Abstract
Purpose
The 2009 worldwide influenza A/H1N1 pandemic particularly affected younger people, including schoolchildren. We assessed the effects of class/school closure during the pandemic on the spread of H1N1 infection in Japan.
Methods
We prospectively monitored 2,141 schoolchildren in 57 classes at two elementary schools and two junior high schools in Japan, and evaluated the effects of class/school closures on the spread of H1N1 using descriptive epidemiological methods.
Results
The cumulative rate of H1N1 infection among these children was 40.9 % (876 children). There was a total of 53 closures of 40 classes, including school closures, during the pandemic. Time-course changes in the epidemic curve showed that school closure reduced the following epidemic peak more than class closure. A Poisson regression model showed that a longer duration of closure was significantly related to decreased H1N1 occurrence after the resumption of classes.
Conclusions
School closure more effectively inhibits subsequent epidemic outbreaks than class closure. Longer school closures are effective in reducing the spread of infection, and school closure should be implemented as early as possible.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The influenza A/H1N1 (H1N1) pandemic first broke out in several countries in April 2009 [1]. The first infection case in Japan was reported at the quarantine facility of Narita Airport in early May 2009, and the epidemic spread to the urban areas of western Japan in the middle of May 2009. Governmental infection control measures were implemented over a broad urban area, and the epidemic ended by the end of May. The H1N1 epidemic resumed in various areas of Japan from August to September, and the epidemic spread to Nagano Prefecture, where this study was performed. The pandemic affected almost 15 million people between May 2009 and March 2010, with 200 deaths ascribed to this disease in Japan [2].
At the end of the pandemic, it became clear that H1N1 had spread more among younger people than older people [3–8], and there were many infections among schoolchildren [9–11]. Measures instituted to prevent the transmission of H1N1 included school closures [12–15]. The effects of school closures were evaluated in simulation models [14–16] and some reports have shown the effects of actual closures [17, 18]. However, there have been few reports indicating the optimal length and timing of closure for effective control of infection spread [19], and comprehensive effects of these closures remain unclear. Therefore, further study is required to clarify these issues.
Four schools affiliated with Shinshu University in Japan experienced the H1N1 pandemic and implemented short-term class/school closures in 2009 and 2010. Although we have reported an overview of the pandemic in these schools and the possible effects of these closures [7], we have not described the effects of these closures in detail or analyzed the effects of these closures on the spread of H1N1. In this study, we, therefore, determined how these closures inhibited the spread of H1N1 using descriptive epidemiological methods.
Methods
Subjects
The study subjects included students at four schools, two elementary schools and two junior high schools, affiliated with Shinshu University in Nagano Prefecture, Japan. These schools are located in two districts, each containing one elementary school and one junior high school, that are 70 km apart. Education of children at this age is compulsory, and each class unit contains 35–40 children. Students attending the elementary schools are 7–12 years old and those attending the junior high school are 13–15 years old. In district A, there were 422 children in 12 classes at the elementary school and 464 children in 12 classes at the junior high school. In district B, there were 598 children in 16 classes at the elementary school and 657 children in 17 classes at the junior high school. We prospectively monitored the total number of 2,141 schoolchildren attending 57 classes during the H1N1 pandemic from August 2009 to March 2010. Staff members, including teachers and administrators, were excluded from this investigation because this study focused only on schoolchildren.
Precautions and records
All children attending the four schools were encouraged, verbally and in writing, to be aware of personal hygiene and to take precautions, including washing their hands, gargling, and wearing masks [7]. These precautions were initially implemented in September 2009, when school resumed after the summer recess. Moreover, it was recommended that all events at which schoolchildren gather together be suspended. The supply of H1N1 vaccine in the area was insufficient during this period; thus, few children were vaccinated.
