Abstract
Purpose of Review
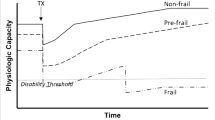
This review presents an overview of the clinical syndrome of frailty and its association with kidney transplantation outcomes, recent developments in refining frailty assessment, and considerations for its implementation into kidney transplant evaluation.
Recent Findings
Recent studies show that frailty is associated with adverse clinical outcomes before and after kidney transplantation, including decreased likelihood of listing and increased risks of mortality. However, frailty assessment has yet to be fully adopted by transplant centers; a study found that 40.9% of centers reported never assessing frailty at evaluation of kidney transplant candidates. Geriatric transplant experts and kidney transplant candidates agree that frailty is a valid consideration for evaluating candidacy.
Summary
While frailty is an important consideration for treatment of patients with end-stage renal disease, its use in kidney transplant evaluation remains under-utilized. Future research is necessary to refine the frailty phenotype for effective integration into a kidney transplant context.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Recently published papers of particular interest have been denoted as:• Of importance •• Of major importance
Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–56. https://doi.org/10.1093/gerona/56.3.m146.
Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci. 2004;59(3):255–63. https://doi.org/10.1093/gerona/59.3.m255.
Fried LP, Cohen AA, Xue QL, Walston J, Bandeen-Roche K, Varadhan R. The physical frailty syndrome as a transition from homeostatic symphony to cacophony. Nat Aging. 2021;1(1):36–46. https://doi.org/10.1038/s43587-020-00017-z.
Perez Fernandez M, Martinez Miguel P, Ying H, Haugen CE, Chu NM, Rodriguez Puyol DM, et al. Comorbidity, frailty, and waitlist mortality among kidney transplant candidates of all ages. Am J Nephrol. 2019;49(2):103–10. https://doi.org/10.1159/000496061.
Harhay MN, Rao MK, Woodside KJ, Johansen KL, Lentine KL, Tullius SG, et al. An overview of frailty in kidney transplantation: measurement, management and future considerations. Nephrol Dial Transplant. 2020;35(7):1099–112. https://doi.org/10.1093/ndt/gfaa016.
Thurlow JS, Joshi M, Yan G, Norris KC, Agodoa LY, Yuan CM, et al. Global epidemiology of end-stage kidney disease and disparities in kidney replacement therapy. Am J Nephrol. 2021;52(2):98–107. https://doi.org/10.1159/000514550.
Quint EE, Zogaj D, Banning LBD, Benjamens S, Annema C, Bakker SJL, et al. Frailty and kidney transplantation: a systematic review and meta-analysis. Transplant Direct. 2021;7(6):e701. https://doi.org/10.1097/TXD.0000000000001156. This review highlights studies on the prevalence of frailty among kidney transplant candidates, and the association between frailty, patient characteristics, and postoperative outcomes for recipients.
Bandeen-Roche K, Seplaki CL, Huang J, Buta B, Kalyani RR, Varadhan R, et al. Frailty in older adults: a nationally representative profile in the United States. J Gerontol A Biol Sci Med Sci. 2015;70(11):1427–34. https://doi.org/10.1093/gerona/glv133.
Alsaad R, Chen X, McAdams-DeMarco M. The clinical application of frailty in nephrology and transplantation. Curr Opin Nephrol Hypertens. 2021;30(6):593–9. https://doi.org/10.1097/MNH.0000000000000743.
Buta BJ, Walston JD, Godino JG, Park M, Kalyani RR, Xue QL, et al. Frailty assessment instruments: systematic characterization of the uses and contexts of highly-cited instruments. Ageing Res Rev. 2016;26:53–61. https://doi.org/10.1016/j.arr.2015.12.003.
Mitnitski AB, Mogilner AJ, Rockwood K. Accumulation of deficits as a proxy measure of aging. Sci World J. 2001;1:323–36. https://doi.org/10.1100/tsw.2001.58.
Rockwood K, Mitnitski A. Frailty in relation to the accumulation of deficits. J Gerontol A Biol Sci Med Sci. 2007;62(7):722–7. https://doi.org/10.1093/gerona/62.7.722.
