Abstract
Minor and severe burn injuries are common and highly complicated pathology causing huge mortality and costly wound treatment protocols. In this work, an injectable microgel assembly was developed to accelerate burn wound healing rate and quality where the network formation occurred after injection of the precursor on the wound bed. Poly(hexamethylene biguanide) (PHMB), an amine-containing antibacterial polymer, was synthesized and functioned as a linker of microgels by the addition of a specific deep eutectic solvent (DES) as a catalyst for particles connection. The major function of the eutectic mixture was to assist in the cross-linking of the microgels; however, it could play as an antibacterial agent against Gram + bacteria. The THDES was prepared by the reaction of arginine with ascorbic acid (Asc), and glycerol ([DES]Arg/G,A), two of which are known as the components involved in the wound healing process. Depending on the PHMB concentration, the microgel assembly experienced a gel-to-sol transition under shear stresses ranging from 104 to 105 Pa and exhibited much stronger antibacterial activities as the fraction of PHMB increased. Application of the developed hydrogel promoted healing of the infected burned rat, enhanced re-epithelialization, and attenuated the formation of fibrotic scar tissue.
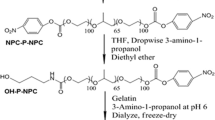
Graphical abstract














Similar content being viewed by others
References
Bakadia M, Lamboni L, Ahmed Q, Zheng R, Boni O, Shi Z, Yang G (2023) Antibacterial silk sericin/poly(vinyl alcohol) hydrogel with antifungal property for potential infected large burn wound healing: systemic evaluation. Smart Mater Med 4:37–58
Dong Y, Cui M, Qu J, Wang X, Kwon SH, Barrera J, Gurtner G (2020) Conformable hyaluronic acid hydrogel delivers adipose-derived stem cells and promotes regeneration of burn injury. Acta Biomater 108:56–66
Ng JY, Zhu X, Mukherjee D, Zhang C, Hong S, Kumar Y, Ee PL (2021) Pristine gellan gum–collagen interpenetrating network hydrogels as mechanically enhanced anti-inflammatory biologic wound dressings for burn wound therapy. ACS Appl Biomater 4:1470–1482
Margolis DJ, Gupta J, Hoffstad O, Papdopoulos M, Glick HA, Thom SR, Mitra N (2013) Lack of effectiveness of hyperbaric oxygen therapy for the treatment of diabetic foot ulcer and the prevention of amputation: a cohort study. Diabetes Care 36:1961–1966
Hartmann DD, Martins RP, da Silva TC, Stefanello ST, Courtes AA, Gonçalves DF, Furtado ABV, Duarte BSL, Signori LU, Soares FAA, Puntel GO (2021) Oxidative stress is involved in LLLT mechanism of action on skin healing in rats. Braz J Med Biol Res 54:1–9
Tehrani FK, Sheikhi M, Rafiemanzelat F, Esmaeili F, Ghodsi S, Koohmareh GA, Ghalavand B (2022) Protein and polysaccharide-based asymmetric mat with tuned bilayer configuration for enhanced wound healing efficiency. Carbohydr Polym 292:119666
Shakiba M, Sheikhi M, Pahnavar Z, Tajiki A, Bigham A, Foroozandeh A, Abdouss M (2023) Development of an antibacterial and antioxidativenanofibrous membrane using curcumin-loaded halloysite nanotubes for smart wound healing: In vitro and in vivo studies. Int J Pharm 642:123207
Shahriari-Khalaji M, Sattar M, Cao R, Zhu M (2023) Angiogenesis, hemocompatibility and bactericidal effect of bioactive natural polymer-based bilayer adhesive skin substitute for infected burned wound healing. Bioact Mater 29:177–195
Bhatnagar P, Law JX, Ng SF (2022) Delivery systems for platelet derived growth factors in wound healing: a review of recent developments and global patent landscape. J Drug Deliv Sci Technol 71:103270
