Abstract
The incidence of osteoporosis and cardiovascular disease increases with age, and there are potentially shared mechanistic associations between the two conditions. It is therefore highly relevant to understand the cardiovascular implications of osteoporosis medications. These are presented in this narrative review. Calcium supplementation could theoretically cause atheroma formation via calcium deposition, and in one study was found to be associated with myocardial infarction, but this has not been replicated. Vitamin D supplementation has been extensively investigated for cardiac benefit, but no consistent effect has been found. Despite findings in the early 21st century that menopausal hormone therapy was associated with coronary artery disease and venous thromboembolism (VTE), this therapy is now thought to be potentially safe (from a cardiac perspective) if started within the first 10 years of the menopause. Selective estrogen receptor modulators (SERMs) are associated with increased risk of VTE and may be related to fatal strokes (a subset of total strokes). Bisphosphonates could theoretically provide protection against atheroma. However, data from randomised trials and observational studies have neither robustly supported this nor consistently demonstrated the potential association with atrial fibrillation. Denosumab does not appear to be associated with cardiovascular disease and, although parathyroid hormone analogues are associated with palpitations and dizziness, no association with a defined cardiovascular pathology has been demonstrated. Finally, romosozumab has been shown to have a possible cardiovascular signal, and therefore post-market surveillance of this therapy will be vital.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Osteoporosis and cardiovascular disease are the potential consequences of shared mechanisms. |
Anti-osteoporosis medications are associated with potential increases in cardiac risk (romosozumab, calcium supplementation, menopausal hormonal therapy), no effect on cardiac risk (vitamin D) or reduced cardiac risk (bisphosphonates). |
Selective estrogen receptor modulators, such as raloxifene, and menopausal hormonal therapy are associated with increased risk of venous thromboembolic disease. |
Romosozumab therapy is contra-indicated in those with a history of myocardial infarction or ischaemic stroke. |
1 Introduction
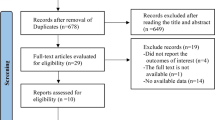
Osteoporosis is characterised by a reduction in bone mineral density and an increased risk of fractures. As with cardiovascular disease, the prevalence increases in older age so that osteoporosis and cardiovascular disease (and cardiovascular risk factors) often coexist in the same patient. Given the age group of patients with osteoporosis [5], made it difficult to interpret the cardiovascular effect of calcium supplementation, and warranted further examination through data assimilation.
Fifteen calcium trials were meta-analysed, and a significantly increased risk of MI was observed (HR 1.27, 95% CI 1.01–1.59), although there was no excess risk of stroke, death or the composite endpoint in the trial-level data [6]. However, in individual patient-level analyses, there was an interaction between treatment and dietary calcium intake when the outcome of interest was MI. This interaction was observed in the patients with a spontaneous calcium intake above, but not below, the median. Thus, clarity was sought through further interrogation of the WHI calcium trial dataset in a meta-analysis together with seven other studies [7] to distil out the effect of personal supplementation alongside calcium supplementation. In those patients who were not taking over-the-counter calcium or vitamin D supplements, there was a 13% increase in the risk of cardiovascular events in those in the calcium arm (HRs from 1.13 to 1.22, p values ranging from 0.04 to 0.05) [7]. However, those who were taking over-the-counter supplements at the time of the study were at no increased risk of cardiovascular events. Calcium or calcium and vitamin D increased the risk of MI (HR 1.24, 95% CI 1.07–1.45) and the composite of MI or stroke (HR 1.15, 95% CI 1.03–1.27). The authors concluded that there was an increased risk of MI and stroke due to calcium supplementation and that this had been “obscured” in the previous WHI study by the use of personal calcium and vitamin D supplements. There are a few caveats to this assertion [8]. Firstly, if Bonferroni correction had been performed, the association with MI and stroke would be non-significant. Secondly, there was no evidence of a dose effect if supplementation was assessed in fifths of supplement intake. Thirdly, this was not a true time-to-event analysis, with more than one event allowed to count in one patient. Fourthly, the safety data were recorded in a heterogeneous fashion depending on the study and, as has been said previously, were not primary endpoints of the trials. These caveats are significant and numerous enough to call into question the findings of the above analysis, and these findings are contradicted by re-analyses and further follow-up of the WHI dataset, the results of more recent meta-analyses and by large observational studies.
Indeed a study by Prentice et al. re-examined the effect of calcium and vitamin D supplementation in the WHI clinical trial and observational study, with a specific focus on fractures, cardiovascular disease, cancer and all-cause mortality [9] and the duration of therapy. They found no associations with risks of cardiovascular disease, including MI, coronary heart disease, total heart disease or stroke. In support of this finding, at 5 years of follow-up, no significant associations were observed with any cardiovascular disease outcomes (Fig. 1 ) [10].
Results taken from the Women’s Health Initiative (WHI) trial of calcium and vitamin D (CaD) showing the cumulative hazard of coronary heart disease (CHD) against time. Intervention (left) and post-intervention (right) follow-up are depicted. There was no significant difference in the rates of CHD between the CaD and placebo arms [10]
Due to the emergence of new data since the meta-analysis by Bolland et al. [6], an updated meta-analysis was performed in 2015 by Lewis et al. [11] particularly examining randomised controlled trial data comparing calcium (and vitamin D) supplements to non-treatment or placebo controls and limiting their analyses to females alone. They included 18 studies, with a total of 63,563 participants with 3390 coronary heart disease events and 4157 deaths, and found no associations between primary outcomes (coronary heart disease and mortality) or secondary outcomes (acute MI, angina and chronic coronary heart disease).
Further observational studies have found no increased cardiovascular risk with calcium supplementation. A study using the UK Biobank (a cohort of 500,000 men and women in the UK, aged 40–69 years at baseline) showed incident cardiovascular disease in the 10.6% of women and 2.6% of men who took calcium supplements [12]. Subsets of patients on calcium supplements alone were compared to those on calcium and vitamin D, and no effect was observed in the incidence of MI, IHD or any cardiovascular outcomes over the 5–10 years of follow-up. Within such observational studies, there are potential epidemiological issues, including confounding by indication, time-varying confounding, depletion of susceptible subjects and over-the-counter use of calcium and vitamin D, which is common in the UK. One explanation for the apparent confusion in this area may be in the definition of cardiovascular events. However, even a large study including coronary artery computed tomography (CT) scans and a mean of 7 years of supplements in ~ 750 women (aged 50–59 at baseline) demonstrated no association [13].
The most recent meta-analysis at the time of writing was performed in 2019 by Yang et al. Their meta-analysis of 42 studies (26 prospective cohort studies and 16 randomised controlled trials) of calcium intake, in which cardiovascular disease outcomes were recorded, showed that dietary calcium intake of up to 1500 mg/day had no significant effect on the risk of cardiovascular disease as a whole or on stroke in isolation [86]. Interestingly, in this study, the patients who underwent coronary angiography were investigated as a high-risk subgroup and, again, no benefit of bisphosphonate therapy was observed [86].
The possible cardioprotective effects of bisphosphonates remain under scrutiny, and there is certainly not sufficiently robust, cohesive data to support a recommendation for this class of medications to be used to treat cardiovascular disease, or even to recommend using them to treat osteoporosis in those at high risk of MI or stroke. A recent meta-analysis reported that mortality was not altered by bisphosphonate treatment [87].