Xue QL, Tian J, Walston JD, Chaves PHM, Newman AB, Bandeen-Roche K. Discrepancy in frailty identification: move beyond predictive validity. J Gerontol A Biol Sci Med Sci. 2020;75(2):387–93. https://doi.org/10.1093/gerona/glz052.
Cesari M, Gambassi G, van Kan GA, Vellas B. The frailty phenotype and the frailty index: different instruments for different purposes. Age Ageing. 2014;43(1):10–2. https://doi.org/10.1093/ageing/aft160.
Ritt M, Schwarz C, Kronawitter V, Delinic A, Bollheimer LC, Gassmann KG, et al. Analysis of Rockwood et al's Clinical Frailty Scale and Fried et al's Frailty Phenotype as predictors of mortality and other clinical outcomes in older patients who were admitted to a geriatric ward. J Nutr Health Aging. 2015;19(10):1043–8. https://doi.org/10.1007/s12603-015-0667-9.
Perracini MR, Mello M, de Oliveira MR, Bilton TL, Ferriolli E, Lustosa LP, et al. Diagnostic accuracy of the short physical performance battery for detecting frailty in older people. Phys Ther. 2020;100(1):90–8. https://doi.org/10.1093/ptj/pzz154.
Nastasi AJ, McAdams-DeMarco MA, Schrack J, Ying H, Olorundare I, Warsame F, et al. Pre-kidney transplant lower extremity impairment and post-kidney transplant mortality. Am J Transplant. 2018;18(1):189–96. https://doi.org/10.1111/ajt.14430.
Pritchard JM, Kennedy CC, Karampatos S, Ioannidis G, Misiaszek B, Marr S, et al. Measuring frailty in clinical practice: a comparison of physical frailty assessment methods in a geriatric out-patient clinic. BMC Geriatr. 2017;17(1):264. https://doi.org/10.1186/s12877-017-0623-0.
Painter P, Kuskowski M. A closer look at frailty in ESRD: getting the measure right. Hemodial Int. 2013;17(1):41–9. https://doi.org/10.1111/j.1542-4758.2012.00719.x.
Bao Y, Dalrymple L, Chertow GM, Kaysen GA, Johansen KL. Frailty, dialysis initiation, and mortality in end-stage renal disease. Arch Intern Med. 2012;172(14):1071–7. https://doi.org/10.1001/archinternmed.2012.3020.
Rodriguez Villarreal I, Ortega O, Hinostroza J, Cobo G, Gallar P, Mon C, et al. Geriatric assessment for therapeutic decision-making regarding renal replacement in elderly patients with advanced chronic kidney disease. Nephron Clin Pract. 2014;128(1-2):73–8. https://doi.org/10.1159/000363624.
Kallenberg MH, Kleinveld HA, Dekker FW, van Munster BC, Rabelink TJ, van Buren M, et al. Functional and cognitive impairment, frailty, and adverse health outcomes in older patients reaching ESRD-a systematic review. Clin J Am Soc Nephrol. 2016;11(9):1624–39. https://doi.org/10.2215/CJN.13611215.
Kutner NG, Zhang R, Huang Y, McClellan WM, Soltow QA, Lea J. Risk factors for frailty in a large prevalent cohort of hemodialysis patients. Am J Med Sci. 2014;348(4):277–82. https://doi.org/10.1097/MAJ.0000000000000250.
Johansen KL, Dalrymple LS, Delgado C, Kaysen GA, Kornak J, Grimes B, et al. Association between body composition and frailty among prevalent hemodialysis patients: a US Renal Data System special study. J Am Soc Nephrol. 2014;25(2):381–9. https://doi.org/10.1681/ASN.2013040431.
Kojima G. Prevalence of frailty in end-stage renal disease: a systematic review and meta-analysis. Int Urol Nephrol. 2017;49(11):1989–97. https://doi.org/10.1007/s11255-017-1547-5.