Schoolchildren who had influenza-like symptoms, as determined by their parents, were required to visit a hospital or clinic. Immediately after a child was diagnosed with confirmed, probable, or suspected H1N1 influenza, the child’s parents were instructed to call the school. These children were defined as H1N1 patients in this study. Each such phone call was responded to by the teacher responsible for that child. The teacher confirmed the name, sex, school, grade of each child, and the date of onset of H1N1 influenza, and instructed the parents to keep the child at home until 2 days after his/her body temperature had returned to normal. All data were recorded on a prescribed form, and the designated teacher immediately faxed the form to the headquarters and to the Center for Health, Safety and Environmental Management of Shinshu University. From the data obtained, we confirmed that all patients reported by parents to the school teacher by phone had been diagnosed as H1N1 by a physician. The data were gathered and entered anonymously into a computer for statistical analysis.
The decision to close a class or school was made by the principal of each school based on the number of children infected. The date for the resumption of classes was also decided by the principal after the discussion of each closure case. All closure data, including the start date, the duration of closure, and the date of resumption of classes, were recorded. All durations were expressed in calendar days.
Because the data were collected in a computer database and because this epidemiological study would not cause any harm to any of the subjects, written informed consent was not required. The study design and procedure were reviewed and approved by the Committee for Medical Ethics of Shinshu University (approval number 1616).
Statistical analysis
Continuous variables included the grade of the children, the number of patients, and the closure duration. For analysis, we used the date of the onset of infection and not the date that the infection was reported. The new cases of H1N1 after a class/school closure were recorded starting on the date when classes were resumed. Because the estimated incubation period for H1N1 virus is 1–7 days [20] and because viral shedding almost completely ceases 7 days after infection [21], the H1N1 cases in each class were recorded during the 7 days following the resumption of classes. Only the first closure of each class was utilized for H1N1 cases analysis to avoid the effect of increased immunization of children in classes closed more than once. We also used a dummy variable for school closure, where 0 represented “no closure” and 1 represented “closures performed.” The number of patients and the closures were recorded every day and expressed using a time-course descriptive epidemiological method. Further, the number of patients at each school was summed and used to express the time-course cumulative rate of infection.
For categorical variables, the percentages of patients in each category were calculated and the proportions were compared using the Chi-squared test. A Poisson regression model was used to analyze the effects of several factors on H1N1 cases after the resumption of classes. All statistical analyses were performed using PASW 18 software for Windows (SPSS, Chicago, IL, USA), with P < 0.05 indicating statistical significance.
Results
Numbers of patients and class/school closures
Among the 2,141 children attending the four schools, the cumulative H1N1 case rate was 40.9 % (876 subjects). There were no differences in the cumulative rate between boys and girls at each school. Only two children who had underlying respiratory illnesses were hospitalized, and none died. The median duration of absence from school was 5 days (range 2–16 days).
Time-course of the number of patients
Figure 1 shows the time-course of the epidemic and the closures of the elementary schools, and Fig. 2 shows the curves and closures of the junior high schools. Forty classes were closed a total of 53 times for a median duration of 4 days (range 1–10 days). Although these two districts are located at a distance of 70 km from each other, the epidemic in schoolchildren occurred simultaneously. In district A, H1N1 spread rapidly, and both the elementary school and junior high school were closed in the middle of November 2009 (Figs. 1a and 2a). In district B, however, H1N1 infection spread more slowly, and only classes, not entire schools, were closed throughout this period (Figs. 1b and 2b).
Time-course of the number of patients and closures in the elementary schools. a The elementary school (all 12 classes) in district A was closed in the middle of November 2009, but a small epidemic was observed after the resumption of classes, leading to the closure of some classes. A gray box indicates a class closure for 1 day. b In the elementary school in district B, classes were closed one by one, and H1N1 was seemingly transmitted from class to class. The epidemic peak became greater with time
Time-course of the number of patients and closures in the junior high schools. a In the junior high school in district A, there was no subsequent epidemic after the resumption of classes. b In the junior high school in district B, the epidemic continued, and classes were closed in November and December 2009
In both districts, the number of patients at the elementary school and junior high school peaked during the middle of November 2009. At the elementary schools, both the school closures in district A (Fig. 1a) and the class closures in district B (Fig. 1b) had similar effects on subsequent peaks throughout the study period. Some classes in district A were closed more than once, whereas each class that was closed in district B was closed only once. In addition, class closures in district B were sequential, not simultaneous (Fig. 1b). Closure of the junior high school in district A had significant effects, and there were few subsequent infection peaks (Fig. 2a), whereas class closures in the district B junior high school were followed by another large peak in December 2009 (Fig. 2b).
