Abstract
Purpose of Review
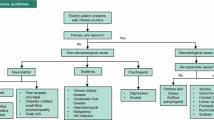
Pruritis is a highly prevalent symptom in older adults significantly impacting their quality of life. It can manifest in the geriatric population due to a spectrum of etiologies including dermatological, systemic, psychological, medication-induced, and idiopathic causes. The purpose of this review was to explore pruritus in older adults with a discussion of common causes and current standards of management with a focus on the latest innovations within the last five years.
Recent Findings
Common dermatological causes of pruritus in the elderly are atopic dermatitis, prurigo nodularis, psoriasis, seborrheic dermatitis, and transient Acantholytic Dermatosis also known as Grover’s disease. Noteworthy systemic causes are uremic or chronic kidney disease-associated pruritus, cholestatic disease, and paraneoplastic causes although additional etiologies such as neuropathic, psychogenic, drug-induced, or idiopathic itch must also be considered. Topical emollients and gentle cleansers are the foundation of managing pruritus in the elderly with adjuvant therapy focused on addressing the underlying trigger. Recent findings demonstrate immunobiologics having a greater role in treating skin conditions that cause pruritus although a variety of topical formulations are being investigated. The latest research on systemic causes of pruritus in the elderly is focused on addressing the underlying condition. Psychiatric medications and behavioral interventions are being explored for neuropathic and idiopathic causes of itch respectively.
Summary
Given the significant impact of pruritus on the quality of life of older adults, there is a need for further research on effective interventions for pruritus specifically among the elderly.

Similar content being viewed by others
Data Availability
No datasets were generated or analysed during the current study.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
James WD, Elston DM, Treat JR, Rosenbach MA. Andrews’ Diseases of the Skin. 13th ed. Elsevier.
**e B, Li X. Inflammatory mediators causing cutaneous chronic itch in some diseases via transient receptor potential channel subfamily V member 1 and subfamily A member 1. J Dermatol. 2019;46(3):177–85.
• Caplan Z. 2020 Census: 1 in 6 People in the United States Were 65 and Over [Internet]. United States Census Bureau; 2023. Available from: https://www.census.gov/library/stories/2023/05/2020-census-united-states-older-population-grew.html. Most recent census data suggests that the number of older adults in the US is growing.
Ständer S, Weisshaar E, Mettang T, Szepietowski JC, Carstens E, Ikoma A, et al. Clinical Classification of Itch: a Position Paper of the International Forum for the Study of Itch. Acta Derm Venereol. 2007;87(4):291–4.
Pruritus in the elderly - ClinicalKey [Internet]. [cited 2024 Jan 31]. Available from: https://www-clinicalkey-com.libproxy.lib.unc.edu/#!/content/playContent/1-s2.0-S0738081X10001173?returnurl=https:%2F%2Flinkinghub.elsevier.com%2Fretrieve%2Fpii%2FS0738081X10001173%3Fshowall%3Dtrue&referrer=https:%2F%2Fpubmed.ncbi.nlm.nih.gov%2F.
Causes, pathophysiology, and treatment of pruritus in the mature patient - ClinicalKey [Internet]. [cited 2024 Jan 31]. Available from: https://www-clinicalkey-com.libproxy.lib.unc.edu/#!/content/playContent/1-s2.0-S0738081X17301955?returnurl=null&referrer=null.
Chan LN, Magyari A, Ye M, Al-Alusi NA, Langan SM, Margolis D, et al. The epidemiology of atopic dermatitis in older adults: A population-based study in the United Kingdom. PLoS ONE. 2021;16(10):e0258219.
Frazier W. Bhardwaj N. Atopic Dermatitis: Diagnosis and Treatment afp. 2020;101(10):590–8.
Cleveland Clinic [Internet]. [cited 2024 Jan 31]. Medications on the Beers Criteria List. Available from: https://my.clevelandclinic.org/health/articles/24946-beers-criteria.
Tannenbaum C, Paquette A, Hilmer S, Holroyd-Leduc J, Carnahan R. A Systematic Review of Amnestic and Non-Amnestic Mild Cognitive Impairment Induced by Anticholinergic, Antihistamine. GABAergic and Opioid Drugs Drugs Aging. 2012;29(8):639–58.
Klein PA, Clark RAF. An Evidence-Based Review of the Efficacy of Antihistamines in Relieving Pruritus in Atopic Dermatitis. Arch Dermatol. 1999;135(12):1522–5.
