Abstract
Purpose
Several studies have reported thromboembolic events to be common in severe COVID-19 cases. We sought to investigate the relationship between lung ultrasound (LUS) findings in hospitalized COVID-19 patients and the development of venous thromboembolic events (VTE).
Methods
A total of 203 adults were included from a COVID-19 ward in this prospective multi-center study (mean age 68.6 years, 56.7% men). All patients underwent 8-zone LUS, and all ultrasound images were analyzed off-line blinded. Several LUS findings were investigated (total number of B-lines, B-line score, and LUS-scores).
Results
Median time from admission to LUS examination was 4 days (IQR: 2, 8). The median number of B-lines was 12 (IQR: 8, 18), and 44 (21.7%) had a positive B-line score. During hospitalization, 17 patients developed VTE (4 deep-vein thrombosis, 15 pulmonary embolism), 12 following and 5 prior to LUS. In fully adjusted multivariable Cox models (excluding participants with VTE prior to LUS), all LUS parameters were significantly associated with VTE (total number of B-lines: HR = 1.14, 95% CI (1.03, 1.26) per 1 B-line increase), positive B-line score: HR = 9.79, 95% CI (1.87, 51.35), and LUS-score: HR = 1.51, 95% CI (1.10, 2.07), per 1-point increase). The B-line score and LUS-score remained significantly associated with VTE in sensitivity analyses.
Conclusion
In hospitalized COVID-19 patients, pathological LUS findings were common, and the total number of B-lines, B-line score, and LUS-score were all associated with VTE. These findings indicate that the LUS examination may be useful in risk stratification and the clinical management of COVID-19. These findings should be considered hypothesis generating.
Clinicaltrials.gov ID
NCT04377035
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
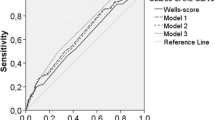
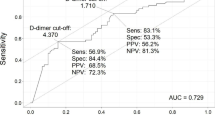
COVID-19 is associated with the development of acute respiratory distress syndrome (ARDS), intensive care unit admission, multi-organ failure, and death, especially in the elderly [Relationship between LUS-score and echocardiographic parameters The relationships between LUS-score and conventional echocardiographic left and right ventricular parameters were assessed with univariable linear regression models. High LUS-score was not associated with elevated TR gradient (stand. β.coefficient: 0.16, P = 0.051), elevated E/E’ (stand. β.coefficient: 0.00, P = 0.99), reduced LVEF (stand. β.coefficient: − 0.03, P = 0.74) or reduced TAPSE (stand. β.coefficient: − 0.11, P = 0.14). Uni- and multivariable Cox and logistic regression models investigating the association between LUS findings (number of B-lines, B-line score, and LUS-score) and VTE are listed in Table 2. In univariable Cox (only VTE cases following the LUS examination) and logistic (all cases of VTE) regressions, an increasing number of B-lines, positive B-line score, and LUS-score were all significant markers of outcome. Number of B-lines was significantly associated with higher risk of VTE in multivariable Cox regression (HR = 1.14, 95% CI (1.03, 1.26), P = 0.016, per 1 B-line increase). This was also the case in multivariable logistic regression (OR = 1.09, 95% CI (1.01, 1.19), P = 0.038, per 1 B-line increase). B-line score also remained a significant marker of VTE during hospitalization in both multivariable Cox and logistic regression models (Cox regression: (HR = 9.79, 95% CI (1.87, 51.35), P = 0.007; logistic regression: OR = 6.10, 95% CI (1.69, 22.05), P = 0.006). Finally, LUS-score remained independently associated with VTE during hospitalization in the fully adjusted models (Cox regression: HR = 1.51, 95% CI (1.10, 2.07), P = 0.010 per 1-point increase; logistic regression: OR = 1.39, 95% CI (1.09, 1.79), P = 0.009, per 1-point increase). The associations between LUS findings and VTE are illustrated in Fig. 2. Association between LUS findings and future VTE during hospitalization. Displaying the unadjusted incidence rates of VTE during hospitalization for COVID-19 (with 95% confidence intervals) for the population in relation to total number of B-lines (A) and LUS-score (B). LUS lung ultrasonography, VTE venous thromboembolic event Three sensitivity analyses were conducted using the same multivariable model. B-line