Abstract
Background:
Injectable Platelet Rich Fibrin (I-PRF) and Advanced-Platelet Rich Fibrin (A-PRF) are autologous materials derived from patients’ blood and employed in periodontal regenerative surgery. Although I-PRF and A-PRF have different characteristics, their biological effects on gingival tissue fibroblasts remain unclear. This research aims to compare the in vitro capacity in inducing gene expression and proliferation of human gingival fibroblasts between A-PRF and I-PRF.
Methods:
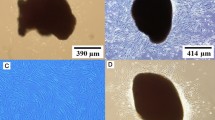
Human donors undergoing dental implant surgery were sampled for normal human gingival fibroblasts (NHGFCs), followed by preparing A-PRF and I-PRF membranes. Enzyme-linked immunosorbent assay (ELISA) kit was used to assess the release of platelet-derived growth factor-AA (PDGF-AA), transforming growth factor-beta1 (TGF- β1), and insulin growth factor-1 (IGF-1) at different periods. Cell viability and proliferation of A-PRF and I-PRF were compared using CCK-8 assay. The impacts of platelet concentration on human gingival fibroblast cells (HGFCs) were evaluated by quantifying the level or amount of phosphorylated extracellular signal-regulated protein kinase (p-ERK), and Matrix metalloproteinases (MMPs), MMP-1 and MMP-3. The effects of PRF on aged human gingival fibroblast cells were examined retrospectively.
Results:
Overall, A-PRF demonstrated a higher release of TGF-B1 and PDGF-AA, while I-PRF reflected higher levels of IGF-1. A significantly higher level of cell proliferation was induced by higher cell proliferation by A-PRF and I-PRF. Additionally, in comparison to I-PRF, the expression of ERK phosphorylation and MMP-1 &MMP-3 in HGFCs was demonstrated by I-PRF and A-PRF. The increase in A-PRF was time-dependent (p < 0.05).
Conclusion:
Both I-PRF and A-PRF induced a stimulatory biological impact on the proliferation of human gingiva fibroblasts, with the latter demonstrating better capacity in facilitating the release of different growth factors. A-PRF also induced higher gene expression of p-ERK, MMP-1 &MMP-3, and the proliferation of fibroblasts.






Similar content being viewed by others
Data availability statement
All relevant study data are available in the tables and figures of the manuscript. If you need more details, please contact the corresponding author.
References
Reid CB, Cloos J, Snow GB, Braakhuis BJ. A simple and reliable technique for culturing of human oral keratinocytes and fibroblasts. Acta Otolaryngol. 1997;117:628–33.
Wanichpakorn S, Kedjarune-Laggat U. Primary cell culture from human oral tissue: gingival keratinocytes, gingival fibroblasts and periodontal ligament fibroblasts. Songklanakarin J Sci Technol. 2010;32:327–31.
Kedjarune U, Pongprerachok S, Arpornmaeklong P, Ungkusonmongkhon K. Culturing primary human gingival epithelial cells: comparison of two isolation techniques. J Craniomaxillofac Surg. 2001;29:224–31.
Klingbeil MFG, Herson MR, Cristo EB, dos Santos Pinto D, Yoshito D, Mathor MB. Comparison of two cellular harvesting methods for primary human oral culture of keratinocytes. Cell Tissue Bank. 2009;10:197–204.
Lauer G, Otten JE, von Specht BU, Schilli W. Cultured gingival epithelium: a possible suitable material for pre-prosthetic surgery. J Craniomaxillofac Surg. 1991;19:21–6.
Pinto N, Quirynen M. RE: Optimized platelet-rich fibrin with the low-speed concept: Growth factor release, biocompatibility, and cellular response. J Periodontol. 2019;90:119–21.
Fujioka-Kobayashi M, Miron RJ, Hernandez M, Kandalam U, Zhang Y, Choukroun J. Optimized platelet‐rich fibrin with the low‐speed concept: growth factor release, biocompatibility, and cellular response. J Periodontol. 2017;88:112–21.
Chang YC, Zhao JH. Effects of platelet‐rich fibrin on human periodontal ligament fibroblasts and application for periodontal infrabony defects. Aust Dental J. 2011;56:365–71.
Strauss FJ, Nasirzade J, Kargarpoor Z, Stähli A, Gruber R. Effect of platelet-rich fibrin on cell proliferation, migration, differentiation, inflammation, and osteoclastogenesis: a systematic review of in vitro studies. Clin Oral Invest. 2020;24:569–84.
Ghanaati S, Booms P, Orlowska A, Kubesch A, Lorenz J, Rut-kowski J, Landes C, Sader R, Kirkpatrick C, Choukroun J. Advanced platelet-rich fibrin: a new concept for cell-based tissue engineering by means of inflammatory cells. J Oral Implantol. 2014;40:679–89.
Kobayashi E, Flückiger L, Fujioka-Kobayashi M, Sawada K, Sculean A, Schaller B, et al. Comparative release of growth factors from PRP PRF, and advanced-PRF. Clin Oral Invest. 2016;20:2353–60.
Mudalal M, Wang Z, Mustafa S, Liu Y, Wang Y, Yu J, et al. Effect of Leukocyte-Platelet Rich Fibrin (L-PRF) on Tissue Regeneration and Proliferation of Human Gingival Fibroblast Cells Cultured Using a Modified Method. Tissue Eng Regen Med. 2021;18:895–904.
