Abstract
Purpose of Review
The thoracic epidural has historically been regarded as the gold standard for the management of post-operative pain in patients undergoing major abdominal surgery. However, it is not without risk, and there are several circumstances in which it is contraindicated. The advent of ultrasound-guided fascial plane blocks has expanded our options in the provision of post-operative analgesia. This narrative review examines the evidence comparing their use against the thoracic epidural in major open abdominal surgery.
Recent Findings
The most common fascial plane blocks used in comparison to thoracic epidurals are rectus sheath blocks, transversus abdominis plane blocks, quadratus lumborum plane blocks, and erector spinae plane blocks. The current evidence demonstrates that these regional techniques can provide a viable alternative to thoracic epidurals for short-term post-operative outcomes and analgesia. However, there have been few studies looking at any long-term outcomes.
Summary
There is a growing number of alternative fascial plane blocks which can provide effective post-operative analgesia as an alternative to thoracic epidurals, especially when patients have contraindications for epidural insertion. Further research is warranted looking at the potential role regional anesthesia has on long-term outcomes for this group of surgical patients.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Nimmo SM, Foo ITH, Paterson HM. Enhanced recovery after surgery: Pain management. J Surg Oncol. 2017;116(5):583–91. https://doi.org/10.1002/jso.24814.
Gan TJ. Poorly controlled postoperative pain: Prevalence, consequences, and prevention. J Pain Res. 2017;10:2287–98. https://doi.org/10.2147/JPR.S144066.
Ludbrook GL. The hidden pandemic: the cost of postoperative complications. Curr Anesthesiol Rep. 2022;12(1):1–9. https://doi.org/10.1007/s40140-021-00493-y.
Benyamin R, Trescot AM, Datta S, Buenaventura R, Adlaka R, Sehgal N, et al. Opioid complications and side effects. Pain Physician. 2008;11(2 Suppl):S105–20. https://doi.org/10.36076/ppj.2008/11/s105.
Schwenk ES, Mariano ER. Designing the ideal perioperative pain management plan starts with multimodal analgesia. Korean J Anesthesiol. 2018;71(5):345–52. https://doi.org/10.4097/kja.d.18.00217.
Rawal N. Epidural technique for postoperative pain: Gold standard no more? Reg Anesth Pain Med. 2012;37(3):310–7. https://doi.org/10.1097/AAP.0b013e31825735c6.
Pirie K, Traer E, Finniss D, Myles PS, Riedel B. Current approaches to acute postoperative pain management after major abdominal surgery: a narrative review and future directions. Br J Anaesth. 2022;129(3):378–93. https://doi.org/10.1016/j.bja.2022.05.029.
Boezaart AP, Smith CR, Chembrovich S, Zasimovich Y, Server A, Morgan G, et al. Visceral versus somatic pain: An educational review of anatomy and clinical implications. Reg Anesth Pain Med. 2021;46(7):629–36. https://doi.org/10.1136/rapm-2020-102084.
Le-Wendling L, DeLoach J, Haller A, Ihnatsenka B. Analgesia for the trunk: A comparison of epidural, thoracic paravertebral and transversus abdominis plane blocks. pain and treatment. InTech. 2014. https://doi.org/10.5772/57403.
Koenen LR, Icenhour A, Forkmann K, Pasler A, Theysohn N, Forsting M, et al. Greater fear of visceral pain contributes to differences between visceral and somatic pain in healthy women. Pain. 2017;158(8):1599–608. https://doi.org/10.1097/j.pain.0000000000000924.
Elsenbruch S, Icenhour A, Enck P. Visceral pain - A biopsychological perspective. Neuroforum. 2017;23:105–10. https://doi.org/10.1515/nf-2017-A029.
Holte K, Kehlet H. Epidural anaesthesia and analgesia - Effects on surgical stress responses and implications for postoperative nutrition. Clinical Nutrition. 2002;21(3):199–206. https://doi.org/10.1054/clnu.2001.0514.
Pöp** DM, Elia N, Marret E, Remy C, Tramèr MR. Protective effects of epidural analgesia on pulmonary complications after abdominal and thoracic surgery: A meta-analysis. Archives of Surgery. 2008;143(10):990–9. https://doi.org/10.1001/archsurg.143.10.990.
Guay J, Kopp S. Epidural pain relief versus systemic opioid-based pain relief for abdominal aortic surgery. Cochrane Database Syst Rev. 2016;2016(1):CD005059. https://doi.org/10.1002/14651858.CD005059.pub4.
Guay J, Nishimori M, Kopp S. Epidural local anaesthetics versus opioid-based analgesic regimens for postoperative gastrointestinal paralysis, vomiting and pain after abdominal surgery. Cochrane Database of Syst Rev. 2016;7(7):CD001893. https://doi.org/10.1002/14651858.CD001893.pub2.
Groen JV, Khawar AAJ, Bauer PA, Bonsing BA, Martini CH, Mungroop TH, et al. Meta-analysis of epidural analgesia in patients undergoing pancreatoduodenectomy. BJS Open. 2019;3(5):559–71. https://doi.org/10.1002/bjs5.50171.