score and LUS-score both remained significantly associated with the outcome in all sensitivity analyses. Meanwhile, the total number of B-lines only remained significant in logistic regression sensitivity analysis 2 and 3, (Table 2). Optimal cutoff values for total number of B-lines and LUS-score were found to be, respectively, ≥ 15 B-lines and a LUS-score ≥ 5. The cutoff value for total number of B-lines demonstrated a sensitivity of 58.8% (IQR: 32.9; 81.6) and specificity of 76.1% (69.6; 81.9). Meanwhile, a positive B-line score had a sensitivity of 52.9% (IQR: 27.8; 77) and specificity of 82.2% (IQR: 76.2; 87.3). Finally, a LUS-score ≥ 5 had a sensitivity and specificity of, respectively, 58.8% (IQR: 32.9; 81.6) and specificity of 76.1% (69.6; 81.9).Relationship between LUS findings and VTE
Discussion
The present study was designed with the objective of assessing the association between lung ultrasound findings and development of VTE in hospitalized COVID-19 patients. We particularly aimed to assess the association between LUS findings and development of VTE, as several studies have coupled the severity of the SARS-CoV-2 infection with LUS findings [28, 29]. One retrospective cohort study investigated whether LUS could be used to detect COVID-19 in 42 patients with COVID-19 and 24 controls without COVID-19. In that study, the B-line score had a similar sensitivity to detect COVID-19 than chest X-ray and CT and improved specificity compared to chest radiograph [29]. However, the sample size was quite small, and they did not investigate how LUS findings were associated with the development of VTE. The results described in a systematic review[28] looking at the utility of LUS in COVID-19 suggest that LUS findings are very common in COVID-19 and that their mere presence in themselves may help detect COVID-19 but are not optimal for risk stratification. Rather, it seems the cumulative amount of LUS findings (B-lines, subpleural and lobar consolidations) may be more useful as a tool for risk stratification in hospitalized patients with COVID-19.
Using only the total number of B-lines may be inadequate as we observed many cases of confluent B-lines and subpleural and lobar consolidations, making it difficult to count the number of B-lines correctly. It seems the LUS findings in COVID-19 are numerous, and we, therefore, suggest a scoring system of the kind presented in this study to account for both the number of zones affected and the possibility of multiple LUS findings per zone. A scoring system like this requires external validation, but we hope that the present study can be hypothesis generating for future LUS studies in COVID-19 and help in elucidating the prognostic potential of LUS in COVID-19.
While we in the present study have found that LUS findings were associated with VTE, the study cannot answer the question of causality as there is a potential risk of reverse causation. That is, it may be that our LUS findings are present due to VTE instead of LUS findings occurring prior to later development of VTE. We used both Cox proportional hazard regression with the outcome being restricted to VTE diagnosed after the LUS examination and logistic regression with the outcome being development of VTE during the entire hospitalization as to observe possible differences that could be due to reverse causation. However, regardless of the method used to analyze the data, LUS findings were significantly associated with the outcome in both scenarios and remained so even after adjusting for possible confounding parameters.
In the present study, we observe that the patients who developed VTE had a higher number of pathological LUS findings. What the LUS detects is increased density of the lung parenchyma most likely due to inflammation related to pneumonitis rather than lung infarction due to emboli which is usually seen as triangular, hypoechoic, subpleural consolidations. Though, diffuse pulmonary intravascular coagulopathy also adds to the increased density of the parenchyma. Our findings suggest that patients who develop VTE have a more severe pneumonitis and probably also increased endotheliitis. Thus, the risk of develo** VTE is related to the clinical stage and severity of the disease and not to the extent of the pathological findings itself.