Roshanravan B, Khatri M, Robinson-Cohen C, Levin G, Patel KV, de Boer IH, et al. A prospective study of frailty in nephrology-referred patients with CKD. Am J Kidney Dis. 2012;60(6):912–21. https://doi.org/10.1053/j.ajkd.2012.05.017.
Wilhelm-Leen ER, Hall YN, M KT, Chertow GM. Frailty and chronic kidney disease: the Third National Health and Nutrition Evaluation Survey. Am J Med. 2009;122(7):664–71 e2. https://doi.org/10.1016/j.amjmed.2009.01.026.
Reese PP, Cappola AR, Shults J, Townsend RR, Gadegbeku CA, Anderson C, et al. Physical performance and frailty in chronic kidney disease. American Journal of Nephrology. 2013;38(4):307–15. https://doi.org/10.1159/000355568.
Johansen KL, Chertow GM, ** C, Kutner NG. Significance of frailty among dialysis patients. J Am Soc Nephrol. 2007;18(11):2960–7. https://doi.org/10.1681/ASN.2007020221.
Lee SY, Yang DH, Hwang E, Kang SH, Park SH, Kim TW, et al. The prevalence, association, and clinical outcomes of frailty in maintenance dialysis patients. J Ren Nutr. 2017;27(2):106–12. https://doi.org/10.1053/j.jrn.2016.11.003.
McAdams-DeMarco MA, Law A, Salter ML, Boyarsky B, Gimenez L, Jaar BG, et al. Frailty as a novel predictor of mortality and hospitalization in individuals of all ages undergoing hemodialysis. J Am Geriatr Soc. 2013;61(6):896–901. https://doi.org/10.1111/jgs.12266.
McAdams-DeMarco MA, Suresh S, Law A, Salter ML, Gimenez LF, Jaar BG, et al. Frailty and falls among adult patients undergoing chronic hemodialysis: a prospective cohort study. BMC Nephrol. 2013;14:224. https://doi.org/10.1186/1471-2369-14-224.
Fitzpatrick J, Sozio SM, Jaar BG, Estrella MM, Segev DL, Shafi T, et al. Frailty, age, and postdialysis recovery time in a population new to hemodialysis. Kidney360. 2021;2(9):1455–62. https://doi.org/10.34067/KID.0001052021.
Ofori-Asenso R, Chin KL, Mazidi M, Zomer E, Ilomaki J, Zullo AR, et al. Global incidence of frailty and prefrailty among community-dwelling older adults: a systematic review and meta-analysis. JAMA Netw Open. 2019;2(8):e198398. https://doi.org/10.1001/jamanetworkopen.2019.8398.
Haugen CE, Thomas AG, Chu NM, Shaffer AA, Norman SP, Bingaman AW, et al. Prevalence of frailty among kidney transplant candidates and recipients in the United States: estimates from a National Registry and Multicenter Cohort Study. Am J Transplant. 2020;20(4):1170–80. https://doi.org/10.1111/ajt.15709. This recent study presents an estimated national prevalence of frailty in the U.S. kidney transplant candidate and recipient populations from 2008 to 2018.
Chu NM, Chen X, Norman SP, Fitzpatrick J, Sozio SM, Jaar BG, et al. Frailty prevalence in younger end-stage kidney disease patients undergoing dialysis and transplantation. Am J Nephrol. 2020;51(7):501–10. https://doi.org/10.1159/000508576.
McAdams-DeMarco MA, Ying H, Thomas AG, Warsame F, Shaffer AA, Haugen CE, et al. Frailty, inflammatory markers, and waitlist mortality among patients with end-stage renal disease in a prospective cohort study. Transplant. 2018;102(10):1740–6. https://doi.org/10.1097/TP.0000000000002213.
Haugen CE, Chu NM, Ying H, Warsame F, Holscher CM, Desai NM, et al. Frailty and access to kidney transplantation. Clin J Am Soc Nephrol. 2019;14(4):576–82. https://doi.org/10.2215/CJN.12921118. This study found frailty to be associated with decreased odds of listing for kidney transplantation; frail patients were also found to undergo transplantation less frequently.
