Abstract
Objective
To assess the cost effectiveness of the second COVID-19 booster vaccination with different age groups.
Methods
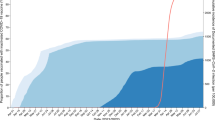
We developed a decision-analytic Susceptible-Exposed-Infected-Recovered (SEIR)-Markov model by five age groups (0–4 years, 5–11 years 12–17 years, 18–49 years, and 50+ years) and calibrated the model by actual mortality in each age group in the USA. We conducted five scenarios to evaluate the cost effectiveness of the second booster strategy and incremental benefits if the strategy would expand to 18–49 years and 12–17 years, from a health care system perspective. The analysis was reported according to the Consolidated Health Economic Evaluation Reporting Standards 2022 statement.
Results
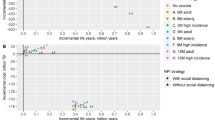
Implementing the second booster strategy for those aged ≥ 50 years cost $823 million but reduced direct medical costs by $1166 million, corresponding to a benefit-cost ratio of 1.42. Moreover, the strategy also resulted in a gain of 2596 quality-adjusted life-years (QALYs) during the 180-day evaluation period, indicating it was dominant. Further, vaccinating individuals aged 18–49 years with the second booster would result in an additional gain of $1592 million and 8790 QALYs. Similarly, expanding the vaccination to individuals aged 12–17 years would result in an additional gain of $16 million and 403 QALYs. However, if social interaction between all age groups was severed, vaccination expansion to ages 18–49 and 12–17 years would no longer be dominant but cost effective with an incremental cost-effectiveness ratio (ICER) of $37,572 and $26,705/QALY gained, respectively.
Conclusion
The second booster strategy was likely to be dominant in reducing the disease burden of the COVID-19 pandemic. Expanding the second booster strategy to ages 18–49 and 12–17 years would remain dominant due to their social contacts with the older age group.




Similar content being viewed by others
References
WHO. WHO coronavirus (COVID-19) dashboard. 2022. https://covid19.who.int/. Accessed 30 Aug 2023.
National Academies of Sciences E, Medicine, Health, et al. The National Academies Collection: Reports funded by National Institutes of Health. In: Kahn B, Brown L, Foege W, Gayle H, eds. Framework for Equitable Allocation of COVID-19 Vaccine. Washington (DC): National Academies Press (US).
Copyright 2020 by the National Academy of Sciences. All rights reserved. 2020.
Burgos RM, Badowski ME, Drwiega E, et al. The race to a COVID-19 vaccine: opportunities and challenges in development and distribution. Drugs Context. 2021;10.
Corey L, Mascola JR, Fauci AS, Collins FS. A strategic approach to COVID-19 vaccine R&D. Science. 2020;368(6494):948–50.
Bergwerk M, Gonen T, Lustig Y, et al. Covid-19 breakthrough infections in vaccinated health care workers. N Engl J Med. 2021;385(16):1474–84.
COVID-19 vaccine breakthrough infections reported to CDC—United States, January 1–April 30, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(21):792–3.
Karim SSA, Karim QA. Omicron SARS-CoV-2 variant: a new chapter in the COVID-19 pandemic. Lancet. 2021;398(10317):2126–8.
Burki T. Booster shots for COVID-19-the debate continues. Lancet Infect Dis. 2021;21(10):1359–60.
CDC. Trends in number of COVID-19 Vaccinations in the US. 2022. https://covid.cdc.gov/covid-data-tracker/#vaccination-trends. Accessed 30 Aug 2023.
Levine-Tiefenbrun M, Yelin I, Alapi H, et al. Waning of SARS-CoV-2 booster viral-load reduction effectiveness. Nat Commun. 2022;13(1):1237.
Arbel R, Sergienko R, Friger M, et al. Effectiveness of a second BNT162b2 booster vaccine against hospitalisation and death from COVID-19 in adults aged over 60 years. Nat Med. 2022;28(7):1486–90.
CDC. CDC Recommends Additional Boosters for Certain Individuals. 2022. https://www.cdc.gov/media/releases/2022/s0328-covid-19-boosters.html. Accessed 12 Aug 2022.
Di Fusco M, Shea KM, Lin J, et al. Health outcomes and economic burden of hospitalized COVID-19 patients in the United States. J Med Econ. 2021;24(1):308–17.
Christensen PA, Olsen RJ, Long SW, et al. Signals of significantly increased vaccine breakthrough, decreased hospitalisation rates, and less severe disease in patients with coronavirus disease 2019 caused by the omicron variant of severe acute respiratory syndrome coronavirus 2 in Houston, Texas. Am J Pathol. 2022;192(4):642–52.
Li R, Liu H, Fairley CK, et al. Cost-effectiveness analysis of BNT162b2 COVID-19 booster vaccination in the United States. Int J Infect Dis. 2022;119:87–94.
Husereau D, Drummond M, Augustovski F, et al. Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS 2022) statement: updated reporting guidance for health economic evaluations. Value Health. 2022;25(1):3–9.