We used an 8-zone model as has previously been recommended [30] in our study. The lower lateral zones are, however, known to be difficult to obtain, in patients with prevalent respiratory failure in the semi-recumbent position. We, therefore, carried out sensitivity analyses to make sure that our results were not driven by inadequate lower lateral image clips in patients with the worst respiratory function. Still, the LUS findings remained significantly associated with the outcome in the majority of sensitivity analyses underscoring that our findings were not driven by differences in missing LUS zones. As the association between LUS findings and VTE remained significant in a 6-zone model, a lower number of zones may suffice in the clinical setting. However, further studies are needed to confirm this observation.
Strengths and limitations
This study is limited by a relatively small sample size. However, we used a multi-center design in which we included patients from all hospitals (8 hospitals) in Eastern Denmark. The multi-center design further strengthens our results as it makes our sample population much more representative of the general population. An important limitation to this study is that the observative design meant that not all participants had a CT angiography performed and thus some of the patients in the non-VTE group may actually have had an undetected VTE. As many of the patients had severe respiratory distress, the LUS examination was at times difficult to perform, especially in the lower lateral zones. Due to this, some of the patients had inadequate lower lateral zones for LUS analysis. In addition, many of the patients were too ill to collaborate to be in a seated position. All of this meant that we chose not to use a 12-zone LUS model which would otherwise have allowed us to assess the posterior zones and instead chose to only assess 8 zones (frontal and lateral zones) which limits our findings although the 8-zone model has been successfully used in several other studies [31, 32]. However, several sensitivity analyses were carried out which confirmed our findings in the primary analyses. A low-frequency probe was used for the study; however, a higher frequency probe would have improved resolution and may have aided in identifying even smaller subpleural consolidations which may have been missed. Due to the relatively small sample size, the number of events was low. However, our results remained stable in several different multivariable regression models and sensitivity models. Lastly, an important limitation is the variability in days from admission to LUS examination. A small team of investigators visiting two of the eight sites each day meant that each site was visited twice per week. Due to this approach, the median time from admission to ultrasound examination was 4 days, and as a result, a subset of our cohort probably represents a subset of COVID-19 patients requiring a longer hospital stay. This limits the generalizability of our results as they most likely reflect patients requiring longer hospital stays. The LUS investigators were experts in ultrasound and physicians without LUS experience may demonstrate poorer diagnostic performance. However, acquisition of LUS images is fairly simple and B-lines are easily recognized.
Conclusion
In hospitalized COVID-19 patients, pathological LUS findings were common, and the total number of B-lines, B-line score, and LUS-score were all associated with VTE. These findings indicate that the LUS examination may be useful in risk stratification and the clinical management of COVID-19. These findings should be considered hypothesis generating.
Data availability
Data are available upon request.
Code availability
Coding is available upon request.