Wang X, Yang Y, Zhang Y, Miron RJ. Fluid platelet-rich fibrin stimulates greater dermal skin fibroblast cell migration, proliferation, and collagen synthesis when compared to platelet-rich plasma. J Cosmet Dermatol. 2019;18:2004–10.
Lundquist R, Dziegiel MH, Ågren MS. Bioactivity and stability of endogenous fibrogenic factors in platelet-rich fibrin. Wound Repair Regen. 2008;16:356–63.
Chang YC, Zhao JH. Effects of platelet-rich fibrin on human periodontal ligament fibroblasts and application for periodontal infrabony defects. Aust Dent J. 2011;56:365–71.
Miron RJ, Fujioka-Kobayashi M, Hernandez M, Kandalam U, Zhang Y, Ghanaati S, Choukroun J. Injectable platelet rich fibrin (i-PRF): opportunities in regenerative dentistry? Clin Oral Invest. 2017;21:2619–27.
Horowitz R, Holtzclaw D, Rosen PS. A review on alveolar ridge preservation following tooth extraction. J Eviden Based Dental Pract. 2012;12:149–60.
Lee CT, Chiu TS, Chuang SK, Tarnow D, Stoupel J. Alterations of the bone dimension following immediate implant placement into extraction socket: systematic review and meta-analysis. J Clin Periodontol. 2014;41:914–26.
Morjaria KR, Wilson R, Palmer RM. Bone healing after tooth extraction with or without an intervention: a systematic review of randomized controlled trials. Clin Implant Dent Relat Res. 2014;16:1–20.
Tan WL, Wong TL, Wong MC, Lang NP. A systematic review of post-extractional alveolar hard and soft tissue dimensional changes in humans. Clin Oral Implant Res. 2012;23:1–21.
Bi J, Intriago MFB, Koivisto L, Jiang G, Häkkinen L, Larjava H. Leucocyte-and platelet-rich fibrin regulates expression of genes related to early wound healing in human gingival fibroblasts. J Clin Periodontol. 2020;47:851–62.
Mudalal M, Sun X, Li X, Zhou Y. The evaluation of leukocyte-platelet rich fibrin as an anti-inflammatory autologous biological additive: a novel in vitro study. Saudi Med J. 2019;40:657.
Boora P, Rathee M, Bhoria M. Effect of platelet rich fibrin (PRF) on peri-implant soft tissue and crestal bone in one-stage implant placement: a randomized controlled trial. J Clin Diagnostic Res. 2015;9:ZC18.
Wang Z, Mudalal M, Sun Y, Liu Y, Wang J, Wang Y, et al. The effects of leukocyte-platelet rich fibrin (L-PRF) on suppression of the expressions of the pro-inflammatory cytokines, and proliferation of Schwann cell, and neurotrophic factors. Sci Rep. 2020;10:1–10.
Chan CM, Chang HH, Wang VC, Huang CL, Hung CF. Inhibitory effects of resveratrol on PDGF-BB-induced retinal pigment epithelial cell migration via PDGFRβ, PI3K/Akt and MAPK pathways. PLoS One. 2013;8:e56819.
Maucksch C, McGregor A, Yang M, Gordon R, Connor B. IGF-I redirects doublecortin-positive cell migration in the normal adult rat brain. Neuroscience. 2013;241:106–15.
Mudalal M, Wang Z, Mustafa S, Liu Y, Wang Y, Yu J, et al. Effect of leukocyte-platelet rich fibrin (L-PRF) on tissue regeneration and proliferation of human gingival fibroblast cells cultured using a modified method. Tissue Eng Regen Med. 2021;18:895–904.
Chang IC, Tsai CH, Chang YC. Platelet-rich fibrin modulates the expression of extracellular signal-regulated protein kinase and osteoprotegerin in human osteoblasts. J Biomed Mater Res, Part A. 2010;95:327–32.
Acknowledgements
This research was funded by the 1) Lanzhou Talent Innovation and Venture Project (2017-RC-31), 2) Competitive Projects for Science and Technology Innovation and Development of Gansu Province (2018ZX-10), and 3) Gansu Key Technologies R&D Program for International S&T Cooperation and Exchange (18YF1WA116).
Author information
Authors and Affiliations
Contributions
Conceptualization: LY, SHA, and MM; methodology: SHA, and MM; software: RA-A, OAA-A; validation: OAA-A; formal analysis: LY; investigation: MM; resources, and data curation: SHA and LY; writing—original draft preparation: SHA; writing—review and editing: MM, OAA-A, and WL; supervision: LY and WL; project administration: OAA-A, RA-A; funding acquisition: LY.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to disclose.
Ethical statement
The study was approved by the Ethics Committee of the School/Hospital of Stomatology, Lanzhou University, China (LZUKQ-2022-030).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ashour, S.H., Mudalal, M., Al-Aroomi, O.A. et al. The Effects of Injectable Platelet-Rich Fibrin and Advanced-Platelet Rich Fibrin on Gingival Fibroblast Cell Vitality, Proliferation, Differentiation. Tissue Eng Regen Med 20, 1161–1172 (2023). https://doi.org/10.1007/s13770-023-00586-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13770-023-00586-1