The connection between bisphosphonates and arrhythmia has an equally mixed picture. Early analysis of the safety data from the HORIZON trial demonstrated a significantly higher incidence of arrhythmia in the zoledronate arm (6.9% vs 5.3% in the placebo arm, p = 0.003) and that within this group ‘serious atrial fibrillation’ (atrial fibrillation that resulted in a serious adverse event) was significantly more common (1.3% vs 0.5% in the placebo arm, p < 0.001) [82]. A similar trend had been previously observed in the Fracture Intervention Trial (of alendronate) [88], but although the cumulative incidence of serious atrial fibrillation had numerically increased with alendronate, the rise had not been statistically significant.
Further studies sought to investigate this association, with conflicting findings. A case–controlled study from a healthcare database in the USA found that a greater number of atrial fibrillation case patients than controls had ever used alendronate (6.5% vs 4.1%, p = 0.03) and that when comparing ever-users (of bisphosphonates) to never-users, the ever-users had a higher risk of incident atrial fibrillation (OR 1.86, 95% CI 1.09–3.15) [89]. However, a European population-based, case–control study (comparing ~ 13,500 patients with atrial fibrillation or flutter to ~ 68,000 controls) found no evidence of increased risk of arrhythmia with bisphosphonates [90]. This finding was supported by another European case–control, register-based cohort study, which found that the highest risk of atrial fibrillation was in the subgroup of patients who only received the bisphosphonates once and the longer the patient was adherent to bisphosphonates, the lower the risk of atrial fibrillation [91].
An interesting hypothesis from the latter study was that fracture patients were inherently more likely to experience atrial fibrillation (compared to non-fracture controls) and more likely to receive bisphosphonates, thus confounding the association [91]. This theory was supported in the aforementioned study of two large prospective databases, which found that patients on bisphosphonates were inherently older with a greater cardiovascular disease burden, thus increasing their risk of atrial fibrillation.
Considering that the majority of the signal is for an increased risk of atrial fibrillation with bisphosphonate therapy came from the HORIZON trial and zoledronic acid, it should be acknowledged that in the Recurrent HORIZON trial (consisting of a more elderly, infirm, post-hip fracture population), there was no significant increase in serious atrial fibrillation [83]. Neither was atrial fibrillation increased in those on zoledronate in the PREVENTION study (a 6-year randomised, placebo-controlled trial of 2000 women) [84].
Therefore, in conclusion, there is no substantial signal for the development of atrial fibrillation with bisphosphonates at present, though further studies examining and powered to answer this exact question are warranted.
8 Denosumab
Denosumab (60 mg, every 6 months) is a fully human monoclonal antibody and inhibitor of receptor activator of nuclear factor-κB (RANK) ligand, which prevents the maturation and activity of osteoclasts and therefore acts to reduce bone resorption. There is a potential, though tenuous, link with cardiovascular health via RANK-ligand, RANK and osteoprotegerin (OPG). OPG is found in calcifications in the aorta and renal arteries, and transgenic overexpression of OPG leads to inhibition of these calcified vascular lesions. Indeed, when an atherogenic mouse model was treated with OPG, there was a significant reduction in calcified lesions. RANK-ligand itself is known to induce calcification of vascular smooth muscle, and the development of vascular calcifications depends on RANK-ligand–mediated expression of bone morphogenetic protein-2 (BMP-2) and matrix Gla protein. Thus OPG could potentially inhibit the formation of vascular calcifications by blocking RANK-ligand and there is thus a plausible biological mechanism for some prevention of cardiovascular pathology when treated with denosumab. This is, however, not borne out by the evidence from randomised controlled trials.
The Fracture Reduction Evaluation of Denosumab in Osteoporosis Every 6 Months (FREEDOM) study was a phase 3, multicentre, double-blind, placebo-controlled trial of denosumab over 3 years [92]. It included a total of 7868 women (with 31.7% of these ≥ 75 years), and throughout this initial trial period, there was no significant difference in cardiovascular events, stroke, coronary heart disease, peripheral vascular disease or atrial fibrillation [92]. Despite the fact that FREEDOM was not powered to investigate mortality, there was a non-significant trend towards reduced mortality in the denosumab group (1.8% participants in denosumab group vs 2.3% participants in the control group, p = 0.08) [92].
In 2014, there was a further analysis of a subset of 2363 women (1142 placebo, 1221 denosumab) from the FREEDOM trial who were at high risk of cardiovascular disease (as defined by the RUTH criteria) [93]. In this study, aortic calcification and progression was assessed using a semi-quantitative method from lateral spine radiographs. There was no significant difference in aortic calcification progression over the 3 years of the trial between the placebo (22%) and denosumab (22%) groups and no difference in cardiovascular risk across the two groups (in the high cardiovascular risk population) [93].
In conclusion, although a plausible biological connection exists between denosumab and cardiovascular disease, there is no evidence from human trials to support a positive or negative effect on cardiovascular risk, at least at the dose used in osteoporosis therapy.
9 Parathyroid Hormone Analogues
It has long been known, initially from animal studies, that PTH has chronotropic effects via receptors in cardiac myocytes and transient dilatory effects on the peripheral vasculature, leading to an increase in heart rate and reduction in blood pressure, respectively [94]. These effects may have manifested as adverse events in the trials for the two PTH analogues that are currently used in osteoporosis clinical practice: teriparatide and abaloparatide.
The Summary of Product Characteristics for teriparatide lists nausea, headache and dizziness as potential adverse effects, which could potentially be related to the cardiovascular mechanisms described above from animal studies. Indeed in the VERtebral Fracture Treatment Comparisons in Osteoporotic Women (VERO) trial comparing teriparatide to risedronate, there was a significantly higher incidence of dizziness (teriparatide 30 [4.4%], risedronate 12 [1.8%], p = 0.007) in those taking teriparatide, but there was no excess incidence of cardiovascular adverse events [95]. Even in post-marketing surveillance, there was no perceptible signal of increased risk of cardiovascular adverse events, as demonstrated by a Japanese, prospective, observational study [96].
A similar story was observed in the Abaloparatide Comparator Trial in Vertebral Endpoints (ACTIVE) [97], which included teriparatide and placebo arms. In the abaloparatide arm, discontinuation of the study drug was most commonly due to nausea (1.6%), dizziness (1.2%), headache (1.0%) and palpitations (0.9%). Dizziness had a higher incidence in the abaloparatide group (10.0%) than in the teriparatide group (7.3%) or placebo group (6.1%). However, ‘dizziness’ is a symptom with both potential cardiovascular and neurological aetiology, and it is therefore interesting that the more cardiovascular endpoint of orthostatic hypotension was defined as an adverse event of special interest and was very similar across all three arms (17.1% in the teriparatide arm, 16.4% in the placebo arm and 15.5% in the teriparatide arm) suggesting a lack of association. Palpitations were most common with abaloparatide (5.1%), with a lower incidence with teriparatide (1.6%), and placebo being the lowest (0.4%). There was no excess risk of MI, falls or syncope.