References
Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, Qiu Y, Wang J, Liu Y, Wei Y, **a J, Yu T, Zhang X, Zhang L (2020) Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 395:507–513. https://doi.org/10.1016/S0140-6736(20)30211-7
Totura AL, Baric RS (2012) SARS coronavirus pathogenesis: host innate immune responses and viral antagonism of interferon. Curr Opin Virol 2:264–275. https://doi.org/10.1016/j.coviro.2012.04.004
Guan W-J, Ni Z-Y, Hu Y, Liang W-H, Ou C-Q, He J-X, Liu L, Shan H, Lei C-L, Hui DSC, Du B, Li L-J, Zeng G, Yuen K-Y, Chen R-C, Tang C-L, Wang T, Chen P-Y, **ang J, Li S-Y, Wang J-L, Liang Z-J, Peng Y-X, Wei L, Liu Y, Hu Y-H, Peng P, Wang J-M, Liu J-Y, Chen Z, Li G, Zheng Z-J, Qiu S-Q, Luo J, Ye C-J, Zhu S-Y, Zhong N-S (2020) China medical treatment expert group for Covid-19, clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 382:1708–1720. https://doi.org/10.1056/NEJMoa2002032
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, **ang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B (2020) Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395:1054–1062. https://doi.org/10.1016/S0140-6736(20)30566-3
Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, **ang H, Cheng Z, **ong Y, Zhao Y, Li Y, Wang X, Peng Z (2020) Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. https://doi.org/10.1001/jama.2020.1585
Tang N, Li D, Wang X, Sun Z (2020) Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost 18:844–847. https://doi.org/10.1111/jth.14768
Fox SE, Akmatbekov A, Harbert JL, Li G, Quincy Brown J, Vander Heide RS (2020) Pulmonary and cardiac pathology in African American patients with COVID-19: an autopsy series from New Orleans. Lancet Respir Med. https://doi.org/10.1016/S2213-2600(20)30243-5
Cui S, Chen S, Li X, Liu S, Wang F (2020) Prevalence of venous thromboembolism in patients with severe novel coronavirus pneumonia. J Thromb Haemost 18:1421–1424. https://doi.org/10.1111/jth.14830
Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers D, Kant KM, Kaptein FHJ, van Paassen J, Stals MAM, Huisman MV, Endeman H (2020) Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: An updated analysis. Thromb Res 191:148–150. https://doi.org/10.1016/j.thromres.2020.04.041
Stoneham SM, Milne KM, Nuttall E, Frew GH, Sturrock BR, Sivaloganathan H, Ladikou EE, Drage S, Phillips B, Chevassut TJ, Eziefula AC (2020) Thrombotic risk in COVID-19: a case series and case-control study. Clin Med (Lond) 20:e76–e81. https://doi.org/10.7861/clinmed.2020-0228
Flor N, Tonolini M (2020) From ground-glass opacities to pulmonary emboli. A snapshot of the evolving role of a radiology unit facing the COVID-19 outbreak. Clin Radiol 75:556–557. https://doi.org/10.1016/j.crad.2020.04.009
Middeldorp S, Coppens M, van Haaps TF, Foppen M, Vlaar AP, Müller MCA, Bouman CCS, Beenen LFM, Kootte RS, Heijmans J, Smits LP, Bonta PI, van Es N (2020) Incidence of venous thromboembolism in hospitalized patients with COVID-19. J Thromb Haemost 18:1995–2002. https://doi.org/10.1111/jth.14888
McGonagle D, Sharif K, O’Regan A, Bridgewood C (2020) The role of cytokines including interleukin-6 in COVID-19 induced pneumonia and macrophage activation syndrome-like disease. Autoimmun Rev 19:102537. https://doi.org/10.1016/j.autrev.2020.102537
McGonagle D, O’Donnell JS, Sharif K, Emery P, Bridgewood C (2020) Immune mechanisms of pulmonary intravascular coagulopathy in COVID-19 pneumonia. Lancet Rheumatol 2:e437–e445. https://doi.org/10.1016/S2665-9913(20)30121-1
Tavazzi G, Civardi L, Caneva L, Mongodi S, Mojoli F (2020) Thrombotic events in SARS-CoV-2 patients: an urgent call for ultrasound screening. Intensive Care Med 46:1121–1123. https://doi.org/10.1007/s00134-020-06040-3