•• Drucker AM, Lam M, Flohr C, Thyssen JP, Kabashima K, Bissonnette R, et al. Systemic therapy for atopic dermatitis in older adults and adults with comorbidities: a sco** review and International Eczema Council survey. Dermatitis. 2022;33(3):200–6. The treatment landscape of atopic dermatitis has shifted significantly since the approval of multiple systemic medications and biologics. This recent review highlights these advances but notes that older adults are often excluded from clinical trials for these therapies due to age or associated comorbidities.
Blauvelt A, Teixeira HD, Simpson EL, Costanzo A, De Bruin-Weller M, Barbarot S, et al. Efficacy and Safety of Upadacitinib vs Dupilumab in Adults With Moderate-to-Severe Atopic Dermatitis: A Randomized Clinical Trial. JAMA Dermatol. 2021;157(9):1047.
•• Reich K, Thyssen JP, Blauvelt A, Eyerich K, Soong W, Rice ZP, et al. Efficacy and safety of abrocitinib versus dupilumab in adults with moderate-to-severe atopic dermatitis: a randomised, double-blind, multicentre phase 3 trial. Lancet. 2022;400(10348):273–82. This phase 3 trial demonstrated that abrocitinib 200 mg may be more efficacious than dupilumab for the treatment of moderate to severe atopic dermatitis. This suggests that oral treatment may be possible alternatives to subcutaneous injections for AD.
Wollenberg A, Howell MD, Guttman-Yassky E, Silverberg JI, Kell C, Ranade K, et al. Treatment of atopic dermatitis with tralokinumab, an anti–IL-13 mAb. Journal of Allergy and Clinical Immunology. 2019;143(1):135–41.
Lam M, Zhu JW, Maqbool T, Adam G, Tadrous M, Rochon P, et al. Inclusion of Older Adults in Randomized Clinical Trials for Systemic Medications for Atopic Dermatitis: A Systematic Review. JAMA Dermatol. 2020;156(11):1240–5.
Ständer S, Augustin M, Berger T, Elmariah S, Korman NJ, Weisshaar E, et al. Prevalence of prurigo nodularis in the United States of America: A retrospective database analysis. JAAD Int. 2020;1(2):28–30.
Williams KA, Huang AH, Belzberg M, Kwatra SG. Prurigo nodularis: Pathogenesis and management. J Am Acad Dermatol. 2020;83(6):1567–75.
Iking A, Grundmann S, Chatzigeorgakidis E, Phan NQ, Klein D, Ständer S. Prurigo as a symptom of atopic and non-atopic diseases: aetiological survey in a consecutive cohort of 108 patients. J Eur Acad Dermatol Venereol. 2013;27(5):550–7.
Pereira MP, Steinke S, Zeidler C, Forner C, Riepe C, Augustin M, et al. European academy of dermatology and venereology European prurigo project: expert consensus on the definition, classification and terminology of chronic prurigo. J Eur Acad Dermatol Venereol. 2018;32(7):1059–65.
Fostini AC, Girolomoni G, Tessari G. Prurigo nodularis: an update on etiopathogenesis and therapy. J Dermatol Treat. 2013;24(6):458–62.
Ständer S, Luger T, Metze D. Treatment of prurigo nodularis with topical capsaicin. J Am Acad Dermatol. 2001;44(3):471–8.
Ständer S, Schürmeyer-Horst F, Luger TA, Weisshaar E. Treatment of pruritic diseases with topical calcineurin inhibitors. Ther Clin Risk Manag. 2006;2(2):213–8.
Siepmann D, Lotts T, Blome C, Braeutigam M, Phan NQ, Butterfass-Bahloul T, et al. Evaluation of the Antipruritic Effects of Topical Pimecrolimus in Non-Atopic Prurigo Nodularis: Results of a Randomized, Hydrocortisone-Controlled. Double-Blind Phase II Trial Dermatology. 2013;227(4):353–60.
Wong SS, Goh CL. Double-blind, Right/Left Comparison of Calcipotriol Ointment and Betamethasone Ointment in the Treatment of Prurigo Nodularis. Arch Dermatol. 2000;136(6):807–8.
Tamagawa-Mineoka R, Katoh N, Ueda E, Kishimoto S. Narrow-band ultraviolet B phototherapy in patients with recalcitrant nodular prurigo. J Dermatol. 2007;34(10):691–5.
Karvonen J, Hannuksela M. Long term results of topical trioxsalen PUVA in lichen planus and nodular prurigo. Acta Derm Venereol Suppl (Stockh). 1985;120:53–5.
•• Yosipovitch G, Mollanazar N, Ständer S, Kwatra SG, Kim BS, Laws E, et al. Dupilumab in patients with prurigo nodularis: two randomized, double-blind, placebo-controlled phase 3 trials. Nat Med. 2023;29(5):1180–90. These trials demonstrate that dupilumab may be an effective treatment for prurigo nodularis with an acceptable safety profile.