In conclusion, animal models have demonstrated potential effects of PTH on the cardiovascular system [94], and these may lead to increased rates of dizziness [95] with PTH analogues. However, whether this increased risk is manifested via the cardiovascular system is not clear, and there is certainly no current evidence to suggest an increased risk of atherosclerotic or thromboembolic cardiac disease with this group of interventions.
10 Romosozumab
Romosozumab is a humanised monoclonal antibody, approved by the Food and Drug Administration (FDA) [98] and European Medicines Agency (EMA) [99], which inhibits sclerostin. Sclerostin is an effective antagonist of Wnt signalling, and thus romosozumab acts as an anabolic agent for bone formation and as an inhibitor of bone resorption. Controversy exists regarding the cardiovascular safety of this drug from the point of biological plausibility, the outcomes of randomised controlled trials [100,101,102] and the output of meta-analyses [103]. Current guidance (in some regions) advocates against use in those with a history of MI and ischaemic stroke and recommends a judicious approach in those with a high baseline risk of cardiovascular disease [99, 104].
The arguments for the biological plausibility of adverse cardiovascular effects of romosozumab centre on a potential role in arterial calcification. Sclerostin is the product of the SOST gene and is primarily secreted by osteocytes. It plays an important role in bone turnover by upregulating bone formation and downregulating bone resorption [101, 105]. Beyond the skeleton, increased sclerostin expression has been observed in smooth muscle tissue in areas of vascular calcification [106]. At these sites, sclerostin may act to limit the formation of calcified plaques [107] and confer a degree of cardiovascular benefit.
In a murine model of increased cardiovascular risk, apolipoprotein E (apoE)-null mice (prone to aortic aneurysm and atherosclerosis) were provided with an infusion of angiotensin II [108]. They were then subjected to sclerostin from either transgenic overexpression or exogenous recombinant murine sclerostin. Increased sclerostin, from either source, was found to be protective against aortic aneurysm formation and atherosclerosis. This was further supported by data from experiments in which a murine model of glucocorticoid-induced osteopenia was crossed with a Sost-deficient (and therefore sclerostin-deficient) mouse [109], with resultant sudden death in ~ 10% of mice. On post-mortem, histopathological evidence of peracute haemopericardium and cardiac tamponade was observed. These murine data support the theory of a cardiovascular protective effect of sclerostin.
This has resulted in the hypothesis that romosozumab-induced sclerostin inhibition could modulate Wnt-β-catenin signalling [110] via a compensatory increase in expression of Dickkopf Wnt signalling pathway inhibitor 1 (DKK1) [111] to result in vascular calcification and destabilisation of atherosclerotic plaques [112].
However, this effect of romosozumab has not been clearly demonstrated in animal models. Indeed, the administration of romosozumab did not significantly alter DKK1 levels in a rat model of progressive renal osteodystrophy [113] or ovariectomised cynomolgus monkeys in response to romosozumab [114].
In human conditions associated with reduced activity of sclerostin, neither van Buchem’s disease nor sclerosteosis demonstrate cardiovascular disease manifestations [115, 116], although it should be noted that a substantial proportion of homozygous individuals die in early adulthood (mean age of death 33 years) due to complications of increased intracranial pressure [117], and the effect of sclerostin inhibition in an older age-group may be different.
As described above, although there are potential hypotheses, there is not a robust demonstration of a biological basis for cardiovascular disease related to romosozumab.
The FRActure study in postmenopausal woMEn with osteoporosis (FRAME) was a randomised controlled trial comparing romosozumab to placebo, before transitioning onto denosumab [100, 101]. In this trial, there were no observed associations between romosozumab and cardiovascular adverse events, including major adverse cardiac events (MACE) (a composite of non-fatal MI, non-fatal stroke and cardiovascular death), with an HR of 1.1 (95% CI 0.7–1.7). In the FRAME extension study, the percentage of positively adjudicated adverse cardiac events did not differ significantly, with 3.6% for romosozumab and 3.5% for placebo [118]. However, it should be noted that the participant population included women with a broad range of osteoporosis severity, rather than being focused only on those with severe disease.
The Active-Controlled Fracture Study in Postmenopausal Women with Osteoporosis at High Risk (ARCH) [102] compared romosozumab to alendronate, before transitioning onto long-term alendronate therapy. Unlike FRAME, ARCH did focus on individuals with severe osteoporosis, and therefore the participant group was older and had a higher baseline prevalence of cardiovascular disease and risk.
Although ARCH was designed and powered to assess efficacy in the treatment of osteoporosis, the primary cardiac safety endpoint was serious cardiovascular adverse events (composed of MACE outcomes [non-fatal MI, non-fatal stroke and cardiovascular death] plus heart failure and non-coronary heart disease), and this did not differ significantly between treatment groups (2.5% romosozumab and 1.9% alendronate; HR 1.32, 95% CI 0.87–2.01, p = 0.2) [102]. In post hoc analyses of MACE, the incidence was 2.0% in the romosozumab group and 1.1% in the alendronate group, indicating a significant preponderance for cardiovascular disease with romosozumab (HR 1.7, 95% CI 1.1–2.6) [99].
Examining the constituent parts of MACE separately, an increased risk of cardiovascular ischaemia was observed in the romosozumab group (n = 2040) compared to the alendronate group (n = 2014) (OR 2.65, 95% CI 1.03–6.77) [102]. However, there was no increased risk of cerebrovascular disease (OR 2.27, 95% CI 0.93–5.22) or cardiovascular mortality (OR 1.42, 95% CI 0.68–2.97) when analysed in isolation, rather than being included with cardiovascular ischaemia in the MACE composite endpoint [102]. It is important to note that, in ARCH, any undisclosed cause of death was recorded as a cardiovascular death, which may have led to overestimation [99]. Interestingly, the incidence of heart failure, non-coronary revascularisation and peripheral vascular ischaemic events not requiring revascularisation was lower in the romosozumab arm [102].
A numerical preponderance towards cardiac adverse events was observed (as a non-primary outcome) in placeBo-contRolled study evaluatIng the efficacy anD safety of romosozumab in treatinG mEn with osteoporosis (BRIDGE) (which examined the bone health of 170 males) [119]. Only ten participants experienced positively adjudicated serious cardiovascular adverse events, 4.9% with romosozumab and 2.5% in the placebo group.
Therefore, the bulk of evidence against the cardiac safety of romosozumab comes from the ARCH trial [102]. This has been the subject of commentaries defining the possible explanations for the increased risk of MACE with romosozumab shown in this study as being due to increased cardiac risk of romosozumab, or the decreased cardiac risk with alendronate or the result of a chance finding [120].
Previously in this paper, we examined the potential cardiovascular protective effect of bisphosphonates and concluded that there was no robust evidence to support this supposition (particularly over the short, 12-month study period of ARCH). Indeed, there is evidence against either drug effect, as once participants were switched to alendronate, there was no change in cardiovascular disease risk [99]. Additionally, there was no apparent inflection of the slope of the cumulative incidence plot of time to first occurrence of MACE as participants switched from romosozumab to alendronate [99], suggesting that there was either no change in the risk of MACE or that the risk of MACE accrued by romosozumab was constant after the 12 months of treatment.