Akter N, Ratnayake B, Joh DB, Chan SJ, Bonner E, Pandanaboyana S. Postoperative Pain Relief after Pancreatic Resection: Systematic Review and Meta-Analysis of Analgesic Modalities. World J Surg. 2021;45(10):3165–73. https://doi.org/10.1007/s00268-021-06217-x.
Li YW, Li HJ, Li HJ, Zhao BJ, Guo XY, Feng Y, et al. Delirium in older patients after combined epidural-general anesthesia or general anesthesia for major surgery: A randomized trial. Anesthesiology. 2021;135(2):218–32. https://doi.org/10.1097/ALN.0000000000003834.
Chekol WB, Melesse DY, Denu ZA, Tawuye HY. Evidence-based thoracic epidural nerve block: A systematic review. Int J Surg Open. 2020;24:151–5. https://doi.org/10.1016/j.ijso.2020.05.004.
Ready LB. Acute pain: Lessons learned from 25,000 patients. Reg Anesth Pain Med. 1999;24(6):499–505. https://doi.org/10.1016/S1098-7339(99)90038-X.
Chauvin C, Klar G, Hopman WM, da Silva LM, Day AG, Phelan R, et al. Sensitivity and specificity of waveform analysis for assessing postoperative epidural function. J Clin Anesth. 2022;77:110630. https://doi.org/10.1016/j.jclinane.2021.110630.
Arnuntasupakul V, Van Zundert TCRV, Vijitpavan A, Aliste J, Engsusophon P, Leurcharusmee P, et al. A randomized comparison between conventional and waveform-confirmed loss of resistance for thoracic epidural blocks. Reg Anesth Pain Med. 2016;41(3):368–73. https://doi.org/10.1097/AAP.0000000000000369.
Tran DQH, González AP, Bernucci F, Finlayson RJ. Confirmation of loss-of-resistance for epidural analgesia. Reg Anesth Pain Med. 2015;40(2):166–73. https://doi.org/10.1097/AAP.0000000000000217.
Kwofie K, Tsui B. How I do it: epidural electrical stimulation (tsui test) for thoracic epidural catheter confirmation. ASRA News. 2021;46 https://doi.org/10.52211/asra050121.029.
Hermanides J, Hollmann MW, Stevens MF, Lirk P. Failed epidural: Causes and management. Br J Anaesth. 2012;109(2):144–54. https://doi.org/10.1093/bja/aes214.
Tran DQH, Van Zundert TCRV, Aliste J, Engsusophon P, Finlayson RJ. Primary failure of thoracic epidural analgesia in training centers: The invisible elephant? Reg Anesth Pain Med. 2016;41(3):309–13. https://doi.org/10.1097/AAP.0000000000000394.
Hogan QH. Epidural anatomy: New observations. Can J Anaesth. 1998;45(5 pt 2):R40–8. https://doi.org/10.1007/bf03019206.
Rigg JRA, Jamrozik K, Myles PS, Silbert BS, Peyton PJ, Parsons RW, et al. Epidural anaesthesia and analgesia and outcome of major surgery: A randomised trial. Lancet. 2002;359(9314):1276–82. https://doi.org/10.1016/S0140-6736(02)08266-1.
Huang Y, Li T, Wang T, Wei Y, **ong L, Wang T, et al. Real time ultrasound-guided thoracic epidural catheterization with patients in the lateral decubitus position without flexion of knees and neck: a preliminary investigation. J Clin Med. 2022;11(21):6459. https://doi.org/10.3390/jcm11216459.
Pakpirom J, Thatsanapornsathit K, Kovitwanawong N, Petsakul S, Benjhawaleemas P, Narunart K, et al. Real-time ultrasound-guided versus anatomic landmark-based thoracic epidural placement: a prospective, randomized, superiority trial. BMC Anesthesiol. 2022;22(1):198. https://doi.org/10.1186/s12871-022-01730-5.
Horlocker TT, Vandermeuelen E, Kopp SL, Gogarten W, Leffert LR, Benzon HT. Regional anesthesia in the patient receiving antithrombotic or thrombolytic therapy. Reg Anesth Pain Med. 2018;43(3):263–309. https://doi.org/10.1097/aap.0000000000000763.
Grewal S, Hocking G, Wildsmith JAW. Epidural abscesses. Br J Anaesth. 2006;96(3):292–302. https://doi.org/10.1093/bja/ael006.
Giebler RM, Scherer RU, Peters J, Rich GF. Incidence of neurologic complications related to thoracic epidural catheterization. Surv Anesthesiol. 1997;86(1):55–63. https://doi.org/10.1097/00132586-199710000-00049.
Manassero A, Bossolasco M, Carrega M, Coletta G. Postoperative thoracic epidural analgesia: Adverse events from a single-center series of 3126 patients. Local Reg Anesth. 2020;13:111–9. https://doi.org/10.2147/LRA.S272410.
Webb CA, Weyker PD, Zhang L, Stanley S, Coyle DT, Tang T, et al. Unintentional dural puncture with a tuohy needle increases risk of chronic headache. Obstetric Anesthesia Digest. 2013;33(2):91–2. https://doi.org/10.1097/01.aoa.0000429123.55800.ac.