Perez-Saez MJ, Redondo-Pachon D, Arias-Cabrales CE, Faura A, Bach A, Buxeda A, et al. Outcomes of frail patients while waiting for kidney transplantation: differences between physical frailty phenotype and FRAIL scale. J Clin Med. 2022;11(3). https://doi.org/10.3390/jcm11030672.
Lorenz EC, Cosio FG, Bernard SL, Bogard SD, Bjerke BR, Geissler EN, et al. The relationship between frailty and decreased physical performance with death on the kidney transplant waiting list. Prog Transplant. 2019;29(2):108–14. https://doi.org/10.1177/1526924819835803.
McAdams-DeMarco MA, Ying H, Olorundare I, King EA, Haugen C, Buta B, et al. Individual frailty components and mortality in kidney transplant recipients. Transplant. 2017;101(9):2126–32. https://doi.org/10.1097/TP.0000000000001546.
Garonzik-Wang JM, Govindan P, Grinnan JW, Liu M, Ali HM, Chakraborty A, et al. Frailty and delayed graft function in kidney transplant recipients. Arch Surg. 2012;147(2):190–3. https://doi.org/10.1001/archsurg.2011.1229.
McAdams-DeMarco MA, Law A, Salter ML, Chow E, Grams M, Walston J, et al. Frailty and early hospital readmission after kidney transplantation. Am J Transplant. 2013;13(8):2091–5. https://doi.org/10.1111/ajt.12300.
Schopmeyer L, El Moumni M, Nieuwenhuijs-Moeke GJ, Berger SP, Bakker SJL, Pol RA. Frailty has a significant influence on postoperative complications after kidney transplantation-a prospective study on short-term outcomes. Transpl Int. 2019;32(1):66–74. https://doi.org/10.1111/tri.13330.
Dos Santos MM, Coelho de Carvalho N, Archangelo TE, Modelli de Andrade LG, Pires Ferreira Filho S, de Souza CR, et al. Frailty predicts surgical complications after kidney transplantation. A propensity score matched study. PLoS One. 2020;15(2):e0229531. https://doi.org/10.1371/journal.pone.0229531.
Davies EA, O'Mahony MS. Adverse drug reactions in special populations - the elderly. Br J Clin Pharmacol. 2015;80(4):796–807. https://doi.org/10.1111/bcp.12596.
Fozouni L, Mohamad Y, Lebsack A, Freise C, Stock P, Lai JC. Frailty is associated with increased rates of acute cellular rejection within 3 months after liver transplantation. Liver Transpl. 2020;26(3):390–6. https://doi.org/10.1002/lt.25669.
McAdams-DeMarco MA, Law A, Tan J, Delp C, King EA, Orandi B, et al. Frailty, mycophenolate reduction, and graft loss in kidney transplant recipients. Transplant. 2015;99(4):805–10. https://doi.org/10.1097/TP.0000000000000444.
Gonzalez-Molina M, Burgos D, Cabello M, Ruiz-Esteban P, Rodriguez MA, Gutierrez C, et al. Impact of immunosuppression treatment on the improvement in graft survival after deceased donor renal transplantation: a long-term cohort study. Nefrologia. 2014;34(5):570–8. https://doi.org/10.3265/Nefrologia.pre2014.Jun.12327.
Opelz G, Dohler B. Effect on kidney graft survival of reducing or discontinuing maintenance immunosuppression after the first year posttransplant. Transplant. 2008;86(3):371–6. https://doi.org/10.1097/TP.0b013e31817fdddb.
McAdams-DeMarco MA, King EA, Luo X, Haugen C, DiBrito S, Shaffer A, et al. Frailty, length of stay, and mortality in kidney transplant recipients: a National Registry and Prospective Cohort Study. Ann Surg. 2017;266(6):1084–90. https://doi.org/10.1097/SLA.0000000000002025.