Ständer S, Yosipovitch G, Legat FJ, Lacour JP, Paul C, Narbutt J, et al. Trial of Nemolizumab in Moderate-to-Severe Prurigo Nodularis. N Engl J Med. 2020;382(8):706–16.
• Yin M, Wu R, Chen J, Dou X. Successful treatment of refractory prurigo nodularis with baricitinib. Dermatol Ther [Internet]. 2022. https://doi.org/10.1111/dth.15642. Cited 1 Feb 2024. Baricitinib has been explored as a potential treatment for prurigo nodularis. However findings are based on a case report and not randomized clinical trials.
• Liu T, Chu Y, Wang Y, Zhong X, Yang C, Bai J, et al. Successful treatment of prurigo nodularis with tofacitinib: The experience from a single center. Int J Dermatol [Internet]. 2023. https://doi.org/10.1111/ijd.16568. Cited 1 Feb 2024. The JAK inhibitor tofacitinib may be an experimental treatment option for prurigo nodularis.
Bolognia JL. Dermatology: ExpertConsult. 3rd ed. Edinburgh: Elsevier; 2012.
Szepietowski JC, Reich A, Wiśnicka B. Itching in patients suffering from psoriasis. Acta Dermatovenerol Croat. 2002;10(4):221–6.
Swanbeck G, Inerot A, Martinsson T, Wahlström J. A population genetic study of psoriasis. Br J Dermatol. 1994;131(1):32–9.
McFadden N, Hande KO. A survey of elderly new patients at a dermatology outpatient clinic. Acta Derm Venereol. 1989;69(3):260–2.
Yap KB, Siew MG, Goh CL. Pattern of skin diseases in the elderly seen at the National Skin Centre (Singapore) 1990. Singapore Med J. 1994;35(2):147–50.
Scarpa R, Oriente P, Pucino A, Torella M, Vignone L, Riccio A, et al. Psoriatic arthritis in psoriatic patients. Rheumatology. 1984;23(4):246–50.
Bakshi H, Nagpal M, Singh M, Dhingra GA, Aggarwal G. Treatment of Psoriasis: A Comprehensive Review of Entire Therapies. Curr Drug Saf. 2020;15(2):82–104.
• Lebwohl MG, Stein Gold L, Strober B, Papp KA, Armstrong AW, Bagel J, et al. Phase 3 trials of tapinarof cream for plaque psoriasis. N Engl J Med. 2021;385(24):2219–29. Tapinarof is a newer agent available for long term topical use with excellent Phase 3 data regarding efficacy and safety for the treatment for plaque psoriasis.
• Lebwohl MG, Kircik LH, Moore AY, Stein Gold L, Draelos ZD, Gooderham MJ, et al. Effect of roflumilast cream vs vehicle cream on chronic plaque psoriasis: the DERMIS-1 and DERMIS-2 randomized clinical trials. JAMA. 2022;328(11):1073. Similar to tapinarof, roflumilast cream has also demonstrated excellent efficacy and safety for the topical treatment of chronic plaque psoriasis.
Psoriasis treatment: Biologics [Internet]. Available from: https://www.aad.org/public/diseases/psoriasis/treatment/medications/biologics. Cited 1 Feb 2024.
Sbidian E, Chaimani A, Guelimi R, Garcia-Doval I, Hua C, Hughes C, et al. Systemic pharmacological treatments for chronic plaque psoriasis: a network meta-analysis. Cochrane Database Syst Rev. 2023;7(7):CD011535.
Yosipovitch G, Tang MBY. Practical Management of Psoriasis in the Elderly: Epidemiology, Clinical Aspects, Quality of Life, Patient Education and Treatment Options. Drugs Aging. 2002;19(11):847–63.
Pariser DM, Bagel J, Lebwohl M, Yosipovitch G, Chien E, Spellman MC. Serlopitant for psoriatic pruritus: A phase 2 randomized, double-blind, placebo-controlled clinical trial. J Am Acad Dermatol. 2020;82(6):1314–20.
• Daudén E, De La Cueva P, Salgado-Boquete L, Llamas-Velasco M, Fonseca E, Pau-Charles I, et al. Efficacy and safety of dimethyl fumarate in patients with moderate-to-severe plaque psoriasis: results from a 52-week open-label phase IV clinical trial (DIMESKIN 1). Dermatol Ther (Heidelb). 2023;13(1):329–45. This open label study suggests that Dimethyl Fumarate may significantly improve pruritus symptoms for moderate to severe plaque psoriasis with sustained impact at 52 weeks.