Clemente A, Carli F. The physiological effects of thoracic epidural anesthesia and analgesia on the cardiovascular, respiratory and gastrointestinal systems. Minerva Anestesiol. 2008;74(10):549–63.
Beattie WS, Badner NH, Choi P. Epidural analgesia reduces postoperative myocardial infarction: A meta-analysis. Anesth Analg. 2001;93(4):853–8. https://doi.org/10.1097/00000539-200110000-00010.
Klotz R, Larmann J, Klose C, Bruckner T, Benner L, Doerr-Harim C, et al. Gastrointestinal complications after pancreatoduodenectomy with epidural vs patient-controlled intravenous analgesia: a randomized clinical trial. JAMA Surg. 2020;155(7):e200794. https://doi.org/10.1001/jamasurg.2020.0794.
Wright GP, Koehler TJ, Davis AT, Chung MH. The drowning whipple: Perioperative fluid balance and outcomes following pancreaticoduodenectomy. J Surg Oncol. 2014;110(4):407–11. https://doi.org/10.1002/jso.23662.
Tsui BCH, Cheung SSK, Ziwenga O, Gragasin FS. Use of Intralipid® in managing refractory hypotension following epidural blockade. Can J Anesth. 2014;62(5):548–9. https://doi.org/10.1007/s12630-014-0279-6.
Ladak SSJ, Katznelson R, Muscat M, Sawhney M, Beattie WS, O’Leary G. Incidence of Urinary Retention in Patients with Thoracic Patient-Controlled Epidural Analgesia (TPCEA) Undergoing Thoracotomy. Pain Manag Nurs. 2009;10(2):94–8. https://doi.org/10.1016/j.pmn.2008.08.001.
El-Boghdadly K, Wolmarans M, Stengel AD, Albrecht E, Chin KJ, Elsharkawy H, et al. Standardizing nomenclature in regional anesthesia: An ASRA-ESRA Delphi consensus study of abdominal wall, paraspinal, and chest wall blocks. Reg Anesth Pain Med. 2021;46(7):571–80. https://doi.org/10.1136/rapm-2020-102451.
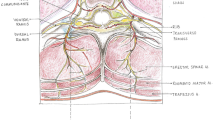
Chin KJ, McDonnell JG, Carvalho B, Sharkey A, Pawa A, Gadsden J. Essentials of our current understanding: Abdominal wall blocks. Reg Anesth Pain Med. 2017;42(2):133–83. https://doi.org/10.1097/AAP.0000000000000545.
Dutton TJ, McGrath JS, Daugherty MO. Use of rectus sheath catheters for pain relief in patients undergoing major pelvic urological surgery. BJU Int. 2014;113(2):246–53. https://doi.org/10.1111/bju.12316.
Barrington MJ, Ivanusic JJ, Rozen WM, Hebbard P. Spread of injectate after ultrasound-guided subcostal transversus abdominis plane block: A cadaveric study. Anaesthesia. 2009;64(7):745–50. https://doi.org/10.1111/j.1365-2044.2009.05933.x.
Rucklidge M, Beattie E. Rectus sheath catheter analgesia for patients undergoing laparotomy. BJA Educ. 2018;18(6):166–72. https://doi.org/10.1016/j.bjae.2018.03.002.
Bungart B, Joudeh L, Fettiplace M. Local anesthetic dosing and toxicity of adult truncal catheters: a narrative review of published practice. Reg Anesth Pain Med. 2023;14:rapm-2023-104667. https://doi.org/10.1136/rapm-2023-104667.
Jankovic Z, Ahmad N, Ravishankar N, Archer F. Transversus abdominis plane block: How safe is it? Anesth Analg. 2008;107(5):1758–9. https://doi.org/10.1213/ane.0b013e3181853619.
Kwon HJ, Kim YJ, Kim Y, Kim S, Cho H, Lee JH, et al. Complications and technical consideration of ultrasound-guided rectus sheath blocks: a retrospective analysis of 4033 patients. Anesth Analg. 2023;136(2):365–72. https://doi.org/10.1213/ANE.0000000000006282.
Walker G. Transversus abdominis plane block: A note of caution! Br J Anaesth. 2010;104(2):265. https://doi.org/10.1093/bja/aep387.
Wikner M. Unexpected motor weakness following quadratus lumborum block for gynaecological laparoscopy. Anaesthesia. 2017;72(2):230–2. https://doi.org/10.1111/anae.13754.
Johnson TR, Rees SGO, Glancy DG. Rectus sheath catheter entrapment. Anaesthesia. 2016;71(5):602–3. https://doi.org/10.1111/anae.13469.
Maury T, Elnar A, Marchionni S, Frisoni R, Goetz C, Bécret A. Effect of rectus sheath anaesthesia versus thoracic epidural analgesia on postoperative recovery quality after elective open abdominal surgery in a French regional hospital: The study protocol of a randomised controlled QoR-RECT-CATH trial. BMJ Open. 2023;13(5):e069736. https://doi.org/10.1136/bmjopen-2022-069736.