The ARCH population had significantly greater cardiovascular risk factors and a greater history of previous cardiovascular events than the FRAME population, which may have implications for the safety of the drug in an older population. In addition, when all the data were considered together, there were more deaths in patients aged over 75 years given the medicine [121]. However, subgroup analyses from ARCH demonstrated no difference in the cardiovascular risk between high- and low-risk subgroups (including those aged < 75 or ≥ 75, ever or never smokers and use of cardiovascular disease medications at baseline) [99].
When all these results were meta-analysed for the association between romosozumab and cardiovascular disease, the associations were non-significant for MACE (1.39, 95% CI 0.97–2.00) and serious adverse cardiovascular events (1.14, 95% CI 0.85–1.53). In support, a recent meta-analysis of six trials found a 39% increased risk of 4-point MACE (including death, MI, stroke and cardiac failure) with romosozumab, which was statistically significant [103]. When examining the cardiovascular adverse event profile of each arm in these trials, it is important to remember that the primary outcomes were efficacy rather than safety related. It is also important to note that the results of this meta-analysis are driven by the results of ARCH and that the marked differences in study populations and design make meta-analysis an ineffective approach for ARCH and FRAME [99].
The delay in the decision regarding the benefit–risk balance of romosozumab when considering cardiovascular safety is understandable. The studies undertaken in patients with a relatively mild deficit in bone mineral density (the best example of which is FRAME) suggest no increase in the risk of a major cardiovascular events, but appear to have equivocal benefits on non-spine fractures [100, 101]. However, those studies focussing on older, frail patients with more severe osteoporosis and previous fracture demonstrate marked effectiveness against recurrent fracture but an increased risk of MACE and cardiovascular ischaemia with romosozumab [102].
Debate may continue as to the extent to which the imbalance in cardiovascular events and mortality represents a protective effect of bisphosphonates on IHD compared to an adverse increase in risk attributable to romosozumab or whether it is a simply a chance effect [120].
For this reason, the EMA have reasonably concluded that romosozumab can be used for postmenopausal women with severe osteoporosis who are at a high risk of fracture, but not in those with a history of MI or stroke [121]. In those individuals with a high baseline cardiovascular risk, a robust risk–benefit assessment should be performed [99]. We now have to wait for data from pharmacovigilance studies that have been instigated worldwide to assess this benefit–risk balance in larger populations when drug use can be evaluated on a more routine clinical basis.
11 Conclusions
In conclusion, despite past studies demonstrating an association with coronary heart disease, there are no consistent data to suggest an association between calcium and coronary artery disease, and vitamin D supplementation does not appear to be associated with increased cardiac risk. There is a window of opportunity until 10 years after the menopause in which to use MHT without apparent detriment regarding cardiovascular disease. SERMs are associated with a significantly increased risk of VTE and may be associated with fatal stroke. Bisphosphonates cannot be recommended for cardiac benefit, and associations with atrial fibrillation are inconsistent. There is no evidence of adverse cardiac effects with denosumab or PTH analogues. The signal on cardiovascular disease adverse events with romosozumab needs post-marketing surveillance, which will be crucial in confirming cardiovascular safety.
References
**a W, Cooper C, Li M, et al. East meets West: current practices and policies in the management of musculoskeletal aging. Aging Clin Exp Res. 2019;31(10):1351–73. https://doi.org/10.1007/s40520-019-01282-8.
Chandran M, Tay D, Mithal A. Supplemental calcium intake in the aging individual: implications on skeletal and cardiovascular health. Aging Clin Exp Res. 2019;31(6):765–81. https://doi.org/10.1007/s40520-019-01150-5.
Prince RL, Devine A, Dhaliwal SS, et al. Effects of calcium supplementation on clinical fracture and bone structure: results of a 5-year, double-blind, placebo-controlled trial in elderly women. Arch Intern Med. 2006;166(8):869–75. https://doi.org/10.1001/archinte.166.8.869.
Bolland MJ, Barber PA, Doughty RN, et al. Vascular events in healthy older women receiving calcium supplementation: randomised controlled trial. BMJ. 2008;336(7638):262–6. https://doi.org/10.1136/bmj.39440.525752.BE.
Hsia J, Heiss G, Ren H, et al. Calcium/vitamin D supplementation and cardiovascular events. Circulation. 2007;115(7):846–54. https://doi.org/10.1161/circulationaha.106.673491.
Bolland MJ, Avenell A, Baron JA, et al. Effect of calcium supplements on risk of myocardial infarction and cardiovascular events: meta-analysis. BMJ. 2010;341:c3691. https://doi.org/10.1136/bmj.c3691.
Bolland MJ, Grey A, Avenell A, et al. Calcium supplements with or without vitamin D and risk of cardiovascular events: reanalysis of the Women’s Health Initiative limited access dataset and meta-analysis. BMJ. 2011;342:d2040. https://doi.org/10.1136/bmj.d2040.
Harvey NC, Biver E, Kaufman JM et al. (2017) The role of calcium supplementation in healthy musculoskeletal ageing: an expert consensus meeting of the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO) and the International Foundation for Osteoporosis (IOF). 28 (2):447-462. https://doi.org/10.1007/s00198-016-3773-6.
Prentice RL, Pettinger MB, Jackson RD, et al. Health risks and benefits from calcium and vitamin D supplementation: Women’s Health Initiative clinical trial and cohort study. Osteoporos Int. 2013;24(2):567–80. https://doi.org/10.1007/s00198-012-2224-2.
Cauley JA, Chlebowski RT, Wactawski-Wende J, et al. Calcium plus vitamin D supplementation and health outcomes five years after active intervention ended: the Women’s Health Initiative. J Women’s Health (2002). 2013;22(11):915–29. https://doi.org/10.1089/jwh.2013.4270.
Lewis JR, Radavelli-Bagatini S, Rejnmark L, et al. The effects of calcium supplementation on verified coronary heart disease hospitalization and death in postmenopausal women: a collaborative meta-analysis of randomized controlled trials. J Bone Miner Res. 2015;30(1):165–75. https://doi.org/10.1002/jbmr.2311.
Harvey NC, D’Angelo S, Paccou J, et al. Calcium and vitamin D supplementation are not associated with risk of incident ischemic cardiac events or death: findings from the UK Biobank Cohort. J Bone Miner Res. 2018;33(5):803–11. https://doi.org/10.1002/jbmr.3375.
Manson JE, Allison MA, Carr JJ, et al. Calcium/vitamin D supplementation and coronary artery calcification in the Women’s Health Initiative. Menopause. 2010;17(4):683–91. https://doi.org/10.1097/gme.0b013e3181d683b5.
Yang C, Shi X, **a H, et al. The evidence and controversy between dietary calcium intake and calcium supplementation and the risk of cardiovascular disease: a systematic review and meta-analysis of cohort studies and randomized controlled trials. J Am Coll Nutr. 2019. https://doi.org/10.1080/07315724.2019.1649219.
Heaney RP, Kopecky S, Maki KC, et al. A review of calcium supplements and cardiovascular disease risk. Adv Nutr. 2012;3(6):763–71. https://doi.org/10.3945/an.112.002899.
Cormick G, Ciapponi A, Cafferata ML, et al. Calcium supplementation for prevention of primary hypertension. Cochrane Database Syst Rev. 2015. https://doi.org/10.1002/14651858.cd010037.pub2.
Reid IR. Effects of calcium supplementation on circulating lipids: potential pharmacoeconomic implications. Drugs Aging. 2004;21(1):7–17. https://doi.org/10.2165/00002512-200421010-00002.