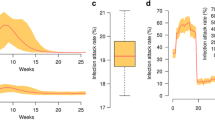
Figure 3 shows the cumulative rate of H1N1 patients in all schools. For both the elementary schools and junior high schools, the cumulative rate was higher in district A than in district B. This difference was likely related to the initial steep upward curve in district A, which indicates that the spread of infection was explosive.
Cumulative rates of H1N1 in children attending the elementary schools and junior high schools. In both a elementary schools and b junior high schools, the initial steep upward curves seemed to be related to the higher cumulative rates. For each type of school, the upward curve occurred when approximately 5 % of the students became infected
H1N1 cases after the resumption of classes
To evaluate the effect of closures, we evaluated the number of H1N1 cases after the resumption of classes. We assessed the first closure of each class (40 closures) and the cases of H1N1 infection that occurred within 7 days after the resumption of classes. We also calculated the effects of possible related factors, including class grade of the children, the duration of the closure, and the type of closure (class or school), using a Poisson regression model for each factor and the number of infections after the resumption of classes.
Table 1 shows the results of the Poisson regression model of the effects of these three factors on infected cases. We confirmed that the closure duration (incidence rate ratio = 0.702; 95 % confidence interval 0.561–0.880, P = 0.002) was significantly related with the number of cases within 7 days after the resumption of classes.
Discussion
We investigated the effect of short-term class/school closures due to the H1N1 epidemic on subsequent infection in schools affiliated with Shinshu University. Although the study sample was very small, including only 40 classes in four schools, the time-course of the epidemic showed that school closure was more effective than class closure in decreasing the number of infections, especially among children attending junior high school. In addition, a longer duration of closure was significantly related to a lower number of cases of infection after the resumption of classes.
School and class closures were implemented after the first wave of the H1N1 epidemic. Previous reports based on actual school closures showed that whole school closures decreased the H1N1 reproductive number [17] or halved the transmission rate among school-age children [18]. These reports showed that school closure is effective against infection spread. In this study, the time-course of patient numbers showed the effects of class or school closures and we evaluated the effect of not only whole school closure but also class closure. In district A, the epidemic did not recur after closure of the junior high school, whereas there was a small increase in the number of infections following the reopening of the elementary school. H1N1 transmission was likely inhibited by school closures. Because H1N1 transmission risk increased among individuals who live in households with younger members [22], it was more difficult to stop the H1N1 epidemic among elementary school children than among junior high school children. Furthermore, children in the junior high school may have better implemented the precautions (e.g., hand washing, gargling) than children in the elementary school because the older children could better understand the importance of these precautions. In addition, a previous report showed that some schoolchildren still met each other during school closure [23], and this potentially facilitated H1N1 transmission, regardless of school closure. Although the contact patterns of children were not investigated in this study, extra-school socialization with classmates might have occurred, especially among the elementary schoolchildren due to less stringent implementation of the measure, which might have induced epidemic recurrence, regardless of school closure. On the other hand, in district B, where class but not school closures were implemented, the epidemic peaked a second time in both the elementary school and the junior high school because class closure alone did not completely inhibit H1N1 transmission. The epidemic curves indicate that continuous transmission among school children in district B likely resulted in a repeat of the epidemic in both the elementary school and the junior high school. These findings suggest that school closure was superior to class closure in reducing the likelihood of a subsequent epidemic, especially among older children. Furthermore, class closure alone may result in a repeat epidemic of a strongly transmissible infectious disease such as H1N1. In addition, further measures of not only school closure but also instructions that children avoid school friends during closure periods will be necessary to strengthen the effect of school closures.