Godden AR, Marshall MJ, Grice AS, Daniels IR. Ultrasonography guided rectus sheath catheters versus epidural analgesia for open colorectal cancer surgery in a single centre. Ann R Coll Surg Engl. 2013;95(8):591–4. https://doi.org/10.1308/rcsann.2013.95.8.591.
Tudor ECG, Yang W, Brown R, Mackey PM. Rectus sheath catheters provide equivalent analgesia to epidurals following laparotomy for colorectal surgery. Ann R Coll Surg Engl. 2015;97(7):530–3. https://doi.org/10.1308/rcsann.2015.0018.
Yassin HM, Abd Elmoneim AT, El Moutaz H. The analgesic efficiency of ultrasound-guided rectus sheath analgesia compared with low thoracic epidural analgesia after elective abdominal surgery with a midline incision: A prospective randomized controlled trial. Anesth Pain Med. 2017;7(3):e14244. https://doi.org/10.5812/aapm.14244.
Eltwab M, Tueki DA, Rahman Ibrahim IA, Elzohry AAM. Peri-operative rectus sheath fentanyl-Levobupivacaine infusion vs. thoracic epidural fentanyl levobupvacaine infusion in patients undergoing major abdominal cancer surgeries with Medline Incision. J Pain Relief. 2018;7(3):318. https://doi.org/10.4172/2167-0846.1000318.
Gupta N, Kumar A, Harish RK, Jain D, Swami AC. Comparison of postoperative analgesia and opioid requirement with thoracic epidural vs. continuous rectus sheath infusion in midline incision laparotomies under general anaesthesia - A prospective randomised controlled study. Indian J Anaesth. 2020;64(9):750–5. https://doi.org/10.4103/ija.IJA_976_19.
Kuniyoshi H, Yamamoto Y, Kimura S, Hiroe T, Terui T, Kase Y. Comparison of the analgesic effects continuous epidural anesthesia and continuous rectus sheath block in patients undergoing gynecological cancer surgery: a non-inferiority randomized control trial. J Anesth. 2021;35(5):663–70. https://doi.org/10.1007/s00540-021-02973-1.
Krige A, Brearley SG, Mateus C, Carlson GL, Lane S. A comparison between thoracic epidural analgesia and rectus sheath catheter analgesia after open midline major abdominal surgery: Randomized clinical trial. BJS Open. 2022;6(3):zrac055. https://doi.org/10.1093/bjsopen/zrac055.
Niraj G, Kelkar A, Jeyapalan I, Graff-Baker P, Williams O, Darbar A, et al. Comparison of analgesic efficacy of subcostal transversus abdominis plane blocks with epidural analgesia following upper abdominal surgery. Anaesthesia. 2011;66(6):465–71. https://doi.org/10.1111/j.1365-2044.2011.06700.x.
Kadam VR, Van Wijk RM, Moran JL, Miller D. Epidural versus continuous transversus abdominis plane catheter technique for postoperative analgesia after abdominal surgery. Anaesth Intensive Care. 2013;41(4):476–81. https://doi.org/10.1177/0310057x1304100407.
Wu Y, Liu F, Tang H, Wang Q, Chen L, Wu H, et al. The analgesic efficacy of subcostal transversus abdominis plane block compared with thoracic epidural analgesia and intravenous opioid analgesia after radical gastrectomy. Anesth Analg. 2013;117(2):507–13. https://doi.org/10.1213/ANE.0b013e318297fcee.
Wahba SS, Kamal SM. Analgesic efficacy and outcome of transversus-abdominis plane block versus low thoracic-epidural analgesia after laparotomy in ischemic heart disease patients. J Anesth. 2014;28(4):517–23. https://doi.org/10.1007/s00540-013-1774-6.
Kandi Y. Efficacy of ultrasound-guided transversus abdominis plane block versus epidural analgesia in pain management following lower abdominal surgery. Ain-Shams J Anaesthesiol. 2015;8(4):653–7. https://doi.org/10.4103/1687-7934.172762.
Ganapathy S, Sondekoppam RV, Terlecki M, Brookes J, Das AS, Subramanian L. Comparison of efficacy and safety of lateral-to-medial continuous transversus abdominis plane block with thoracic epidural analgesia in patients undergoing abdominal surgery: A randomised, open-label feasibility study. Eur J Anaesthesiol. 2015;32(11):797–804. https://doi.org/10.1097/EJA.0000000000000345.
Raghvendra K, Thapa D, Mitra S, Ahuja V, Gombar S, Huria A. Postoperative pain relief following hysterectomy: A randomized controlled trial. J Midlife Health. 2016;7(2):65–8. https://doi.org/10.4103/0976-7800.185327.
Shaker TM, Carroll JT, Chung MH, Koehler TJ, Lane BR, Wolf AM, et al. Efficacy and safety of transversus abdominis plane blocks versus thoracic epidural anesthesia in patients undergoing major abdominal oncologic resections: A prospective, randomized controlled trial. Am J Surg. 2018;215(3):498–501. https://doi.org/10.1016/j.amjsurg.2017.10.055.