Goltzman D, Mannstadt M, Marcocci C. Physiology of the calcium-parathyroid hormone-vitamin D axis. Front Horm Res. 2018;50:1–13. https://doi.org/10.1159/000486060.
Kanis JA, Cooper C, Rizzoli R, et al. European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int. 2019;30(1):3–44. https://doi.org/10.1007/s00198-018-4704-5.
Pepe J, Cipriani C, Sonato C, et al. Cardiovascular manifestations of primary hyperparathyroidism: a narrative review. Eur J Endocrinol. 2017;177(6):R297–308. https://doi.org/10.1530/EJE-17-0485.
Bjerregaard P, Nallapaneni H, Gussak I. Short QT interval in clinical practice. J Electrocardiol. 2010;43(5):390–5. https://doi.org/10.1016/j.jelectrocard.2010.06.004.
Durup D, Jørgensen HL, Christensen J, et al. A reverse J-shaped association between serum 25-hydroxyvitamin D and cardiovascular disease mortality: the CopD study. J Clin Endocrinol Metab. 2015;100(6):2339–46. https://doi.org/10.1210/jc.2014-4551.
Ellam T, Hameed A, ul Haque R, et al. Vitamin D deficiency and exogenous vitamin D excess similarly increase diffuse atherosclerotic calcification in apolipoprotein E knockout mice. PLoS One. 2014;9(2):e88767. https://doi.org/10.1371/journal.pone.0088767.
Billington EO, Burt LA, Rose MS, et al. Safety of high-dose vitamin D supplementation: secondary analysis of a randomized controlled trial. J Clin Endocrinol Metab. 2019. https://doi.org/10.1210/clinem/dgz212.
Bouillon R. Vitamin D and cardiovascular disorders. Osteoporos Int. 2019;30(11):2167–81. https://doi.org/10.1007/s00198-019-05098-0.
Swart KM, Lips P, Brouwer IA, et al. Effects of vitamin D supplementation on markers for cardiovascular disease and type 2 diabetes: an individual participant data meta-analysis of randomized controlled trials. AM J Clin Nutr. 2018;107(6):1043–53. https://doi.org/10.1093/ajcn/nqy078.
Manson JE, Cook NR, Lee IM, et al. Vitamin D supplements and prevention of cancer and cardiovascular disease. N Engl J Med. 2019;380(1):33–44. https://doi.org/10.1056/NEJMoa1809944.
Scragg R, Stewart AW, Waayer D, et al. Effect of monthly high-dose vitamin D supplementation on cardiovascular disease in the Vitamin D Assessment Study: a randomized clinical trial. JAMA Cardiol. 2017;2(6):608–16. https://doi.org/10.1001/jamacardio.2017.0175.
Barbarawi M, Kheiri B, Zayed Y, et al. Vitamin D supplementation and cardiovascular disease risks in more than 83 000 individuals in 21 randomized clinical trials: a meta-analysis. JAMA Cardiol. 2019;4(8):765–75. https://doi.org/10.1001/jamacardio.2019.1870.
Kanis JA, Cooper C, Rizzoli R, et al. Executive summary of European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Aging Clin Exp Res. 2019;31(1):15–7. https://doi.org/10.1007/s40520-018-1109-4.
Grübler MR, März W, Pilz S, et al. Vitamin-D concentrations, cardiovascular risk and events—a review of epidemiological evidence. Rev Endocr Metab Disord. 2017;18(2):259–72. https://doi.org/10.1007/s11154-017-9417-0.
Zhu L, Jiang X, Sun Y, et al. Effect of hormone therapy on the risk of bone fractures: a systematic review and meta-analysis of randomized controlled trials. Menopause. 2016;23(4):461–70. https://doi.org/10.1097/gme.0000000000000519.
Kannel WB, Hjortland MC, McNamara PM, et al. Menopause and risk of cardiovascular disease: the Framingham study. Ann Intern Med. 1976;85(4):447–52. https://doi.org/10.7326/0003-4819-85-4-447.
Rivera CM, Grossardt BR, Rhodes DJ, et al. Increased cardiovascular mortality after early bilateral oophorectomy. Menopause (New York, NY). 2009;16(1):15–23. https://doi.org/10.1097/gme.0b013e31818888f7.
Lisabeth LD, Beiser AS, Brown DL, et al. Age at natural menopause and risk of ischemic stroke: the Framingham Heart Study. Stroke. 2009;40(4):1044–9. https://doi.org/10.1161/STROKEAHA.108.542993.
Bassuk SS, Manson JE. The Timing Hypothesis: do coronary risks of menopausal hormone therapy vary by age or time since menopause onset? Metab Clin Exp. 2016;65(5):794–803. https://doi.org/10.1016/j.metabol.2016.01.004.
Chester RC, Kling JM, Manson JE. What the Women’s Health Initiative has taught us about menopausal hormone therapy. Clin Cardiol. 2018;41(2):247–52. https://doi.org/10.1002/clc.22891.
Hernán MA, Alonso A, Logan R, et al. Observational studies analyzed like randomized experiments: an application to postmenopausal hormone therapy and coronary heart disease. Epidemiology (Cambridge, Mass). 2008;19(6):766–79. https://doi.org/10.1097/EDE.0b013e3181875e61.
Rossouw JE, Anderson GL, Prentice RL, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288(3):321–33. https://doi.org/10.1093/ajcn/nqy078.
Hersh AL, Stefanick ML, Stafford RS. National use of postmenopausal hormone therapy: annual trends and response to recent evidence. JAMA. 2004;291(1):47–53. https://doi.org/10.1001/jama.291.1.47.
Simon JA. What’s new in hormone replacement therapy: focus on transdermal estradiol and micronized progesterone. Clim J Int Menopause Soc. 2012;15(Suppl 1):3–10. https://doi.org/10.3109/13697137.2012.669332.
Cushman M, Kuller LH, Prentice R, et al. Estrogen plus progestin and risk of venous thrombosis. JAMA. 2004;292(13):1573–80. https://doi.org/10.1001/jama.292.13.1573.
Wassertheil-Smoller S, Hendrix SL, Limacher M, et al. Effect of estrogen plus progestin on stroke in postmenopausal women: the Women’s Health Initiative: a randomized trial. JAMA. 2003;289(20):2673–84. https://doi.org/10.1001/jama.289.20.2673.
Manson JE, Hsia J, Johnson KC, et al. Estrogen plus progestin and the risk of coronary heart disease. N Engl J Med. 2003;349(6):523–34. https://doi.org/10.1056/NEJMoa030808.
Curb JD, Prentice RL, Bray PF, et al. Venous thrombosis and conjugated equine estrogen in women without a uterus. Arch Intern Med. 2006;166(7):772–80. https://doi.org/10.1001/archinte.166.7.772.
Hendrix SL, Wassertheil-Smoller S, Johnson KC, et al. Effects of conjugated equine estrogen on stroke in the Women’s Health Initiative. Circulation. 2006;113(20):2425–34. https://doi.org/10.1161/CIRCULATIONAHA.105.594077.
Rossouw JE, Prentice RL, Manson JE, et al. Postmenopausal hormone therapy and risk of cardiovascular disease by age and years since menopause. JAMA. 2007;297(13):1465–77. https://doi.org/10.1001/jama.297.13.1465.