Because the toxicity of H1N1 was recognized to be weak from the start of the pandemic and fatalities were fewer than expected, it could be argued that school closure might not be an essential measure. However, further evolution of the strain might occur without such closures. And because individuals with underlying severe illnesses become critical or even die due to H1N1 infection [5], and the incidence rate of patients with critical illnesses might have increased if the school closure measure had not been applied, we concluded that the school closure measure was necessary to reduce transmission, regardless of low virus toxicity. While vaccination is shown to be the most important infection control measure [24], epidemic control measures without vaccine must be taken when insufficient vaccine is available. Because these closures can decrease and slow the epidemic peak, many more uninfected children may have an opportunity to receive vaccination. Thus, closure measures should be effective when new infections occur in the future. If herd immunity measures are employed to inhibit infectious epidemics, further interventions such as transmission interception and vaccination at not only the school level but also in the wider community will be necessary [13, 15].
In general, classes and schools are closed in order to control the epidemic transmission of infectious viruses shed by patients. However, the optimal duration of closure is unclear, and, to date, there is no standardized method to evaluate the effect of these closures. Simulation models have shown that several weeks of school closures are necessary to reduce the cases of H1N1 [14, 15], but the minimum number of closure days necessary to minimize the cases of influenza infection has not been determined. Longer closures will interfere with the education of children, with the occupations of their parents, and with social or economic activity [16, 25–27]. Our findings suggest that short-term closures, even closures of a few days, effectively decrease the number of infections after the resumption of classes. Our findings also showed that the effects of closure were related to the duration of the closure. Because an epidemic may be influenced by several factors, such as transmission within households [22, 28], the severity or transmissibility of the strain of influenza [15], or weather [18], further detailed investigations that include these factors are required so as to clarify the effects of school closure.
We found that the cumulative rate of H1N1 infection was higher in district A than in district B because the initial epidemic spread explosively in district A, as shown by the steep upward epidemic curve in November 2009, and the cumulative rate was likely to be dependent on the initial epidemic spread. These results indicate that the prevention of the spread of the primary infection may reduce the total number of H1N1-infected individuals, as reported by Collins et al. [29]. In addition, an explosive spread was observed when the cumulative rate exceeded approximately 5 % of students in these schools. Pandemics may be inhibited if precautions are implemented when approximately 2 % of the population is infected, but could not be inhibited when approximately 10 % of the population is infected [29]. Accurate comparison was difficult because the report is old and social systems might be different; however, the measure of early intervention to intercept transmission and to slow the epidemic was substantially essential and effective. Thus, interventions such as school closures should be implemented as soon as possible after the outbreak of an epidemic such as H1N1, before the cumulative rate exceeds 5 % of the population at a school.
This study has several limitations. First, the study sample, consisting of 57 classes at four schools, was small, and, therefore, the results may be only suggestive. Larger samples are needed to determine the detailed effect of class/school closures and to further generalize these results. However, the method we used, recording information correctly at the onset of infection, both before and after closures, is better implemented with small samples. Future research should include larger samples with correct records. Second, the effects of closure were determined without considering weekend effects. In Japan, children do not generally attend elementary school or junior high school on Saturdays and Sundays, and the lack of child-to-child contact on these days may have influenced their overall rate of H1N1 infection. Third, children were monitored by not medical specialists but their parents, and, therefore, there might be children who were not identified as patients due to being oligosymptomatic during the study period. Thus, the patient number might have been underestimated. Fourth, our study was based on self-reports of patients diagnosed with influenza at a hospital or clinic. Although it would have been more accurate to evaluate H1N1 infection by laboratory methods, such as reverse transcription polymerase chain reaction (RT-PCR) or viral culture, as suggested in World Health Organization (WHO) and Centers for Disease Control and Prevention (CDC) guidelines, this was practically impossible. Thus, a few patients diagnosed with H1N1 may have been infected with seasonal influenza or other respiratory diseases with similar symptoms, and we may have overestimated the number of H1N1-infected patients. Because the self-report system of this study involved the judgement of parents and medical diagnosis at a hospital without laboratory methods, potential biases might have arisen. However, because almost all influenza patients in Japan in 2009 were infected with H1N1 [30], it is likely that all patients in this study were infected with H1N1. Fifth, subclinical infections may have altered the effects of class/school closures. An increase in the number of subclinical infections may increase the number of immunized children relative to those absent, thus, reducing epidemic spread. A previous report, however, showed that the rate of subclinical infection was low in Japan in 2009 [31], indicating that the influence of subclinical infection was small.