Mathew P, Aggarwal N, Kumari K, Gupta A, Panda N, Bagga R. Quality of recovery and analgesia after total abdominal hysterectomy under general anesthesia: A randomized controlled trial of TAP block vs epidural analgesia vs parenteral medications. J Anaesthesiol Clin Pharmacol. 2019;35(2):170–5. https://doi.org/10.4103/joacp.JOACP_206_18.
Cata JP, Fournier K, Corrales G, Owusu-Agyemang P, Soliz J, Bravo M, et al. The Impact of thoracic epidural analgesia versus four quadrant transversus abdominis plane block on quality of recovery after cytoreductive surgery with hyperthermic intraperitoneal chemotherapy surgery: a single-center, noninferiority, randomized. Controlled Trial. Ann Surg Oncol. 2021;28(9):5297–310. https://doi.org/10.1245/s10434-021-09622-7.
Trujillo CN, Ogutcu H, GnanaDev R, Johna S, Al-Temimi MH. Regional abdominal wall nerve block versus epidural anesthesia after hepatectomy: analysis of the ACS NSQIP database. Surg Endosc. 2022;36(10):7259–65. https://doi.org/10.1007/s00464-022-09109-w.
Zubair M, Adil Khan M, Khan MNA, Iqbal S, Ashraf M, Saleem SA. Comparison of continuous thoracic epidural with erector spinae block for postoperative analgesia in adult living donor hepatectomy. Cureus. 2022;14(3):e23151. https://doi.org/10.7759/cureus.23151.
Greenbaum A, Wilcox H, Teng CH, Petersen T, Billstrand M, Campbell R, et al. Use of erector spinae fascial plane blocks in enhanced recovery for open abdominal surgery. J Surg Res. 2021;268:673–80. https://doi.org/10.1016/j.jss.2021.08.008.
Korgvee A, Veskimae E, Huhtala H, Koskinen H, Tammela T, Junttila E, et al. Posterior quadratus lumborum block versus epidural analgesia for postoperative pain management after open radical cystectomy: A randomized clinical trial. Acta Anaesthesiol Scand. 2023;67(3):347–55. https://doi.org/10.1111/aas.14188.
Gu B, Zhou H, Lian Y, Zhou Y, He S, **e K, et al. Ultrasound-guided anterior quadratus lumborum block at lateral supra-arcuate ligament vs thoracic epidural analgesia after open liver surgery: A randomized, controlled, noninferiority trial. J Am Coll Surg. 2022;235(6):871–8. https://doi.org/10.1097/XCS.0000000000000354.
Elsharkawy H, Ahuja S, Sessler DI, Maheshwari K, Mao G, Esa WAS, et al. Subcostal anterior quadratus lumborum block versus epidural block for analgesia in open nephrectomy: A randomized clinical trial. Anesth Analg. 2021;132(4):1138–45. https://doi.org/10.1213/ANE.0000000000005382.
Furuya T, Kato J, Yamamoto Y, Hirose N, Suzuki T. Comparison of dermatomal sensory block following ultrasound-guided transversus abdominis plane block by the lateral and posterior approaches: A randomized controlled trial. J Anaesthesiol Clin Pharmacol. 2018;34(2):205–10. https://doi.org/10.4103/joacp.JOACP_295_15.
Abdildin Y, Tapinova K, Nugumanova M, Viderman D. Transversus abdominis plane block in adult open liver surgery patients: A systematic review with meta-analysis of randomized controlled trials. J Visc Surg. 2023;160(4):253–60. https://doi.org/10.1016/j.jviscsurg.2022.11.003.
Hong S, Kim H, Park J. Analgesic effectiveness of rectus sheath block during open gastrectomy: A prospective double-blinded randomized controlled clinical trial. Medicine. 2019;98(15):e15159. https://doi.org/10.1097/MD.0000000000015159.
Zayed M, Allers K, Hoffmann F, Bantel C. Transversus abdominis plane block in urological procedures: A systematic review and meta-Analysis. Eur J Anaesthesiol. 2021;38(7):758–67. https://doi.org/10.1097/EJA.0000000000001453.
Sharma A, Goel AD, Sharma PP, Vyas V, Agrawal SP. The effect of transversus abdominis plane block for analgesia in patients undergoing liver transplantation: A systematic review and meta-analysis. Turk J Anaesthesiol Reanim. 2019;47(5):359–66. https://doi.org/10.5152/TJAR.2019.60251.
Penuela L, DBrass TJ, Tubog TD. Use of transversus abdominis plane block in hysterectomy: a systematic review. J Perianesth Nurs. 2023;38(2):331–8. https://doi.org/10.1016/j.jopan.2022.06.017.
Viderman D, Aubakirova M, Abdildin YG. Transversus abdominis plane block in colorectal surgery: A meta-analysis. Front Med (Lausanne). 2022;8:802039. https://doi.org/10.3389/fmed.2021.802039.
Osborn S, Cyna AM, Middleton P, Griffiths JD. Perioperative transversus abdominis plane (TAP) blocks for analgesia after abdominal surgery. Cochrane Database of Syst Rev. 2020;4(4):CD007705. https://doi.org/10.1002/14651858.CD007705.pub3.