McAdams-DeMarco MA, Law A, King E, Orandi B, Salter M, Gupta N, et al. Frailty and mortality in kidney transplant recipients. Am J Transplant. 2015;15(1):149–54. https://doi.org/10.1111/ajt.12992.
Chu NM, Deng A, Ying H, Haugen CE, Garonzik Wang JM, Segev DL, et al. Dynamic frailty before kidney transplantation: time of measurement matters. Transplant. 2019;103(8):1700–4. https://doi.org/10.1097/TP.0000000000002563.
McAdams-DeMarco MA, Isaacs K, Darko L, Salter ML, Gupta N, King EA, et al. Changes in frailty after kidney transplantation. J Am Geriatr Soc. 2015;63(10):2152–7. https://doi.org/10.1111/jgs.13657.
Chu NM, Ruck J, Chen X, Xue QL, Norman SP, Segev DL, et al. Long-term trajectories of frailty and its components after kidney transplantation. J Gerontol A Biol Sci Med Sci. 2022;77(12). https://doi.org/10.1093/gerona/glac051.
McAdams-DeMarco MA, Olorundare IO, Ying H, Warsame F, Haugen CE, Hall R, et al. Frailty and postkidney transplant health-related quality of life. Transplant. 2018;102(2):291–9. https://doi.org/10.1097/TP.0000000000001943.
McAdams-DeMarco MA, Ying H, Olorundare I, King EA, Desai N, Dagher N, et al. Frailty and health-related quality of life in end stage renal disease patients of all ages. J Frailty Aging. 2016;5(3):174–9.
McAdams-DeMarco MA, Tan J, Salter ML, Gross A, Meoni LA, Jaar BG, et al. Frailty and cognitive function in incident hemodialysis patients. Clin J Am Soc Nephrol. 2015;10(12):2181–9. https://doi.org/10.2215/CJN.01960215.
Chu NM, Xue QL, McAdams-DeMarco MA, Carlson MC, Bandeen-Roche K, Gross AL. Frailty-a risk factor of global and domain-specific cognitive decline among a nationally representative sample of community-dwelling older adult U.S. Medicare beneficiaries. Age Ageing. 2021;50(5):1569–77. https://doi.org/10.1093/ageing/afab102.
Haugen CE, Mountford A, Warsame F, Berkowitz R, Bae S, Thomas AG, et al. Incidence, risk factors, and sequelae of post-kidney transplant delirium. J Am Soc Nephrol. 2018;29(6):1752–9. https://doi.org/10.1681/ASN.2018010064.
Chu NM, Gross AL, Shaffer AA, Haugen CE, Norman SP, Xue QL, et al. Frailty and changes in cognitive function after kidney transplantation. J Am Soc Nephrol. 2019;30(2):336–45. https://doi.org/10.1681/ASN.2018070726.
Warsame F, Haugen CE, Ying H, Garonzik-Wang JM, Desai NM, Hall RK, et al. Limited health literacy and adverse outcomes among kidney transplant candidates. Am J Transplant. 2019;19(2):457–65. https://doi.org/10.1111/ajt.14994.
Konel JM, Warsame F, Ying H, Haugen CE, Mountford A, Chu NM, et al. Depressive symptoms, frailty, and adverse outcomes among kidney transplant recipients. Clin Transplant. 2018;32(10):e13391. https://doi.org/10.1111/ctr.13391.
Van Pilsum RS, Konel J, Warsame F, Ying H, Buta B, Haugen C, et al. Engaging clinicians and patients to assess and improve frailty measurement in adults with end stage renal disease. BMC Nephrol. 2018;19(1):8. https://doi.org/10.1186/s12882-017-0806-0.
Salter ML, Gupta N, Massie AB, McAdams-DeMarco MA, Law AH, Jacob RL, et al. Perceived frailty and measured frailty among adults undergoing hemodialysis: a cross-sectional analysis. BMC Geriatr. 2015;15:52. https://doi.org/10.1186/s12877-015-0051-y.
McAdams-DeMarco MA, Van Pilsum Rasmussen SE, Chu NM, Agoons D, Parsons RF, Alhamad T, et al. Perceptions and practices regarding frailty in kidney transplantation: results of a national survey. Transplant. 2020;104(2):349–56. https://doi.org/10.1097/TP.0000000000002779.