Nazerian P, Volpicelli G, Vanni S, Gigli C, Betti L, Bartolucci M, Zanobetti M, Ermini FR, Iannello C, Grifoni S (2015) Accuracy of lung ultrasound for the diagnosis of consolidations when compared to chest computed tomography. Am J Emerg Med 33:620–625. https://doi.org/10.1016/j.ajem.2015.01.035
Volpicelli G, Elbarbary M, Blaivas M, Lichtenstein DA, Mathis G, Kirkpatrick AW, Melniker L, Gargani L, Noble VE, Via G, Dean A, Tsung JW, Soldati G, Copetti R, Bouhemad B, Reissig A, Agricola E, Rouby JJ, Arbelot C, Liteplo A, Sargsyan A, Silva F, Hoppmann R, Breitkreutz R, Seibel A, Neri L, Storti E, Petrovic T (2012) International liaison committee on lung ultrasound (ILC-LUS) for international conference consensus on lung ultrasound (ICC-LUS), International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med 38:577–591. https://doi.org/10.1007/s00134-012-2513-4
Hu L, Wang C (2020) Radiological role in the detection, diagnosis and monitoring for the coronavirus disease 2019 (COVID-19). Eur Rev Med Pharmacol Sci 24:4523–4528. https://doi.org/10.26355/eurrev_202004_21035
Volpicelli G, Lamorte A, Villén T (2020) What’s new in lung ultrasound during the COVID-19 pandemic. Intensive Care Med. https://doi.org/10.1007/s00134-020-06048-9
Shi H, Han X, Jiang N, Cao Y, Alwalid O, Gu J, Fan Y, Zheng C (2020) Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis 20:425–434. https://doi.org/10.1016/S1473-3099(20)30086-4
Pan F, Ye T, Sun P, Gui S, Liang B, Li L, Zheng D, Wang J, Hesketh RL, Yang L, Zheng C (2020) Time course of lung changes at chest CT during recovery from coronavirus disease 2019 (COVID-19). Radiology 295:715–721. https://doi.org/10.1148/radiol.2020200370
**ng C, Li Q, Du H, Kang W, Lian J, Yuan L (2020) Lung ultrasound findings in patients with COVID-19 pneumonia. Crit Care 24:174. https://doi.org/10.1186/s13054-020-02876-9
Sultan LR, Sehgal CM (2020) A review of early experience in lung ultrasound in the diagnosis and management of COVID-19. Ultrasound Med Biol. https://doi.org/10.1016/j.ultrasmedbio.2020.05.012
Lassen MCH, Skaarup KG, Lind JN, Alhakak AS, Sengeløv M, Nielsen AB, Espersen C, Ravnkilde K, Hauser R, Schöps LB, Holt E, Johansen ND, Modin D, Djernaes K, Graff C, Bundgaard H, Hassager C, Jabbari R, Carlsen J, Lebech A-M, Kirk O, Bodtger U, Lindholm MG, Joseph G, Wiese L, Schiødt FV, Kristiansen OP, Walsted ES, Nielsen OW, Madsen BL, Tønder N, Benfield T, Jeschke KN, Ulrik CS, Knop F, Lamberts M, Sivapalan P, Gislason G, Marott JL, Møgelvang R, Jensen G, Schnohr P, Søgaard P, Solomon SD, Iversen K, Jensen JUS, Schou M, Biering-Sørensen T (2020) Echocardiographic abnormalities and predictors of mortality in hospitalized COVID-19 patients: the ECHOVID-19 study. ESC Heart Fail. https://doi.org/10.1002/ehf2.13044
Skaarup KG, Lassen MCH, Lind JN, Alhakak AS, Sengeløv M, Nielsen AB, Espersen C, Hauser R, Schöps LB, Holt E, Johansen ND, Modin D, Sharma S, Graff C, Bundgaard H, Hassager C, Jabbari R, Lebech A-M, Kirk O, Bødtger U, Lindholm MG, Joseph G, Wiese L, Schiødt FV, Kristiansen OP, Walsted ES, Nielsen OW, Madsen BL, Tønder N, Benfield TL, Jeschke KN, Ulrik CS, Knop F, Pallisgaard J, Lamberts M, Sivapalan P, Gislason G, Solomon SD, Iversen K, Jensen JUS, Schou M, Biering-Sørensen T (2020) Myocardial impairment and acute respiratory distress syndrome in hospitalized patients with coronavirus disease-2019: The ECHOVID-19 study. JACC Cardiovasc Imaging. https://doi.org/10.1016/j.jcmg.2020.08.005
Pivetta E, Goffi A, Nazerian P, Castagno D, Tozzetti C, Tizzani P, Tizzani M, Porrino G, Ferreri E, Busso V, Morello F, Paglieri C, Masoero M, Cassine E, Bovaro F, Grifoni S, Maule MM, Lupia E (2019) Study group on lung ultrasound from the Molinette and Careggi hospitals, lung ultrasound integrated with clinical assessment for the diagnosis of acute decompensated heart failure in the emergency department: a randomized controlled trial. Eur J Heart Fail 21:754–766. https://doi.org/10.1002/ejhf.1379