Yao Y, Zhang A, Yuan C, Chen X, Liu Y (2021) Recent trends on burn wound care: hydrogel dressings and scaffolds. Biomater Sci 9:4523–4540
Alavi M, Nokhodchi A (2022) Antimicrobial and wound healing activities of electrospun nanofibers based on functionalized carbohydrates and proteins. Cellulose 29:1331–1347
Zia T, Usman M, Sabir A, Shafiq M, Khan RU (2020) Development of inter-polymeric complex of anionic polysaccharides, alginate/k-carrageenan bio-platform for burn dressing. Int J Biol Macromol 157:83–95
Qazi TH, Burdick JA (2021) Granular hydrogels for endogenous tissue repair. Bioprocess Biosyst Eng 1:1–3
Feng Q, Li D, Li Q, Cao X, Dong H (2022) Microgel assembly: Fabrication, characteristics and application in tissue engineering and regenerative medicine. Bioact Mater 9:105–119
Feng Q, Li D, Li Q, Li S, Huang H, Li H, Dong H, Cao X (2022) Dynamic nanocomposite microgelassembly with microporosity, injectability, tissue-adhesion, and sustained drug release promotes articular cartilage repair and regeneration. Adv Healthc Mater 11:e2102395
Cui T, Yu J, Wang CF, Chen S, Li Q, Guo K, Qing R, Wang G, Ren J (2022) Micro-gel ensembles for accelerated healing of chronic wound via pH regulation. Adv Sci 9:1–12
Sheikhi M, Rafiemanzelat F, Moroni L, Setayeshmehr M (2021) Ultrahigh-water-content biocompatible gelatin-based hydrogels: Toughened through micro-sized dissipative morphology as an effective strategy. Mater Sci Eng C 120:1–15
Sheikhi M, Rafiemanzelat F, Sadeghpour N, Shams M, Esfahani AN (2021) Deep eutectic solvents based on l-Arginine and glutamic acid as green catalysts and conductive agents for epoxy resins. J Mol Liq 343:117568
Sheikhi M, Rafiemanzelat F, Ghodsi S, Moroni L, Setayeshmehr M (2022) 3D printing of jammed self-supporting microgels with alternative mechanism for shape fidelity, crosslinking and conductivity. Addit Manuf 58:102997
Rahman MS, Roy R, Jadhav B, Hossain MN, Halim MA, Raynie DE (2021) Formulation, structure, and applications of therapeutic and amino acid-based deep eutectic solvents: an overview. J Mol Liq 321:3761–3776
Değim Z, Çelebi N, Alemdaroğlu C, Deveci M, Öztürk S, Özoğul C (2011) Evaluation of chitosan gel containing liposome-loaded epidermal growth factor on burn wound healing. Int Wound J 8:343–354
Rana MM, Rahman MS, Ullah MA, Siddika A, Hossain ML, Akhter MS, Hasan MZ, Asaduzzaman SM (2020) Amnion and collagen-based blended hydrogel improves burn healing efficacy on a rat skin wound model in the presence of wound dressing biomembrane. Biomed Mater Eng 31:1–17
Xu C, Molino BZ, Wang X, Cheng F, Xu W, Molino P, Bacher M, Su D, Rosenau T, Willför S, Wallace G (2018) 3D printing of nanocellulose hydrogel scaffolds with tunable mechanical strength towards wound healing application. J Mater Chem B 6:7066–7075
Ousey K, Cutting KF, Rogers AA, Rippon MG (2016) The importance of hydration in wound healing: reinvigorating the clinical perspective. J Wound Care 25:122–130
Rousselle P, Montmasson M, Garnier C (2019) Extracellular matrix contribution to skin wound re-epithelialization. Matrix Biol 75:12–26
Veith AP, Henderson K, Spencer A, Sligar AD, Baker AB (2019) Therapeutic strategies for enhancing angiogenesis in wound healing. Adv Drug Deliv Rev 146:97–125
Morgan FL, Moroni L, Baker MB (2020) Dynamic bioinks to advance bioprinting. Adv Healthc Mater 9:1–18
Moores J (2013) Vitamin C: a wound healing perspective. Br J Community Nurs 18:S6–S11
Zhou Y, Liu G, Huang H, Wu J (2021) Advances and impact of arginine-based materials in wound healing. J Mater Chem B 9:6738–6750