Ismail S, Ahmed A, Hoda MQ, Asghar S, Habib A, Aziz A. Mid-Axillary transversus abdominis plane block and stress response after abdominal hysterectomy: A randomised controlled placebo trial. Eur J Anaesthesiol. 2021;38(7):768–76. https://doi.org/10.1097/EJA.0000000000001413.
Liu R, Qin H, Wang M, Li K, Zhao G. Transversus abdominis plane block with general anesthesia blunts the perioperative stress response in patients undergoing radical gastrectomy. BMC Anesthesiol. 2019;19(1):205. https://doi.org/10.1186/s12871-019-0861-0.
Dieu A, Huynen P, Lavand’homme P, Beloeil H, Freys SM, Pogatzki-Zahn EM, et al. Pain management after open liver resection: Procedure-Specific Postoperative Pain Management (PROSPECT) recommendations. Reg Anesth Pain Med. 2021;46(5):433–45. https://doi.org/10.1136/rapm-2020-101933.
Bayramov N, Mammadova S. A review of the current ERAS guidelines for liver resection, liver transplantation and pancreatoduodenectomy. Annals of Medicine and Surgery. 2022;82:104596. https://doi.org/10.1016/j.amsu.2022.104596.
Blanco R. 271: Tap block under ultrasound guidance: the description of a “no pops” technique. Reg Anesth Pain Med. 2007;32(5):130. https://doi.org/10.1016/j.rapm.2007.06.268.
Balocco AL, López AM, Kesteloot C, Horn JL, Brichant JF, Vandepitte C, et al. Quadratus lumborum block: An imaging study of three approaches. Reg Anesth Pain Med. 2021;46(1):35–40. https://doi.org/10.1136/rapm-2020-101554.
Mao Y, Zhao W, Hao M, **ng R, Yan M. Ultrasound-guided quadratus lumborum block at the lateral supra-arcuate ligament versus subcostal transversus abdominis plane block for postoperative analgesia following open hepatectomy: A randomized controlled trial. J Pain Res. 2023;16:1429–40. https://doi.org/10.2147/JPR.S404810.
Naaz S, Kumar R, Ozair E, Sahay N, Asghar A, Jha S, et al. Ultrasound guided quadratus lumborum block versus transversus abdominis plane block for post-operative analgesia in patients undergoing total abdominal hysterectomy. Turk J Anaesthesiol Reanim. 2021;49(5):357–64. https://doi.org/10.5152/TJAR.2021.985.
Kolacz M, Mieszkowski M, Janiak M, Zagorski K, Byszewska B, Weryk-Dysko M, et al. Transversus abdominis plane block versus quadratus lumborum block type 2 for analgesia in renal transplantation: A randomised trial. Eur J Anaesthesiol. 2020;37(9):773–89. https://doi.org/10.1097/EJA.0000000000001193.
Yousef N. Quadratus lumborum block versus transversus abdominis plane block in patients undergoing total abdominal hysterectomy: A randomized prospective controlled trial. Anesth Essays Res. 2018;12(3):742–7. https://doi.org/10.4103/aer.aer_108_18.
Lonnqvist PA, Karmakar MK, Richardson J, Moriggl B. Daring discourse: Should the ESP block be renamed RIP II block? Reg Anesth Pain Med. 2021;46(1):57–60. https://doi.org/10.1136/rapm-2020-101822.
Pawa A, King C, Thang C, White L. Erector spinae plane block: the ultimate ‘plan A’ block? Br J Anaesth. 2023;130(5):497–502. https://doi.org/10.1016/j.bja.2023.01.012.
Zhou L, Wang S, Liu C, Yan T, Song Y, Shu S, et al. The efficiency of ultrasound-guided erector spinae plane block in early cervical cancer patients undergoing laparotomic radical hysterectomy: A double-blind randomized controlled trial. Front Surg. 2023;9:1039629. https://doi.org/10.3389/fsurg.2022.1039629.
Shukla U, Yadav U, Singh AK, Tyagi A. Randomized comparative study between bilateral erector spinae plane block and transversus abdominis plane block under ultrasound guidance for postoperative analgesia after total abdominal hysterectomy. Cureus. 2022;14(5):e25227. https://doi.org/10.7759/cureus.25227.
Kamel AAF, Amin OAI, Ibrahem MAM. Bilateral ultrasound-guided erector spinae plane block versus transversus abdominis plane block on postoperative analgesia after total abdominal hysterectomy. Pain Physician. 2020;23(4):375–82. https://doi.org/10.36076/ppj.2020/23/375.
Onay M, Kayhan GE, Özen A, Baş SŞ, Yelken B. Comparison of ultrasound-guided quadratus lumborum block and erector spinae plane block in terms of their effects on postoperative pain in open nephrectomy. Minerva Anestesiol. 2023;89(1-2):32–9. https://doi.org/10.23736/S0375-9393.22.16635-6.
Wijeysundera DN, Beattie WS, Austin PC, Hux JE, Laupacis A. Epidural anaesthesia and survival after intermediate-to-high risk non-cardiac surgery: a population-based cohort study. The Lancet. 2008;372(9638):562–9. https://doi.org/10.1016/S0140-6736(08)61121-6.