Jit M, Brisson M. Modelling the epidemiology of infectious diseases for decision analysis: a primer. Pharmacoeconomics. 2011;29(5):371–86.
Bartsch SM, O’Shea KJ, Chin KL, et al. Maintaining face mask use before and after achieving different COVID-19 vaccination coverage levels: a modelling study. Lancet Public Health. 2022;7(4):e356–65.
Chemaitelly H, Ayoub HH, AlMukdad S, et al. Duration of mRNA vaccine protection against SARS-CoV-2 Omicron BA.1 and BA.2 subvariants in Qatar. Nat Commun. 2022;13(1):3082.
Kirsebom FCM, Andrews N, Stowe J, et al. COVID-19 vaccine effectiveness against the omicron (BA.2) variant in England. Lancet Infect Dis. 2022;22(7):931–3.
Patalon T, Saciuk Y, Peretz A, et al. Waning effectiveness of the third dose of the BNT162b2 mRNA COVID-19 vaccine. Nat Commun. 2022;13(1):3203.
Garrett N, Tapley A, Andriesen J, et al. High rate of asymptomatic carriage associated with variant strain omicron. medRxiv: the preprint server for health sciences 2022:2021.12.20.21268130.
Reddy KP, Shebl FM, Foote JHA, et al. Cost-effectiveness of public health strategies for COVID-19 epidemic control in South Africa: a microsimulation modelling study. Lancet Glob Health. 2021;9(2):e120–9.
IVAC. Results of COVID-19 vaccine effectiveness studies: an ongoing systematic review. 2022. https://view-hub.org/resources. Accessed 30 July 2022.
CDC. Provisional COVID-19 deaths by sex and age. 2022. https://data.cdc.gov/NCHS/Provisional-COVID-19-Deaths-by-Sex-and-Age/9bhg-hcku. Accessed 15 Nov 2022.
Treeage. Calibrate your model. 2022. https://www.treeage.com/learn-more/model-calibration/. Accessed 30 July 2022.
Sanders GD, Neumann PJ, Basu A, et al. Recommendations for conduct, methodological practices, and reporting of cost-effectiveness analyses: second panel on cost-effectiveness in health and medicine. JAMA. 2016;316(10):1093–103.
McDougall JA, Furnback WE, Wang BCM, Mahlich J. Understanding the global measurement of willingness to pay in health. J Mark Access Health Policy. 2020;8(1):1717030.
Neumann PJ, Cohen JT, Weinstein MC. Updating cost-effectiveness—the curious resilience of the $50,000-per-QALY threshold. N Engl J Med. 2014;371(9):796–7.
Link-Gelles R, Levy ME, Gaglani M, et al. Effectiveness of 2, 3, and 4 COVID-19 mRNA vaccine doses among immunocompetent adults during periods when SARS-CoV-2 omicron BA.1 and BA.2/BA.2.12.1 sublineages predominated—VISION network, 10 States, December 2021–June 2022. MMWR Morb Mortal Wkly Rep. 2022;71(29):931–9.
CDC. COVID-19 case surveillance public use data. 2022. https://data.cdc.gov/Case-Surveillance/COVID-19-Case-Surveillance-Public-Use-Data/vbim-akqf. Accessed 15 Nov 2022.
Acknowledgements
This study is supported by the World Health Organization (Grant number: 2022/1262416-0); LZ is supported by the Bill & Melinda Gates Foundation (Grant number: INV-006104); the National Natural Science Foundation of China (Grant number: 81950410639); Outstanding Young Scholars Support Program (Grant number: 3111500001); **’an Jiaotong University Basic Research and Profession Grant (Grant number: xtr022019003, xzy032020032); Epidemiology modelling and risk assessment (Grant number: 20200344) and **’an Jiaotong University Young Scholar Support Grant (Grant number: YX6J004). MS is supported by the National Key R&D Program of China (2022YFC2505100), the National Natural Science Foundation of China (12171387), China Post-doctoral Science Foundation (2018M631134 and 2020T130095ZX), and Young Talent Support Programme of Shaanxi University Association for Science and Technology (20210307).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval and consent to participate
Not applicable.
Consent for publication (from patients/participants)
Not applicable.
Data sharing
All data relevant to the study are included in the Article or in the online appendix.
Code availability
The TreeAge programme file used for the analysis described in this manuscript is available from the corresponding author upon reasonable request.
Author contributions
RL, LZ, MS and YL conceived the study. RL was involved in the study concept and design, data acquisition, data analysis, interpretation of data, and drafting of the manuscript. PL and QY were involved in the acquisition of data. CF, JP, WH and GZ were involved in the critical revision of the manuscript. LZ, YL and MS were involved in overall study supervision. RL, LZ, YL and MS had access to and verified the data. All authors participated in preparing the manuscript and have seen and approved the final version for submission.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, R., Lu, P., Fairley, C.K. et al. Cost-Effectiveness of the Second COVID-19 Booster Vaccination in the USA. Appl Health Econ Health Policy 22, 85–95 (2024). https://doi.org/10.1007/s40258-023-00844-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-023-00844-2