Santen RJ, Allred DC, Ardoin SP, et al. Postmenopausal hormone therapy: an Endocrine Society scientific statement. J Clin Endocrinol Metab. 2010;95(7 Suppl 1):s1–66. https://doi.org/10.1210/jc.2009-2509.
Mikkola TS, Clarkson TB. Estrogen replacement therapy, atherosclerosis, and vascular function. Cardiovasc Res. 2002;53(3):605–19. https://doi.org/10.1016/s0008-6363(01)00466-7.
Hodis HN, Collins P, Mack WJ, et al. The timing hypothesis for coronary heart disease prevention with hormone therapy: past, present and future in perspective. Clim J Int Menopause Soc. 2012;15(3):217–28. https://doi.org/10.3109/13697137.2012.656401.
Harman SM, Black DM, Naftolin F, et al. Arterial imaging outcomes and cardiovascular risk factors in recently menopausal women: a randomized trial. Ann Intern Med. 2014;161(4):249–60. https://doi.org/10.7326/M14-0353.
Hodis HN, Mack WJ, Henderson VW, et al. Vascular effects of early versus late postmenopausal treatment with estradiol. N Engl J Med. 2016;374(13):1221–31. https://doi.org/10.1056/NEJMoa1505241.
Baber RJ, Panay N, Fenton A, et al. 2016 IMS recommendations on women’s midlife health and menopause hormone therapy. Clim J Int Menopause Soc. 2016;19(2):109–50. https://doi.org/10.3109/13697137.2015.1129166.
Canonico M, Scarabin PY. Oral versus transdermal estrogens and venous thromboembolism in postmenopausal women: what is new since 2003? Menopause. 2016;23(6):587–8. https://doi.org/10.1097/gme.0000000000000665.
Vinogradova Y, Coupland C, Hippisley-Cox J. Use of hormone replacement therapy and risk of venous thromboembolism: nested case-control studies using the QResearch and CPRD databases. BMJ. 2019;364:k4810. https://doi.org/10.1136/bmj.k4810.
Sturdee DW, Pines A, International Menopause Society Writing G, et al. Updated IMS recommendations on postmenopausal hormone therapy and preventive strategies for midlife health. Clim J Int Menopause Soc. 2011;14(3):302–20. https://doi.org/10.3109/13697137.2011.570590.
Manson JE, Kaunitz AM. Menopause management–getting clinical care back on track. N Engl J Med. 2016;374(9):803–6. https://doi.org/10.1056/NEJMp1514242.
Yates J, Barrett-Connor E, Barlas S, et al. Rapid loss of hip fracture protection after estrogen cessation: evidence from the National Osteoporosis Risk Assessment. Obstet Gynecol. 2004;103(3):440–6. https://doi.org/10.1097/01.aog.0000114986.14806.37.
Menopause: diagnosis and management; NG23. National Institute for Health and Care Excellence, London. 2015.
Cummings SR, Ettinger B, Delmas PD, et al. The effects of tibolone in older postmenopausal women. N Engl J Med. 2008;359(7):697–708. https://doi.org/10.1056/NEJMoa0800743.
Walsh BW, Kuller LH, Wild RA, et al. Effects of raloxifene on serum lipids and coagulation factors in healthy postmenopausal women. JAMA. 1998;279(18):1445–51. https://doi.org/10.1001/jama.279.18.1445.
Gol M, Akan P, Dogan E, et al. Effects of estrogen, raloxifene, and hormone replacement therapy on serum C-reactive protein and homocysteine levels. Maturitas. 2006;53(3):252–9. https://doi.org/10.1016/j.maturitas.2005.05.006.
Nanetti L, Camilletti A, Francucci CM, et al. Role of raloxifene on platelet metabolism and plasma lipids. Eur J Clin Invest. 2008;38(2):117–25. https://doi.org/10.1111/j.1365-2362.2007.01905.x.
Grover-Páez F, Zavalza-Gómez AB, Anaya-Prado R. Raloxifene modifies the insulin sensitivity and lipid profile of postmenopausal insulin resistant women. Gynecol Endocrinol. 2013;29(7):674–7. https://doi.org/10.3109/09513590.2013.788628.
Colacurci N, Manzella D, Fornaro F, et al. Endothelial function and menopause: effects of raloxifene administration. J Clin Endocrinol Metab. 2003;88(5):2135–40. https://doi.org/10.1210/jc.2002-021557.
Cagnacci A, Zanni AL, Volpe A. Administration of raloxifene does not influence 24-hour ambulatory blood pressure of postmenopausal women with osteopenia: a double-blind placebo-controlled study. Am J Obstet Gynecol. 2003;188(5):1278–82. https://doi.org/10.1067/mob.2003.299.
Adomaityte J, Farooq M, Qayyum R. Effect of raloxifene therapy on venous thromboembolism in postmenopausal women. A meta-analysis. Thromb Haemost. 2008;99(2):338–42.
Cummings SR, Ensrud K, Delmas PD, et al. Lasofoxifene in postmenopausal women with osteoporosis. N Engl J Med. 2010;362(8):686–96. https://doi.org/10.1056/NEJMoa0808692.
Barrett-Connor E, Grady D, Sashegyi A, et al. Raloxifene and cardiovascular events in osteoporotic postmenopausal women: four-year results from the MORE (Multiple Outcomes of Raloxifene Evaluation) randomized trial. JAMA. 2002;287(7):847–57. https://doi.org/10.1001/jama.287.7.847.
Ensrud K, Genazzani AR, Geiger MJ, et al. Effect of raloxifene on cardiovascular adverse events in postmenopausal women with osteoporosis. Am J Cardiol. 2006;97(4):520–7. https://doi.org/10.1016/j.amjcard.2005.09.083.
Barrett-Connor E, Mosca L, Collins P, et al. Effects of raloxifene on cardiovascular events and breast cancer in postmenopausal women. N Engl J Med. 2006;355(2):125–37. https://doi.org/10.1056/NEJMoa062462.
Ensrud K, LaCroix A, Thompson JR, et al. Lasofoxifene and cardiovascular events in postmenopausal women with osteoporosis: five-year results from the Postmenopausal Evaluation and Risk Reduction with Lasofoxifene (PEARL) trial. Circulation. 2010;122(17):1716–24. https://doi.org/10.1161/CIRCULATIONAHA.109.924571.
McFarlane SI, Muniyappa R, Shin JJ, et al. Osteoporosis and cardiovascular disease: brittle bones and boned arteries, is there a link? Endocrine. 2004;23(1):1–10. https://doi.org/10.1385/ENDO:23:1:01.
Bevilacqua M, Dominguez LJ, Rosini S, et al. Bisphosphonates and atherosclerosis: why? Lupus. 2005;14(9):773–9. https://doi.org/10.1191/0961203305lu2219oa.
Wagner WD, Clarkson TB, Foster J. Contrasting effects of ethane-1-hydroxy-1,1-diphosphonate (EHDP) on the regression of two types of dietary-induced atherosclerosis. Atherosclerosis. 1977;27(4):419–35. https://doi.org/10.1016/0021-9150(77)90161-7.