Conclusions
In this study, we investigated the effect of short-term class/school closures in elementary schools and junior high schools affiliated with Shinshu University in Japan. Our findings suggest that school closures, rather than class closures, better inhibit subsequent epidemics among older children, that closures of longer duration were more effective, and that school closure should be implemented as soon as possible after the start of an outbreak.
References
World Health Organization (WHO). Pandemic (H1N1) 2009. 2009. http://www.who.int/csr/disease/swineflu/en/index.html. Accessed 20 Dec 2011.
Ueda H. The administrative context of the emergency control measures for the pandemic (H1N1) 2009 influenza in Japan. Nihon Koshu Eisei Zasshi. 2010;57:157–64.
Dawood FS, Jain S, Finelli L, Shaw MW, Lindstrom S, Garten RJ, et al. Emergence of a novel swine-origin influenza A (H1N1) virus in humans. N Engl J Med. 2009;360:2605–15.
Fraser C, Donnelly CA, Cauchemez S, Hanage WP, Van Kerkhove MD, Hollingsworth TD, et al. Pandemic potential of a strain of influenza A (H1N1): early findings. Science. 2009;324:1557–61.
Girard MP, Tam JS, Assossou OM, Kieny MP. The 2009 A (H1N1) influenza virus pandemic: a review. Vaccine. 2010;28:4895–902.
Miller E, Hoschler K, Hardelid P, Stanford E, Andrews N, Zambon M. Incidence of 2009 pandemic influenza A H1N1 infection in England: a cross-sectional serological study. Lancet. 2010;375:1100–8.
Uchida M, Tsukahara T, Kaneko M, Washizuka S, Kawa S. Swine-origin influenza A outbreak 2009 at Shinshu University, Japan. BMC Public Health. 2011;11:79.
Uchida M, Tsukahara T, Kaneko M, Washizuka S, Kawa S. How the H1N1 influenza epidemic spread among university students in Japan: experience from Shinshu University. Am J Infect Control. 2012;40:218–20.
Lessler J, Reich NG, Cummings DA, Nair HP, Jordan HT, Thompson N. Outbreak of 2009 pandemic influenza A (H1N1) at a New York City school. N Engl J Med. 2009;361:2628–36.
Centers for Disease Control and Prevention (CDC). Outbreak of 2009 pandemic influenza A (H1N1) at a school—Hawaii, May 2009. MMWR Morb Mortal Wkly Rep. 2010;58:1440–4.
Van D, McLaws ML, Crimmins J, MacIntyre CR, Seale H. University life and pandemic influenza: attitudes and intended behaviour of staff and students towards pandemic (H1N1) 2009. BMC Public Health. 2010;10:130.
Stevenson E, Barrios L, Cordell R, Delozier D, Gorman S, Koenig LJ, et al. Pandemic influenza planning: addressing the needs of children. Am J Public Health. 2009;99:S255–60.
Cauchemez S, Donnelly CA, Reed C, Ghani AC, Fraser C, Kent CK, et al. Household transmission of 2009 pandemic influenza A (H1N1) virus in the United States. N Engl J Med. 2009;361:2619–27.
Lee BY, Brown ST, Cooley P, Potter MA, Wheaton WD, Voorhees RE, et al. Simulating school closure strategies to mitigate an influenza epidemic. J Public Health Manag Pract. 2010;16:252–61.
Halder N, Kelso JK, Milne GJ. Develo** guidelines for school closure interventions to be used during a future influenza pandemic. BMC Infect Dis. 2010;10:221.
Halder N, Kelso JK, Milne GJ. Analysis of the effectiveness of interventions used during the 2009 A/H1N1 influenza pandemic. BMC Public Health. 2010;10:168.