Chen X, Liu Y, Thompson V, Chu NM, King EA, Walston JD, et al. Transplant centers that assess frailty as part of clinical practice have better outcomes. BMC Geriatrics. 2022;22(1):1–12. This study revealed an association between frailty assessment at evaluation and decreased transplant rate for kidney transplant candidates. Their findings also suggest that the use of a validated frailty screening instrument is associated with better survival for candidates, particulary over the age of 65.
Bandeen-Roche K, Gross AL, Varadhan R, Buta B, Carlson MC, Huisingh-Scheetz M, et al. Principles and issues for physical frailty measurement and its clinical application. J Gerontol A Biol Sci Med Sci. 2020;75(6):1107–12. https://doi.org/10.1093/gerona/glz158.
Haugen CE, Gross A, Chu NM, Norman SP, Brennan DC, Xue QL, et al. Development and validation of an inflammatory-frailty index for kidney transplantation. J Gerontol A Biol Sci Med Sci. 2021;76(3):470–7. https://doi.org/10.1093/gerona/glaa167.
Kobashigawa J, Dadhania D, Bhorade S, Adey D, Berger J, Bhat G, et al. Report from the American Society of Transplantation on frailty in solid organ transplantation. Am J Transplant. 2019;19(4):984–94. https://doi.org/10.1111/ajt.15198.
Morley JE, Vellas B, van Kan GA, Anker SD, Bauer JM, Bernabei R, et al. Frailty consensus: a call to action. J Am Med Dir Assoc. 2013;14(6):392–7. https://doi.org/10.1016/j.jamda.2013.03.022.
Walston J, Bandeen-Roche K, Buta B, Bergman H, Gill TM, Morley JE, et al. Moving frailty toward clinical practice: NIA Intramural Frailty Science Symposium Summary. J Am Geriatr Soc. 2019;67(8):1559–64. https://doi.org/10.1111/jgs.15928This report summarizes recommendations for implementation of frailty into clinical practice.
Chen X, Shafaat O, Liu Y, King EA, Weiss CR, Xue QL, et al. Revision of frailty assessment in kidney transplant recipients: replacing unintentional weight loss with CT-assessed sarcopenia in the physical frailty phenotype. Am J Transplant. 2022;22(4):1145–57. https://doi.org/10.1111/ajt.16934.
Druckmann I, Yashar H, Schwartz D, Schwartz IF, Goykhman Y, Kliuk Ben-Bassat O, et al. Presence of sarcopenia before kidney transplantation is associated with poor outcomes. Am J Nephrol. 2022;53(6):1–8. https://doi.org/10.1159/000524774.
Bohm CJ, Storsley LJ, Hiebert BM, Nelko S, Tangri N, Cheskin LJ, et al. Impact of exercise counseling on physical function in chronic kidney disease: an observational study. Can J Kidney Health Dis. 2018;5:2054358117753615. https://doi.org/10.1177/2054358117753615.
Fazal MS, Gordon EJ, Humbyrd CJ. Current bioethical issues in geriatric organ transplantation. Curr Transplant Rep. 2022;9(2):55–62. https://doi.org/10.1007/s40472-022-00364-3. This review presents recent developments in geriatric transplantation and corresponding ethical considerations related to organ donation and allocation.
Haugen CE, Agoons D, Chu NM, Liyanage L, Long J, Desai NM, et al. Physical impairment and access to kidney transplantation. Transplant. 2020;104(2):367–73. https://doi.org/10.1097/TP.0000000000002778.
Wu C, Geldhof GJ, Xue QL, Kim DH, Newman AB, Odden MC. Development, construct validity, and predictive validity of a continuous Frailty Scale: results from 2 large US cohorts. Am J Epidemiol. 2018;187(8):1752–62. https://doi.org/10.1093/aje/kwy041.
