Abstract
Background and Objective
Aberrant accumulation of glycosphingolipids (GSLs) in the lysosome leads to GSL storage diseases. Glucosylceramide synthase inhibitors (GCSi) have the potential to treat several GSL storage diseases by reducing the synthesis of the disease-causing GSLs. AL01211 is a potent oral GCSi under investigation for Type 1 Gaucher disease and Fabry disease. Here, we evaluate the pharmacokinetics, pharmacodynamics, safety, and tolerability of AL01211 in healthy Chinese volunteers.
Methods
AL01211 was tested in a Phase 1, single-center, randomized, double-blind, placebo-controlled study with single-dose (15 and 60 mg) and multiple-dose (30 mg) arms.
Results
Results of AL01211 demonstrated dose-dependent pharmacokinetics, rapid absorption (median time to maximum plasma concentration [tmax] 2.5–4 hours), relatively slow clearance rate (mean apparent total clearance from plasma [CL/F] 88.3–200 L/h) and the mean terminal half-life above 30 hours. Repeated once-daily oral administration of AL01211 for 14 days had an approximately 2-fold accumulation, reaching steady-state levels between 7 and 10 days, and led to a 73% reduction in plasma glucosylceramide (GL1) on Day 14. AL01211 was safe and well tolerated, with no identified serious adverse events.
Conclusion
AL01211 showed a favorable pharmacokinetic, pharmacodynamics, safety, and tolerability profile in healthy Chinese volunteers. These data support the further clinical development of AL01211 as a therapy for GSL storage diseases.
Clinical Trial Registry
Clinical Trial Registry no. CTR20221202 (http://www.chinadrugtrials.org.cn) registered on 6 June 2022 and ChiCTR2200061431 (http://www.chictr.org.cn) registered on 24 June 2022.


Similar content being viewed by others
References
Breiden B, Sandhoff K. Lysosomal glycosphingolipid storage diseases. Annu Rev Biochem. 2019;20(88):461–85.
Xu YH, Barnes S, Sun Y, Grabowski GA. Multi-system disorders of glycosphingolipid and ganglioside metabolism. J Lipid Res. 2010;51(7):1643–75.
Stone WL, Basit H, Mukkamalla SKR, et al. Gaucher Disease. [Updated 2023 Nov 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448080/.
Hughes DA, Pastores GM. Gaucher disease. In: Adam MP, Feldman J, Mirzaa GM, Pagon RA, Wallace SE, Bean LJH, et al. (eds) GeneReviews((R)), Seattle 1993.
Schiffmann R. Fabry disease. Handb Clin Neurol. 2015;132:231–48.
Clarke JT. Narrative review: Fabry disease. Ann Intern Med. 2007;146(6):425–33.
Solomon M, Muro S. Lysosomal enzyme replacement therapies: historical development, clinical outcomes, and future perspectives. Adv Drug Deliv Rev. 2017;1(118):109–34.
Azevedo O, Gago MF, Miltenberger-Miltenyi G, Sousa N, Cunha D. Fabry disease therapy: state-of-the-art and current challenges. Int J Mol Sci. 2020;22(1):206.
Mehta A. Gaucher disease: unmet treatment needs. Acta Paediatr. 2008;97(457):83–7.
Kido J, Sugawara K, Nakamura K. Gene therapy for lysosomal storage diseases: current clinical trial prospects. Front Genet. 2023;14:1064924.
Weidemann F, Jovanovic A, Herrmann K, Vardarli I. Chaperone therapy in Fabry disease. Int J Mol Sci. 2022;23(3):1887.
Hughes DA, Nicholls K, Shankar SP, Sunder-Plassmann G, Koeller D, Nedd K, et al. Oral pharmacological chaperone migalastat compared with enzyme replacement therapy in Fabry disease: 18-month results from the randomised phase III ATTRACT study. J Med Genet. 2017;54(4):288–96.
Yu RK, Tsai YT, Ariga T, Yanagisawa M. Structures, biosynthesis, and functions of gangliosides–an overview. J Oleo Sci. 2011;60(10):537–44.
Cox TM, Drelichman G, Cravo R, Balwani M, Burrow TA, Martins AM, et al. Eliglustat maintains long-term clinical stability in patients with Gaucher disease type 1 stabilized on enzyme therapy. Blood. 2017;129(17):2375–83.
Nabizadeh A, Amani B, Kadivar M, Toroski M, Asl AA, Bayazidi Y, et al. The clinical efficacy of imiglucerase versus eliglustat in patients with Gaucher’s disease type 1: a systematic review. J Res Pharm Pract. 2018;7(4):171–7.
Peterschmitt MJ, Crawford NPS, Gaemers SJM, Ji AJ, Sharma J, Pham TT. Pharmacokinetics, pharmacodynamics, safety, and tolerability of oral venglustat in healthy volunteers. Clin Pharmacol Drug Dev. 2021;10(1):86–98.
Deegan PB, Goker-Alpan O, Geberhiwot T, Hopkin RJ, Lukina E, Tylki-Szymanska A, et al. Venglustat, an orally administered glucosylceramide synthase inhibitor: assessment over 3 years in adult males with classic Fabry disease in an open-label phase 2 study and its extension study. Mol Genet Metab. 2023;138(2): 106963.
Schiffmann R, Cox TM, Dedieu JF, Gaemers SJM, Hennermann JB, Ida H, et al. Venglustat combined with imiglucerase for neurological disease in adults with Gaucher disease type 3: the LEAP trial. Brain. 2023;146(2):461–74.