Kramsch DM, Aspen AJ, Rozler LJ. Atherosclerosis: prevention by agents not affecting abnormal levels of blood lipids. Science (New York, NY). 1981;213(4515):1511–2. https://doi.org/10.1126/science.6792706.
Gonnelli S, Caffarelli C, Tanzilli L, et al. Effects of intravenous zoledronate and ibandronate on carotid intima-media thickness, lipids and FGF-23 in postmenopausal osteoporotic women. Bone. 2014;61:27–32. https://doi.org/10.1016/j.bone.2013.12.017.
Yang Y, Rong X, Lv X, et al. Inhibition of mevalonate pathway prevents ischemia-induced cardiac dysfunction in rats via RhoA-independent signaling pathway. Cardiovasc Ther. 2017. https://doi.org/10.1111/1755-5922.12285.
Zhou S, Fang X, **n H, et al. Effects of alendronate on the Notch1-RBP-Jκ signaling pathway in the osteogenic differentiation and mineralization of vascular smooth muscle cells. Mol Med Rep. 2013;8(1):89–94. https://doi.org/10.3892/mmr.2013.1489.
Giollo A, Rossini M, Gatti D, et al. Amino-bisphosphonates and cardiovascular risk: a new hypothesis involving the effects on gamma-delta T cells. J Bone Miner Res. 2019;34(3):570–1. https://doi.org/10.1002/jbmr.3660.
Steinbuch M, D’Agostino RB, Mandel JS, et al. Assessment of mortality in patients enrolled in a risedronate clinical trial program: a retrospective cohort study. Regulatory toxicology and pharmacology: RTP. 2002;35(3):320–6. https://doi.org/10.1006/rtph.2002.1550.
Black DM, Delmas PD, Eastell R, et al. Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med. 2007;356(18):1809–22. https://doi.org/10.1056/NEJMoa067312.
Lyles KW, Colón-Emeric CS, Magaziner JS, et al. Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med. 2007;357(18):1799–809. https://doi.org/10.1056/NEJMoa074941.
Reid IR, Horne AM, Mihov B, et al. Fracture prevention with zoledronate in older women with osteopenia. N Engl J Med. 2018;379(25):2407–16. https://doi.org/10.1056/NEJMoa1808082.
Reid IR, Horne AM, Mihov B, et al. Effects of zoledronate on cancer, cardiac events, and mortality in osteopenic older women. J Bone Miner Res. 2020;35(1):20–7. https://doi.org/10.1002/jbmr.3860.
Bunch TJ, Anderson JL, May HT, et al. Relation of bisphosphonate therapies and risk of develo** atrial fibrillation. The American journal of cardiology. 2009;103(6):824–8. https://doi.org/10.1016/j.amjcard.2008.11.037.
Cummings SR, Lui L-Y, Eastell R, et al. Association between drug treatments for patients with osteoporosis and overall mortality rates: a meta-analysis. JAMA Intern Med. 2019. https://doi.org/10.1001/jamainternmed.2019.2779.
Black DM, Thompson DE, Bauer DC, et al. Fracture risk reduction with alendronate in women with osteoporosis: the Fracture Intervention Trial. FIT Research Group. J Clin Endocrinol Metab. 2000;85(11):4118–24. https://doi.org/10.1210/jcem.85.11.6953.
Heckbert SR, Li G, Cummings SR, et al. Use of alendronate and risk of incident atrial fibrillation in women. Arch Intern Med. 2008;168(8):826–31. https://doi.org/10.1001/archinte.168.8.826.
Sørensen HT, Christensen S, Mehnert F, et al. Use of bisphosphonates among women and risk of atrial fibrillation and flutter: population based case-control study. BMJ (Clin Res ed). 2008;336(7648):813–6. https://doi.org/10.1136/bmj.39507.551644.BE.
Abrahamsen B, Eiken P, Brixen K. Atrial fibrillation in fracture patients treated with oral bisphosphonates. J Intern Med. 2009;265(5):581–92. https://doi.org/10.1111/j.1365-2796.2008.02065.x.
Cummings SR, San Martin J, McClung MR, et al. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med. 2009;361(8):756–65. https://doi.org/10.1056/NEJMoa0809493.
Samelson EJ, Miller PD, Christiansen C, et al. RANKL inhibition with denosumab does not influence 3-year progression of aortic calcification or incidence of adverse cardiovascular events in postmenopausal women with osteoporosis and high cardiovascular risk. J Bone Miner Res. 2014;29(2):450–7. https://doi.org/10.1002/jbmr.2043.
Jordan LR, Dallemagne CR, Cross RB. Cardiovascular effects of parathyroid hormone in conscious sheep. Exp Physiol. 1991;76(2):251–7. https://doi.org/10.1113/expphysiol.1991.sp003491.
Kendler DL, Marin F, Zerbini CAF, et al. Effects of teriparatide and risedronate on new fractures in post-menopausal women with severe osteoporosis (VERO): a multicentre, double-blind, double-dummy, randomised controlled trial. Lancet. 2018;391(10117):230–40. https://doi.org/10.1016/s0140-6736(17)32137-2.
Nishikawa A, Ishida T, Taketsuna M, et al. Safety and effectiveness of daily teriparatide in a prospective observational study in patients with osteoporosis at high risk of fracture in Japan: final report. Clin Interv Aging. 2016;11:913–25. https://doi.org/10.2147/CIA.S107285.
Miller PD, Hattersley G, Riis BJ, et al. Effect of abaloparatide vs placebo on new vertebral fractures in postmenopausal women with osteoporosis: a randomized clinical trial. JAMA. 2016;316(7):722–33. https://doi.org/10.1001/jama.2016.11136.
Final summary minutes of the Bone, Reproductive and Urologic Drugs Advisory Committee Meeting (January 16). Food and Drug Administration, Center for Drug Evaluation and Research. 2019.
Evenity: EPAR public assessment report. European Medicines Agency. 2019.
Cosman F, Crittenden DB, Ferrari S, et al. FRAME Study: the foundation effect of building bone with 1 year of romosozumab leads to continued lower fracture risk after transition to denosumab. J Bone Miner Res. 2018;33(7):1219–26. https://doi.org/10.1002/jbmr.3427.
Cosman F, Crittenden DB, Adachi JD, et al. Romosozumab treatment in postmenopausal women with osteoporosis. N Engl J Med. 2016;375(16):1532–43. https://doi.org/10.1056/NEJMoa1607948.
Saag KG, Petersen J, Brandi ML, et al. Romosozumab or alendronate for fracture prevention in women with osteoporosis. N Engl J Med. 2017;377(15):1417–27. https://doi.org/10.1056/NEJMoa1708322.
Lv F, Cai X, Yang W, et al. Denosumab or romosozumab therapy and risk of cardiovascular events in patients with primary osteoporosis: systematic review and meta- analysis. Bone. 2020;130:115121. https://doi.org/10.1016/j.bone.2019.115121.
Shoback D, Rosen CJ, Black DM, et al. Pharmacological management of osteoporosis in postmenopausal women: an Endocrine Society Guideline update. J Clin Endocrinol Metab. 2020. https://doi.org/10.1210/clinem/dgaa048.
Appelman-Dijkstra NM, Papapoulos SE. Clinical advantages and disadvantages of anabolic bone therapies targeting the WNT pathway. Nat Rev Endocrinol. 2018;14(10):605–23. https://doi.org/10.1038/s41574-018-0087-0.