Pöp** DM, Elia N, Van Aken HK, Marret E, Schug SA, Kranke P, et al. Impact of epidural analgesia on mortality and morbidity after surgery. Ann Surg. 2014;259(6):1056–67. https://doi.org/10.1097/sla.0000000000000237.
Moormann S, Rüebsam ML, Warnking E, Gottschalk A, Hahnenkamp K, Van Aken H, et al. Beneficial effects of thoracic epidural anesthesia on mortality rate in geriatric patients after elective surgery for colon cancer: A study of 215 consecutive patients. Anesth Crit Care. 2022;4(2):104–17. https://doi.org/10.26502/acc.044.
Bardia A, Sood A, Mahmood F, Orhurhu V, Mueller A, Montealegre-Gallegos M, et al. Combined epidural-general anesthesia vs general anesthesia alone for elective abdominal aortic aneurysm repair. JAMA Surg. 2016;151(12):1116–23. https://doi.org/10.1001/jamasurg.2016.2733.
Grandhi RK, Lee S, Abd-Elsayed A. Does opioid use cause angiogenesis and metastasis? Pain Med. 2017;18(1):140–51. https://doi.org/10.1093/pm/pnw132.
Onuma AE, Zhang H, Gil L, Huang H, Tsung A. Surgical stress promotes tumor progression: A focus on the impact of the immune response. J Clin Med. 2020;9(12):4096. https://doi.org/10.3390/jcm9124096.
Chen Z, Zhang P, Xu Y, Yan J, Liu Z, Lau WB, et al. Surgical stress and cancer progression: The twisted tango. Mol Cancer. 2019;18(1):132. https://doi.org/10.1186/s12943-019-1058-3.
Dockrell L, Buggy DJ. The role of regional anaesthesia in the emerging subspecialty of onco-anaesthesia: a state-of-the-art review. Anaesthesia. 2021;76(Suppl 1):148–59. https://doi.org/10.1111/anae.15243.
• Li T, Meng X, Wang D, Wang Q, Ma J, Dai Z. Regional anesthesia did not improve postoperative long-term survival of tumor patients: a systematic review and meta-analysis of randomized controlled trials. World J Surg Oncol. 2023;21(1):68. https://doi.org/10.1186/s12957-023-02957-3. No role for regional anesthesia in improving long-term survival following oncological surgery.
Rosenberger DC, Pogatzki-Zahn EM. Chronic post-surgical pain – update on incidence, risk factors and preventive treatment options. BJA Educ. 2022;22(5):190–6. https://doi.org/10.1016/j.bjae.2021.11.008.
Ayoo K, Mikhaeil JS, Huang A, Wąsowicz M. The opioid crisis in North America: Facts and future lessons for Europe. Anaesthesiol Intensive Ther. 2020;52(2):139–47. https://doi.org/10.5114/AIT.2020.94756.
Clarke H, Soneji N, Ko DT, Yun L, Wijeysundera DN. Rates and risk factors for prolonged opioid use after major surgery: Population based cohort study. BMJ (Online). 2014;348:g1251. https://doi.org/10.1136/bmj.g1251.
Chen YYK, Boden KA, Schreiber KL. The role of regional anaesthesia and multimodal analgesia in the prevention of chronic postoperative pain: a narrative review. Anaesthesia. 2021;76(Suppl 1):8–17. https://doi.org/10.1111/anae.15256.
Weinstein EJ, Levene JL, Cohen MS, Andreae DA, Chao JY, Johnson M, et al. Local anaesthetics and regional anaesthesia versus conventional analgesia for preventing persistent postoperative pain in adults and children. Cochrane Database Syst Rev. 2018;(6):CD007105. https://doi.org/10.1002/14651858.cd007105.pub4.
Lavand’homme P, De Kock M. The use of intraoperative epidural or spinal analgesia modulates postoperative hyperalgesia and reduces residual pain after major abdominal surgery. Acta Anaesthesiol Belg. 2006;57(4):373–9.
Bouman EA, Theunissen M, Bons SA, van Mook WN, Gramke HF, van Kleef M, et al. Reduced incidence of chronic postsurgical pain after epidural analgesia for abdominal surgery. Pain Practice. 2014;14(2):E76–84. https://doi.org/10.1111/papr.12091.
Lavand’homme P, De Kock M, Waterloos H. Intraoperative epidural analgesia combined with ketamine provides effective preventive analgesia in patients undergoing major digestive surgery. Anesthesiology. 2005;103(4):813–20. https://doi.org/10.1097/00000542-200510000-00020.
Ladha KS, Patorno E, Liu J, Bateman BT. Impact of perioperative epidural placement on postdischarge opioid use in patients undergoing abdominal surgery. Anesthesiology. 2016;124(2):396–403. https://doi.org/10.1097/ALN.0000000000000952.
Katz J, Cohen L. Preventive analgesia is associated with reduced pain disability 3 weeks but not 6 months after major gynecologic surgery by laparotomy. Anesthesiology. 2004;101(1):169–74. https://doi.org/10.1097/00000542-200407000-00026.