Giladi N, Alcalay RN, Cutter G, Gasser T, Gurevich T, Hoglinger GU, et al. Safety and efficacy of venglustat in GBA1-associated Parkinson’s disease: an international, multicentre, double-blind, randomised, placebo-controlled, phase 2 trial. Lancet Neurol. 2023;22(8):661–71.
Gansevoort RT, Hariri A, Minini P, Ahn C, Chapman AB, Horie S, et al. Venglustat, a novel glucosylceramide synthase inhibitor, in patients at risk of rapidly progressing ADPKD: primary results of a double-blind, placebo-controlled, phase 2/3 randomized clinical trial. Am J Kidney Dis. 2023;81(5):517-27.e1.
Guerard N, Oder D, Nordbeck P, Zwingelstein C, Morand O, Welford RWD, et al. Lucerastat, an iminosugar for substrate reduction therapy: tolerability, pharmacodynamics, and pharmacokinetics in patients with Fabry disease on enzyme replacement. Clin Pharmacol Ther. 2018;103(4):703–11.
Guerard N, Zwingelstein C, Dingemanse J. Lucerastat, an iminosugar for substrate reduction therapy: pharmacokinetics, tolerability, and safety in subjects with mild, moderate, and severe renal function impairment. J Clin Pharmacol. 2017;57(11):1425–31.
Babcock M, Zheng J, Li L, Garovoy M, Shen Y. Development of AL01211, a novel glucosylceramide synthase inhibitor, to treat Fabry disease. In: 7th International Update on Fabry Disease. 29–31 May 2022; Würzburg, Germany.
Babcock M, Zheng J, Gail Shurr J, Li L, Wang B, Huertas P, et al. Phase 1 healthy volunteer study of AL01211, an oral, non-brain penetrant glucosylceramide synthase inhibitor, to treat Fabry disease and type 1 Gaucher disease. Clin Pharmacol Drug Dev. 2024. https://doi.org/10.1002/cpdd.1375.
Peterschmitt MJ, Burke A, Blankstein L, Smith SE, Puga AC, Kramer WG, et al. Safety, tolerability, and pharmacokinetics of eliglustat tartrate (Genz-112638) after single doses, multiple doses, and food in healthy volunteers. J Clin Pharmacol. 2011;51(5):695–705.
Cox TM. Eliglustat tartrate, an orally active glucocerebroside synthase inhibitor for the potential treatment of Gaucher disease and other lysosomal storage diseases. Curr Opin Investig Drugs. 2010;11(10):1169–81.
Babcock M. Development of AL01211, an oral, non-brain penetrant glucosylceramide synthase inhibitor (GCSi), to treat Fabry disease. Poster LB-08 presented at the WORLD Symposium. February 23, 2023; Orlando, Fl.
Wanner C, Kimonis V, Politei J, Warnock DG, Uceyler N, Frey A, et al. Understanding and modifying Fabry disease: rationale and design of a pivotal Phase 3 study and results from a patient-reported outcome validation study. Mol Genet Metab Rep. 2022;31: 100862.
Hasunuma T, Tohkin M, Kaniwa N, Jang IJ, Yimin C, Kaneko M, et al. Absence of ethnic differences in the pharmacokinetics of moxifloxacin, simvastatin, and meloxicam among three East Asian populations and Caucasians. Br J Clin Pharmacol. 2016;81(6):1078–90.
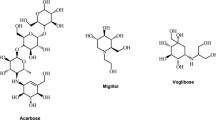
Belmatoug N, Burlina A, Giraldo P, Hendriksz CJ, Kuter DJ, Mengel E, et al. Gastrointestinal disturbances and their management in miglustat-treated patients. J Inherit Metab Dis. 2011;34(5):991–1001.
Acknowledgments
The study was managed by the clinical CRO Hangzhou Tigermed Consulting Co., Ltd and conducted at the Second Hospital of Anhui Medical University Phase 1 Unit in Hefei, China. The bioanalytical work (pharmacokinetic and GL1 measurements) was performed at Wu** Tan, Marvin Garovoy & Jianhong Zheng
Corresponding authors
Ethics declarations
Funding
This study was funded by AceLink Therapeutics, Inc.
Conflict of interest
J.X., M.B., Y.S., L.L., and J.Z. are full-time employees of AceLink Therapeutics. L.T. and M.G. were AceLink Therapeutics employees at the time of this study. L.D., Y.C., Y.W., and W.H. have no relevant financial or non-financial competing interests to report.
Ethical approval
This study was approved by the Ethics Committee of the Second Hospital of Anhui Medical University (approval number: YW2022-050(F1); approval date: 25 April 2022) and was conducted in accordance with the Declaration of Helsinki and International Council for Harmonisation (ICH) guidelines for Good Clinical Practice (GCP).
Consent to participate
All volunteers gave their written informed consent prior to any study-related procedure.
Consent for publication
Not applicable.
Availability of data and material
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
Author contributions
M.B., J.Z., Y.S., M.G., and W.H. were responsible for study concept and study design. L.D., Y.C., Y.W., L.L., L.T., W.H., and J.Z. were responsible for study conduct and data acquisition. L.D., J.X., M.B., W.H., and J.Z. were responsible for analysis and interpretation. J.X. was responsible for original draft preparation. M.B., L.D., Y.S., M.G., J.Z., and W.H. were responsible for draft review and editing. All authors have read and agreed to the final version of this manuscript.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dong, L., **ang, J., Babcock, M. et al. Pharmacokinetics, Pharmacodynamics, Safety, and Tolerability of Oral AL01211 in Healthy Chinese Volunteers. Clin Drug Investig 44, 387–398 (2024). https://doi.org/10.1007/s40261-024-01362-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-024-01362-2