Shrestha P, Van Pilsum Rasmussen SE, King EA, Gordon EJ, Faden RR, Segev DL, et al. Defining the ethical considerations surrounding kidney transplantation for frail and cognitively impaired patients: a Delphi study of geriatric transplant experts. BMC Geriatr. 2022;22(1):566. https://doi.org/10.1186/s12877-022-03209-x. This paper highlights clinical expert opinions on key ethical issues surrounding frailty, cognitive impairment, and geriatric transplantation.
Shrestha P, Van Pilsum Rasmussen SE, Fazal M, Chu NM, Garonzik-Wang JM, Gordon EJ, et al. Patient perspectives on the use of frailty, cognitive function, and age in kidney transplant evaluation. AJOB Empir Bioeth. 2022;13(4):1–12. https://doi.org/10.1080/23294515.2022.2090460.
Fernandez-Costa D, Gomez-Salgado J, Castillejo Del Rio A, Borrallo-Riego A, Guerra-Martin MD. Effects of prehabilitation on functional capacity in aged patients undergoing cardiothoracic surgeries: a systematic review. Healthcare (Basel). 2021;9(11). https://doi.org/10.3390/healthcare9111602.
Ismail H, Cormie P, Burbury K, Waterland J, Denehy L, Riedel B. Prehabilitation prior to major cancer surgery: training forsurgery to optimize physiologic reserve to reduce postoperative complications. Curr Anesthesiol Rep. 2018;8(4):375–85. https://doi.org/10.1007/s40140-018-0300-7.
Koh FH, Loh CH, Tan WJ, Ho LML, Yen D, Chua JMW, et al. Structured presurgery prehabilitation for aged patients undergoing elective surgery significantly improves surgical outcomes and reduces cost: a nonrandomized sequential comparative prospective cohort study. Nutr in Clin Pract. 2022;37(3):645–53. https://doi.org/10.1002/ncp.10787.
Milder DA, Pillinger NL, Kam PCA. The role of prehabilitation in frail surgical patients: a systematic review. Acta Anaesthesiol Scand. 2018;62(10):1356–66. https://doi.org/10.1111/aas.13239.
Hanna K, Ditillo M, Joseph B. The role of frailty and prehabilitation in surgery. Curr Opin in Crit Care. 2019;25(6):717–22. https://doi.org/10.1097/mcc.0000000000000669.
McAdams-DeMarco MA, Ying H, Van Pilsum RS, Schrack J, Haugen CE, Chu NM, et al. Prehabilitation prior to kidney transplantation: Results from a pilot study. Clin Transplant. 2019;33(1):e13450. https://doi.org/10.1111/ctr.13450.
Lorenz EC, Hickson LJ, Weatherly RM, Thompson KL, Walker HA, Rasmussen JM, et al. Protocolized exercise improves frailty parameters and lower extremity impairment: a promising prehabilitation strategy for kidney transplant candidates. Clin Transplant. 2020;34(9):e14017. https://doi.org/10.1111/ctr.14017.
Cheng XS, Myers JN, Chertow GM, Rabkin R, Chan KN, Chen Y, et al. Prehabilitation for kidney transplant candidates: Is it time? Clin Transplant. 2017;31(8). https://doi.org/10.1111/ctr.13020.
Cheng XS, Lentine KL, Koraishy FM, Myers J, Tan JC. Implications of frailty for peritransplant outcomes in kidney transplant recipients. Curr Transplant Rep. 2019;6(1):16–25. https://doi.org/10.1007/s40472-019-0227-z.
Funding
This work was supported by grant number R01AG055781 (McAdams-DeMarco) and R01AG077888 (McAdams-DeMarco) from the National Institute of Aging (NIA). Dr. Segev was supported by K24AI144954 from the National Institute of Allergy and Infectious Diseases.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Frailty and Gerontology
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Thompson, V.L., Segev, D.L. & McAdams-DeMarco, M. Integrating Frailty into the Kidney Transplant Evaluation. Curr Transpl Rep 10, 12–20 (2023). https://doi.org/10.1007/s40472-023-00389-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40472-023-00389-2