Stein Gold L, Bhatia N, Tallman AM, Rubenstein DS. A phase 2b, randomized clinical trial of tapinarof cream for the treatment of plaque psoriasis: Secondary efficacy and patient-reported outcomes. J Am Acad Dermatol. 2021;84(3):624–31.
Ramachandran V, Bertus B, Bashyam AM, Feldman SR. Treating Psoriasis With Halobetasol Propionate and Tazarotene Combination: A Review of Phase II and III Clinical Trials. Ann Pharmacother. 2020;54(9):872–8.
• Beylot-Barry M, Mahé E, Rolland C, De La Bretèque MA, Eychenne C, Charles J, et al. Evaluation of the benefit of thermal spa therapy in plaque psoriasis: the PSOTHERMES randomized clinical trial. Int J Biometeorol. 2022;66(6):1247–56. This randomized control trial suggests that spa treatment may be beneficial for improving life quality and disease severity among plaque psoriasis patients.
• Sowell J, Pena SM, Elewski BE. Seborrheic dermatitis in older adults: pathogenesis and treatment options. Drugs Aging. 2022;39(5):315–21. In this article, Sowell et al provides an updated review of the pathogenesis and latest management options for SD in older adults.
• Kim H, Yun JW, Baek G, Kim S, Jue MS. Differential microRNA profiles in elderly males with seborrheic dermatitis. Sci Rep. 2022;12(1):21241. Newest research regarding the pathogenesis of SD suggests a potential role of microRNA alterations in disease manifestation.
Gupta A, Bluhm R. Seborrheic dermatitis. Acad Dermatol Venereol. 2004;18(1):13–26.
Cribier Florence Samain. Denis VB (1998) Systematic Cutaneous Examination in Hepatitis C Virus Infected Patients. Acta Dermato Venereologica. 1998;78(5):355–7.
Erics M, Balci S, Atakan N. Dermatological manifestations of 71 Down syndrome children admitted to a clinical genetics unit. Clin Genet. 1996;50(5):317–20.
Maietta G, Fornaro P, Rongioletti F, Rebora A. Patients with mood depression have a high prevalence of seborrhoeic dermatitis. Acta Derm Venereol. 1990;70(5):432–4.
Binder RL, Jonelis FJ. Seborrheic dermatitis in neuroleptic-induced parkinsonism. Arch Dermatol. 1983;119(6):473–5.
Szepietowski JC, Reich A, Wesołowska-Szepietowska E, Baran E, for the National Quality of Life in Dermatology Group. Quality of life in patients suffering from seborrheic dermatitis: influence of age, gender and education level. Mycoses. 2009;52(4):357–63.
Okokon EO, Verbeek JH, Ruotsalainen JH, Ojo OA, Bakhoya VN. Topical antifungals for seborrhoeic dermatitis. In: The Cochrane Collaboration, editor. Cochrane Database of Systematic Reviews [Internet]. Chichester, UK: John Wiley & Sons, Ltd; 2015, p. CD008138.pub2. Available from: https://doi.org/10.1002/14651858.CD008138.pub2. Cited 2 Feb 2024.
Borda LJ, Perper M, Keri JE. Treatment of seborrheic dermatitis: a comprehensive review. J Dermatol Treat. 2019;30(2):158–69.
• Zirwas MJ, Draelos ZD, DuBois J, Kircik LH, Moore AY, Stein Gold L, et al. Efficacy of roflumilast foam, 0.3%, in patients with seborrheic dermatitis: a double-blind, vehicle-controlled phase 2a randomized clinical trial. JAMA Dermatol. 2023;159(6):613. Roflumilast foam demonstrated favorable efficacy and safety profile in this Phase 2 trial and may be a feasible topical treatment for SD and an alternative to topical steroids.
• Azizzadeh M, Pahlevan D, Bagheri B. The efficacy and safety of pimecrolimus 1% cream vs. sertaconazole 2% cream in the treatment of patients with facial seborrhoeic dermatitis: a randomized blinded trial. Clin Experimental Derm. 2022;47(5):926–31. This randomized trial demonstrated that pimecrolimus cream was more efficacious and less irritating than sertaconazole cream for facial SD.
Joly P, Tejedor I, Tetart F, Cailleux HC, Barrel A, De Preville PA, et al. Tacrolimus 0.1% versus ciclopiroxolamine 1% for maintenance therapy in patients with severe facial seborrheic dermatitis: A multicenter, double-blind, randomized controlled study. J Am Acad Dermatol. 2021;84(5):1278–84.