Royse C, Remedios C, Royse A. High thoracic epidural analgesia reduces the risk of long-term depression in patients undergoing coronary artery bypass surgery. Ann Thorac Cardiovasc Surg. 2007;13(1):32–5.
Pagé MG, Kudrina I, Zomahoun HTV, Croteau J, Ziegler D, Ngangue P, et al. A systematic review of the relative frequency and risk factors for prolonged opioid prescription following surgery and trauma among adults. Ann Surg. 2020;271(5):845–54. https://doi.org/10.1097/SLA.0000000000003403.
Pan ZY, Hu ZH, Zhang F, **e WX, Tang YZ, Liao Q. The effect of transversus abdominis plane block on the chronic pain after colorectal surgery: A retrospective cohort study. BMC Anesthesiol. 2020;20(1):116. https://doi.org/10.1186/s12871-020-01032-8.
Liu QR, **e J, Dai YC, Ji MH, Zhou CM, Gu HW, et al. Quadratus lumborum block spares postoperative opioid usage but does not appear to prevent the development of chronic pain after gastrointestinal surgery. Pain Physician. 2021;24(8):E1191–8.
Liu QR, Dai YC, **e J, Li X, Sun XB, Sun J. Ultrasound-guided quadratus lumborum block enhances the quality of recovery after gastrointestinal surgery: a randomized controlled trial. Pain Res Manag. 2022;2022:8994297. https://doi.org/10.1155/2022/8994297.
Sellam S, Nguyen AT, Pogu M, Kianmanesh R, Malinovsky JM, Renard Y. Transversus abdominis plane block in the treatment of chronic postsurgical abdominal wall pain improves patient quality of life: A retrospective study and literature review. Pain Physician. 2023;26(2):E91–E100.
Elsharydah A, De La Cruz R, Horani SM, **ao CY. Utilization of truncal fascial plane nerve blocks for chronic pain management: A narrative review. Curr Pain Headache Rep. 2023;27(6):149–55. https://doi.org/10.1007/s11916-023-01112-7.
Felling DR, Jackson MW, Ferraro J, Battaglia MA, Albright JJ, Wu J, et al. Liposomal bupivacaine transversus abdominis plane block versus epidural analgesia in a colon and rectal surgery enhanced recovery pathway: A randomized clinical trial. Dis Colon Rectum. 2018;61(10):1196–204. https://doi.org/10.1097/DCR.0000000000001211.
Holtz M, Liao N, Lin JH, Asche CV. Economic outcomes and incidence of postsurgical hypotension with liposomal bupivacaine vs epidural analgesia in abdominal surgeries. J Health Econ Outcomes Res. 2019;9(2):86–94. https://doi.org/10.36469/jheor.2022.37739.
Elsharkawy H, Kolli S, Soliman LM, Seif J, Drake RL, Mariano ER, et al. The external oblique intercostal block: anatomic evaluation and case series. Pain Med (United States). 2021;22(11):2436–42. https://doi.org/10.1093/pm/pnab296.
• Barry G, Sehmbi H, Retter S, Bailey JG, Tablante R, Uppal V. Comparative efficacy and safety of non-neuraxial analgesic techniques for midline laparotomy: a systematic review and frequentist network meta-analysis of randomised controlled trials. Br J Anaesth. 2023;131(6):1053–71. https://doi.org/10.1016/j.bja.2023.08.024. Systematic review and network meta-analysis suggesting continuous RS and TAP blocks are the most efficacious fascial plane techniques for managing post-operative pain in patients undergoing midline laparotomy.
• Howle R, Ng SC, Wong HY, Onwochei D, Desai N. Comparison of analgesic modalities for patients undergoing midline laparotomy: a systematic review and network meta-analysis. Can J Anesth. 2022;69(1):140–76. https://doi.org/10.1007/s12630-021-02128-6. Systematic review and network meta-analysis concluding TEA provide clinically superior analgesia compared with continuous regional techniques for the first 24 h post-operatively following midline laparotomy.
• Bailey JG, Morgan CW, Christie R, Ke JXC, Kwesi Kwofie M, Uppal V. Continuous peripheral nerve blocks compared to thoracic epidurals or multimodal analgesia for midline laparotomy: A systematic review and meta-analysis. Korean J Anesthesiol. 2021;74(5):394–408. https://doi.org/10.4097/KJA.20304. Systematic review and meta-analysis find no statistically significant difference between TEA and continuous nerve blocks in the management of post-operative pain following midline laparotomy.
Author information
Authors and Affiliations
Contributions
A.C. first author. F.W. second author. A.P. Senior author. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
Amit Pawa has received honoraria from GE healthcare and consults for Pacira Pharmaceutical.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Carver, A., Wou, F. & Pawa, A. Do Outcomes Differ Between Thoracic Epidurals and Continuous Fascial Plane Blocks in Adults Undergoing Major Abdominal Surgery?. Curr Anesthesiol Rep 14, 25–41 (2024). https://doi.org/10.1007/s40140-023-00594-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40140-023-00594-w