Wu JT, Cowling BJ, Lau EH, Ip DK, Ho LM, Tsang T, et al. School closure and mitigation of pandemic (H1N1) 2009, Hong Kong. Emerg Infect Dis. 2010;16:538–41.
Earn DJ, He D, Loeb MB, Fonseca K, Lee BE, Dushoff J. Effects of school closure on incidence of pandemic influenza in Alberta, Canada. Ann Intern Med. 2012;156:173–81.
Sasaki A, Hoen AG, Ozonoff A, Suzuki H, Tanabe N, Seki N, et al. Evidence-based tool for triggering school closures during influenza outbreaks, Japan. Emerg Infect Dis. 2009;15:1841–3.
Sullivan SJ, Jacobson RM, Dowdle WR, Poland GA. 2009 H1N1 influenza. Mayo Clin Proc. 2010;85:64–76.
Carrat F, Vergu E, Ferguson NM, Lemaitre M, Cauchemez S, Leach S, et al. Time lines of infection and disease in human influenza: a review of volunteer challenge studies. Am J Epidemiol. 2008;167:775–85.
Sikora C, Fan S, Golonka R, Sturtevant D, Gratrix J, Lee BE, et al. Transmission of pandemic influenza A (H1N1) 2009 within households: Edmonton, Canada. J Clin Virol. 2010;49:90–3.
Jackson C, Mangtani P, Vynnycky E, Fielding K, Kitching A, Mohamed H, et al. School closures and student contact patterns. Emerg Infect Dis. 2011;17:245–7.
Centers for Disease Control and Prevention (CDC). Prevention and control of influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices (ACIP), 2011. MMWR Morb Mortal Wkly Rep. 2011;60:1128–32.
Cauchemez S, Ferguson NM, Wachtel C, Tegnell A, Saour G, Duncan B, et al. Closure of schools during an influenza pandemic. Lancet Infect Dis. 2009;9:473–81.
Centers for Disease Control and Prevention (CDC). Parental attitudes and experiences during school dismissals related to 2009 influenza A (H1N1)—United States, 2009. MMWR Morb Mortal Wkly Rep. 2010;59:1131–4.
Keogh-Brown MR, Smith RD, Edmunds JW, Beutels P. The macroeconomic impact of pandemic influenza: estimates from models of the United Kingdom, France, Belgium and The Netherlands. Eur J Health Econ. 2010;11:543–54.
Cowling BJ, Chan KH, Fang VJ, Lau LL, So HC, Fung RO, et al. Comparative epidemiology of pandemic and seasonal influenza A in households. N Engl J Med. 2010;362:2175–84.
Collins SD, Frost WH, Gover M, Sydenstricker E. Mortality from influenza and pneumonia in 50 large cities of the United States, 1910–1929. Public Health Rep. 1930;45:2277–328.
National Institute of Infectious Diseases (NIID), Japan. A survey for H1N1 influenza in Japan. 2009. http://idsc.nih.go.jp/disease/swine_influenza/webcast/pdf/3.pdf. Accessed 20 Dec 2011.
Tsai TF, Pedotti P, Hilbert A, Lindert K, Hohenboken M, Borkowski A et al. Regional and age-specific patterns of pandemic H1N1 influenza virus seroprevalence inferred from vaccine clinical trials, August–October 2009. Euro Surveill. 2010;15:1–4.
Acknowledgments
We thank Tomoko Fujimura, Hiroko Hayashi, Saemi Tokuhara, Hiroko Takeda, Kuniyo Kodama, Rieko Nishizawa, Midori Fuse, Naomi Yuzawa, Hiromi Saguchi, Koji Kamijo, Yasuyoshi Matsushima, Kazuki Nagai, Junichi Kitamura, Masashi Miura, Naohisa Kuraishi, Kazumi Maeshima, Dr. Tetsuo Nomiyama, and other organization members for their assistance in the collection and analysis of the data.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Uchida, M., Tsukahara, T., Kaneko, M. et al. Effect of short-term school closures on the H1N1 pandemic in Japan: a comparative case study. Infection 40, 549–556 (2012). https://doi.org/10.1007/s15010-012-0304-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-012-0304-z