Lui KJ, Cumberland WG (1995) A Wilcoxon-type test for trend. Stat Med 14:445–446. https://doi.org/10.1002/sim.4780140409
Trauer MM, Matthies A, Mani N, McDermott C, Jarman R (2020) The utility of lung ultrasound in COVID-19: a systematic sco** review. Ultrasound. https://doi.org/10.1177/1742271X20950779
Favot M, Malik A, Rowland J, Haber B, Ehrman R, Harrison N (2020) Point-of-care lung ultrasound for detecting severe presentations of coronavirus disease 2019 in the emergency department: A retrospective analysis. Crit Care Explor 2:e0176. https://doi.org/10.1097/CCE.0000000000000176
Platz E, Campbell RT, Claggett B, Lewis EF, Groarke JD, Docherty KF, Lee MMY, Merz AA, Silverman M, Swamy V, Lindner M, Rivero J, Solomon SD, McMurray JJV (2019) Lung ultrasound in acute heart failure: prevalence of pulmonary congestion and short- and long-term outcomes. JACC Heart Fail 7:849–858. https://doi.org/10.1016/j.jchf.2019.07.008
Platz E, Lewis EF, Uno H, Peck J, Pivetta E, Merz AA, Hempel D, Wilson C, Frasure SE, Jhund PS, Cheng S, Solomon SD (2016) Detection and prognostic value of pulmonary congestion by lung ultrasound in ambulatory heart failure patients. Eur Heart J 37:1244–1251. https://doi.org/10.1093/eurheartj/ehv745
Espersen C, Campbell RT, Claggett B, Lewis EF, Groarke JD, Docherty KF, Lee MMY, Lindner M, Biering-Sørensen T, Solomon SD, McMurray JJV, Platz E (2021) Sex differences in congestive markers in patients hospitalized for acute heart failure. ESC Heart Fail 8:1784–1795. https://doi.org/10.1002/ehf2.13300
Funding
TBS, together with KGS and MHL, received a research grant from the Novo Nordisk Foundation to conduct the study. Europcar Denmark provided cars for KGS and MHL to transport the equipment from hospital to hospital. TBS received funds from Herlev and Gentofte Hospital and the Lundbeck foundation while conducting this study. The sponsors had no role in the design and interpretation of the data.
Author information
Authors and Affiliations
Contributions
All the authors have contributed to the study in a manner that merits authorship as described in the journals’ “guideline for authors”.
Corresponding author
Ethics declarations
Conflict of interest
TBS reports receiving research grants from Sanofi Pasteur and GE Healthcare, is a Steering Committee member of the Amgen financed GALACTIC-HF trial, on advisory boards for Sanofi Pasteur and Amgen, and speaker honorariums from Novartis and Sanofi Pasteur. EP has received research support from the NIH outside the submitted work, and consulting fees from scPharmaceuticals outside the submitted work. Her employer has received support from Novartis for consulting work outside the submitted work. The remaining authors have nothing to disclose in relation to the present project.
Ethics approval
The study was approved by the regional ethics board and was conducted in accordance with the 2nd Helsinki Declaration. The ECHOVID-19 study is registered at Clinicaltrials.gov (NCT04377035).
Consent to participate
Informed consent was obtained from all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
All the authors take responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation.
Rights and permissions
About this article
Cite this article
Skaarup, K.G., Lassen, M.C.H., Espersen, C. et al. Lung ultrasound findings in hospitalized COVID-19 patients in relation to venous thromboembolic events: the ECHOVID-19 study. J Ultrasound 25, 457–467 (2022). https://doi.org/10.1007/s40477-021-00605-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40477-021-00605-8