Zhu D, Mackenzie NC, Millan JL, et al. The appearance and modulation of osteocyte marker expression during calcification of vascular smooth muscle cells. PLoS ONE. 2011;6(5):e19595. https://doi.org/10.1371/journal.pone.0019595.
Evenepoel P, Goffin E, Meijers B, et al. Sclerostin serum levels and vascular calcification progression in prevalent renal transplant recipients. J Clin Endocrinol Metab. 2015;100(12):4669–76. https://doi.org/10.1210/jc.2015-3056.
Krishna SM, Seto SW, Jose RJ, et al. Wnt signaling pathway inhibitor sclerostin inhibits angiotensin II-induced aortic aneurysm and atherosclerosis. Arterioscler Thromb Vasc Biol. 2017;37(3):553–66. https://doi.org/10.1161/atvbaha.116.308723.
Javaheri B, Herbert E, Hopkinson M, et al. Sost haploinsufficiency provokes peracute lethal cardiac tamponade without rescuing the osteopenia in a mouse model of excess glucocorticoids. Am J Pathol. 2019;189(4):753–61. https://doi.org/10.1016/j.ajpath.2018.12.007.
Kuipers AL, Miljkovic I, Barinas-Mitchell E, et al. Wnt pathway gene expression is associated with arterial stiffness. J Am Heart Assoc. 2020;9(3):e014170. https://doi.org/10.1161/jaha.119.014170.
Florio M, Gunasekaran K, Stolina M, et al. A bispecific antibody targeting sclerostin and DKK-1 promotes bone mass accrual and fracture repair. Nat Commun. 2016;7:11505. https://doi.org/10.1038/ncomms11505.
Di M, Wang L, Li M, et al. Dickkopf1 destabilizes atherosclerotic plaques and promotes plaque formation by inducing apoptosis of endothelial cells through activation of ER stress. Cell Death Dis. 2017;8(7):e2917. https://doi.org/10.1038/cddis.2017.277.
Moe SM, Chen NX, Newman CL, et al. Anti-sclerostin antibody treatment in a rat model of progressive renal osteodystrophy. J Bone Miner Res. 2015;30(3):499–509. https://doi.org/10.1002/jbmr.2372.
Ominsky MS, Boyd SK, Varela A, et al. Romosozumab improves bone mass and strength while maintaining bone quality in ovariectomized cynomolgus monkeys. J Bone Miner Res. 2017;32(4):788–801. https://doi.org/10.1002/jbmr.3036.
Balemans W, Van Hul W. Identification of the disease-causing gene in sclerosteosis–discovery of a novel bone anabolic target? J Musculoskelet Neuronal Interact. 2004;4(2):139–42.
van Lierop AH, Appelman-Dijkstra NM, Papapoulos SE. Sclerostin deficiency in humans. Bone. 2017;96:51–62. https://doi.org/10.1016/j.bone.2016.10.010.
Hamersma H, Gardner J, Beighton P. The natural history of sclerosteosis. Clin Genet. 2003;63(3):192–7. https://doi.org/10.1034/j.1399-0004.2003.00036.x.
Lewiecki EM, Dinavahi RV, Lazaretti-Castro M, et al. One year of romosozumab followed by two years of denosumab maintains fracture risk reductions: results of the FRAME Extension study. J Bone Miner Res. 2019;34(3):419–28. https://doi.org/10.1002/jbmr.3622.
Lewiecki EM, Blicharski T, Goemaere S, et al. A phase III randomized placebo-controlled trial to evaluate efficacy and safety of romosozumab in men with osteoporosis. J Clin Endocrinol Metab. 2018;103(9):3183–93. https://doi.org/10.1210/jc.2017-02163.
Cummings SR, McCulloch C. Explanations for the difference in rates of cardiovascular events in a trial of alendronate and romosozumab. Osteoporos Int. 2020. https://doi.org/10.1007/s00198-020-05379-z.
Approval of the marketing authorisation for Evenity (romosozumab): re-examination leads to recommendation to approve. 2019.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The ESCEO Working Group was funded by the ESCEO. The ESCEO receives unrestricted educational grants to support its educational and scientific activities from non-governmental organisations, not-for-profit organisations, non-commercial or corporate partners. The choice of topics, participants, content and agenda of the Working Groups as well as the writing, editing, submission and reviewing of the manuscript are the sole responsibility of the ESCEO, without any influence from third parties.
Conflicts of interest
NRF, AC, JMK, NA, CC have nothing to disclose. FT reports personal fees for lectures and expertise from Amgen, Arrow, Lilly France, TEVA and Theramex and non-financial support from Besins Healthcare France. MLB reports honoraria from Amgen, Bruno Farmaceutici, Calcilytix and Kyowa Kirin, academic grants and/or speaker fees from Abiogen, Alexion, Amgen, Bruno Farmaceutici, Eli Lilly, Kyowa Kirin, MSD, NPS Pharma, Servier, Shire and Spa and consultancy work for Alexion, Bruno Farmaceutici, Kyowa Kirin, Servier and Shire. SR reports advisory board participation, consultancy work, speakers’ fees and research grants from Mylan, Abbot, Amgen, Ceres and Gilead. NCH reports consultancy work and lecture fees and honoraria from Alliance for Better Bone Health, Amgen, MSD, Eli Lilly, Servier, Shire, UCB, Kyowa Kirin, Consilient Healthcare, Radius Health and Internis Pharma. DPA’s research group has received research grants from Amgen, Servier and UCB and speaker tuition fees and advisory or consultancy fees (all paid to his department) from Amgen and UCB. TT reports personal fees for lectures and expertise from Amgen, Arrow, Biogen, BMS, Chugai, Expanscience, Gilead, Grunenthal, LCA, Lilly, Medac, MSD, Nordic, Novartis, Pfizer, Sandoz, Sanofi, Theramex, Thuasne, TEVA and UCB and reports financial support or fees for research activities from Amgen, Bone Therapeutics, Chugai, MSD, Novartis, Pfizer and UCB. EMD reports consultancy fees for UCB and Pfizer. JAK reports institutional grant support from Radius Health and Amgen. JYR reports consulting fees or advisory board participation for IBSA-Genevrier, Mylan, Radius Health and Pierre Fabre, lecturing fees for IBSA-Genevrier, Mylan, Cniel and Dairy Research Council (DRC) and grant support from IBSA-Genevrier, Mylan, Cniel and Radius Health. RR reports speaker fees from Abiogen, Amgen, EMF and Sandoz and advisory board fees from Echolight, Mylan, ObsEva, Rejuvenate and Theramex. OB reports grants from Biophytis, IBSA, MEDA, Servier and SMB and personal fees from Amgen, Aptissen, Biophytis, IBSA, MEDA, Sanofi, Servier, SMB and UCB. ADP reports speaker and advisory fees from Amgen, Lilly, Theramex, UCB and Sandoz.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Fuggle, N.R., Cooper, C., Harvey, N.C. et al. Assessment of Cardiovascular Safety of Anti-Osteoporosis Drugs. Drugs 80, 1537–1552 (2020). https://doi.org/10.1007/s40265-020-01364-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-020-01364-2