Taysun MB, Sert E, Atalay FS (2016) Physical properties of benzyl tri-methyl ammonium chloride based deep eutectic solvents and employment as catalyst. J Mol Liq 223:845–852
Wikene KO, Rukke HV, BruzellE THH (2017) Investigation of the antimicrobial effect of natural deep eutectic solvents (NADES) as solvents in antimicrobial photodynamic therapy. J Photochem Photobiol B Biol 171:27–33
Alshameri AW, Owais M (2022) Antibacterial and cytotoxic potency of the plant-mediated synthesis of metallic nanoparticles Ag NPs and ZnO NPs: a review. Open Nano 8:1–23
Tian EK, Wang Y, Ren R, Zheng W, Liao W (2021) Gold nanoparticle: recent progress on its antibacterial applications and mechanisms. J Nanomater 2021:1–18
Yousefi SR, Alshamsi HA, Amiri O, Salavati-Niasari M (2021) Synthesis, characterization and application of Co/Co3O4 nanocomposites as an effective photocatalyst for discoloration of organic dye contaminants in wastewater and antibacterial properties. J Mol Liq 337:1–10
Singh TA, Sharma A, Tejwan N, Ghosh N, Das J, Sil PC (2021) A state of the art review on the synthesis, antibacterial, antioxidant, antidiabetic and tissue regeneration activities of zinc oxide nanoparticles. Adv Colloid Interface Sci 295:1–23
Menazea AA, Ahmed MK (2020) Synthesis and antibacterial activity of graphene oxide decorated by silver and copper oxide nanoparticles. J Mol Struct 1218:1–27
Albukhaty S, Al-Bayati L, Al-Karagoly H, Al-Musawi S (2022) Preparation and characterization of titanium dioxide nanoparticles and in vitro investigation of their cytotoxicity and antibacterial activity against Staphylococcus aureus and Escherichia coli. Anim Biotechnol 33:864–870
Lai PL, Hong DW, Ku KL, Lai ZT, Chu IM (2014) Novel thermosensitive hydrogels based on methoxy polyethylene glycol-co-poly(lactic acid-co-aromatic anhydride) for cefazolin delivery. Nanotechnol Biol Med 10:553–560
Posadowska U, Brzychczy-Wloch M, Pamula E (2016) Injectable gellan gum-based nanoparticles-loaded system for the local delivery of vancomycin in osteomyelitis treatment. J Mater Sci Mater Med 27:1–9
Wang X, Liu Z, Ye X, Hu K, Zhong H, Yuan X, **ong H, Guo Z (2015) A facile one-pot method to two kinds of graphene oxide-based hydrogels with broad-spectrum antimicrobial properties. Chem Eng J 260:331–337
Venkatesan J, Jayakumar R, Mohandas A, Bhatnagar I, Kim SK (2014) Antimicrobial activity of chitosan-carbon nanotube hydrogels. Materials 7:3946–3955
Li S, Dong S, Xu W, Tu S, Yan L, Zhao C, Ding J, Chen X (2018) Antibacterial hydrogels. Adv Sci 5:1–17
Ndlovu SP, Ngece K, Alven S, Aderibigbe BA (2021) Gelatin-based hybrid scaffolds: promising wound dressings. Polymers 13:1–31
Brauer E, Lippens E, Klein O, Nebrich G, Schreivogel S, Korus G, Petersen A (2019) Collagen fibrils mechanically contribute to tissue contraction in an in vitro wound healing scenario. Adv Sci 6:1801780
Mathew-Steiner SS, Roy S, Sen CK (2021) Collagen in wound healing. Bioengineering 8:1–15
Acknowledgements
Appreciation is extended to the Office of Vice Chancellor for Research and Technology of the University of Isfahan. Technical support by Dr. SiamakBeheshti for In Vivo Evaluations from the Department of Plant and Animal Biology, Faculty of Biological Science and Technology, University of Isfahan is gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ghorbani, M., Davoudi, S.M., Gouvarchinghaleh, H.E. et al. Injectable hydrogel incorporated with poly(hexamethylene biguanide) and deep eutectic solvent as linker and highly efficient antibacterial agents for bacteria-infected burnt wound. Iran Polym J 33, 419–434 (2024). https://doi.org/10.1007/s13726-023-01262-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13726-023-01262-w