychiatry 27:1072–1079. https://doi.org/10.1016/j.jagp.2019.04.008
Mezuk B, Lohman M, Dumenci L et al (2013) Are depression and frailty overlap** syndromes in mid-and late-life? a latent variable analysis. Am J Geriatr Psychiatry 21:560–569
Ni Lochlainn M, Cox NJ, Wilson T et al (2021) Nutrition and frailty: opportunities for prevention and treatment. Nutrients 13:2349. https://doi.org/10.3390/nu13072349
Bonnefoy M, Berrut G, Lesourd B et al (2015) Frailty and nutrition: searching for evidence. J Nutr Health Aging 19:250–257. https://doi.org/10.1007/s12603-014-0568-3
Xu L, Zhang J, Shen S et al (2020) Association between body composition and frailty in elder inpatients. Clin Interv Aging 15:313–320. https://doi.org/10.2147/CIA.S243211
Liang H, Li X, Lin X et al (2021) The correlation between nutrition and frailty and the receiver operating characteristic curve of different nutritional indexes for frailty. BMC Geriatr 21:619. https://doi.org/10.1186/s12877-021-02580-5
Keller U (2019) Nutritional laboratory markers in malnutrition. J Clin Med 8:775. https://doi.org/10.3390/jcm8060775
van Wijngaarden JP, Wojzischke J, van den Berg C et al (2020) Effects of nutritional interventions on nutritional and functional outcomes in geriatric rehabilitation patients: a systematic review and meta-analysis. J Am Med Dir Assoc 21:1207-1215.e9. https://doi.org/10.1016/j.jamda.2020.04.012
Cruz-Jentoft AJ, Kiesswetter E, Drey M et al (2017) Nutrition, frailty, and sarcopenia. Aging Clin Exp Res 29:43–48. https://doi.org/10.1007/s40520-016-0709-0
de Morais Fabrício D, Chagas MHN, Diniz BS (2020) Frailty and cognitive decline. Transl Res 221:58–64
Brigola AG, Ottaviani AC, Carvalho DHT et al (2020) Association between cognitive impairment and criteria for frailty syndrome among older adults. Arq Neuropsiquiatr 78:02–08
Freitas S, Simões MR et al (2013) Montreal cognitive assessment: validation study for mild cognitive impairment and Alzheimer disease. Alzheimer Dis Assoc Disord 27:37–43
Izquierdo M, Merchant RA, Morley JE et al (2021) International exercise recommendations in older adults (ICFSR): expert consensus guidelines. J Nutr Health Aging 25:824–853
Taylor JA, Greenhaff PL, Bartlett DB et al (2023) Multisystem physiological perspective of human frailty and its modulation by physical activity. Physiol Rev 103:1137–1191
Motta F, Sica A, Selmi C (2020) Frailty in rheumatic diseases. Front Immunol 11:576134
Mielke N, Schneider A, Huscher D et al (2022) Gender differences in frailty transition and its prediction in community-dwelling old adults. Sci Rep 12:7341
Zhao J, Liu YWJ, Tyrovolas S et al (2023) Exploring the concept of psychological frailty in older adults: a systematic sco** review. J Clin Epidemiol 159:300–308. https://doi.org/10.1016/j.jclinepi.2023.05.005
Funding
Key Medical Specialty funded by Shanghai Fifth People’s Hospital, Fudan University (No.2020WYZDZK10). Scientific Research Project funded by Shanghai Fifth People’s Hospital, Fudan University (No.2022WYHLZD01). Natural Science Research Funds of Minhang District, Shanghai ( No.2023MHZ031).
Author information
Authors and Affiliations
Contributions
RQ: methodology, validation, investigation, data curation, writing—original draft, writing—review and editing. YG: conceptualization, methodology, resources, supervision, project administration, funding acquisition, writing—review and editing.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that there are no conflicts of interest. We would like to thank the participating elderly patients for their help and efforts in the data collection process.
Statement of human and animal rights
All data analysed here were collected as part of routine diagnosis and treatment. We informed our local ethical committee of this observational research. No animal was used for this study.
Ethical approval and consent to participate
The study protocol was approved by the Institutional Ethics Committee (Ethical Approval Form no. 2022-130) and adhered to the principles of the Declaration of Helsinki. Written informed consent was obtained from each patient before data collection.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Qiu, R., Gu, Y. Network analysis of frailty indicators in hospitalized elderly patients: unveiling the role of depression and hemoglobin as core factors. Aging Clin Exp Res 35, 3189–3203 (2023). https://doi.org/10.1007/s40520-023-02608-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-023-02608-3