• Wang H, Wang C, Hsieh S, Hung Y, Chen H. Evaluation of a new-formula shampoo containing 6% glycyrrhetinic acid complex for scalp seborrheic dermatitis: A pilot study. J Cosmet Dermatol. 2022;21(8):3423–30. This small pilot study suggests that glycyrrhetinic acid complex shampoo may change bacterial composition of the scalp, reduce symptoms, and improve quality of life among patients with scalp SD.
• Yanfei Z, **aoying N, Dingwei Z, Wei W, Jianwen R. Efficacy and safety of oral isotretinoin in the treatment of moderate to severe seborrheic dermatitis: a retrospective study. Int J Dermatol. 2023;62(6):759–63. This small retrospective study suggests 10mg or 20mg/day of oral isotretinoin may be equally effective in reducing severe seborrheic dermatitis symptoms.
Hu YB, Song XZ. Successful treatment with oral hydroxychloroquine of seborrhoeic dermatitis in a patient with AIDS. Clin Exp Dermatol. 2021;46(3):567–8.
Cohen SR, Gordon SC, Lam AH, Rosmarin D. Recalcitrant Seborrheic Dermatitis Successfully Treated With Apremilast. J Cutan Med Surg. 2020;24(1):90–1.
Grover RW. Transient Acantholytic Dermatosis. Arch Dermatol. 1970;101(4):426.
French LE, Piletta PA, Etienne A, Salomon D, Saurat JH. Incidence of transient acantholytic dermatosis (Grover’s disease) in a hospital setting. Dermatology. 1999;198(4):410–1.
Simon RS. Persistent Acantholytic Dermatosis: A Variant of Transient Acantholytic Dermatosis (Grover Disease). Arch Dermatol. 1976;112(10):1429.
Grover RW, Rosenbaum R. The association of transient acantholytic dermatosis with other skin diseases. J Am Acad Dermatol. 1984;11(2):253–6.
Moon HR, Lee JH, Rhee DY, Won CH, Chang SE, Lee MW, et al. Grover’s Disease in a Liver Transplant Patient. Ann Dermatol. 2014;26(1):117.
Rodríguez-Pazos L, Vilas-Sueiro A, González-Vilas D, Durana C. Enfermedad de Grover en fracaso renal crónico. Nefrologia. 2015;35(3):331–4.
Khan MS, Khan M, Aivaz O. Transient acantholytic dermatosis in a patient with prostate cancer. Dermatol Online J. 2020;26(2):13030/qt02s0n1zr.
Beer J, Rosenbach M. Grover Disease Associated With Chemotherapy: Review of Potential Pathophysiology, Current Treatments, and Future Directions. JDD. 2020;19(11):1056–64.
Bellinato F, Maurelli M, Gisondi P, Girolomoni G. Clinical features and treatments of transient acantholytic dermatosis (Grover’s disease): a systematic review. J Deutsche Derma Gesell. 2020;18(8):826–33.
Mota AV, Correia TM, Lopes JM, Guimarães JM. Successful treatment of Grover’s disease with calcipotriol. Eur J Dermatol. 1998;8(1):33–5.
Helfman RJ. Grover’s disease treated with isotretinoin. J Am Acad Dermatol. 1985;12(6):981–4.
Breuckmann F, Appelhans C, Altmeyer P, Kreuter A. Medium-dose ultraviolet al phototherapy in transient acantholytic dermatosis (Grover’s disease). J Am Acad Dermatol. 2005;52(1):169–70.
Galamgam J, Lee DJ. Treatment of transient acantholytic dermatosis with liquid nitrogen. JAAD Case Reports. 2020;6(4):341–3.
Butler DC, Kollhoff A, Berger T. Treatment of Grover Disease With Dupilumab. JAMA Dermatol. 2021;157(3):353.
Takahagi S, Ashizawa S, Tanaka A, Hide M. Grover’s disease successfully treated with calcipotriene/betamethasone dipropionate ointment. Dermatol Ther [Internet]. 2020. https://doi.org/10.1111/dth.14217. Cited 1 Feb 2024.
Renz P, Hasan S, English JC, Wegner RE, Jedrych J, Ho J, et al. Grover’s Disease Treated With Total Skin Electron Beam Radiotherapy. J Drugs Dermatol. 2019;18(4):392–3.
• Hrin ML, Patel PV, Jorizzo JL, Feldman SR, Huang WW. Methotrexate versus acitretin for Grover’s disease refractory to topical therapies. J Cutan Med Surg. 2023;22:12034754231211568. This very small retrospective study suggests methotrexate and acitretin may help with Grover's disease. However, this study has several weaknesses including a small sample size, non-standardized outcomes, and use of concomitant treatments.
Mills KT, Xu Y, Zhang W, Bundy JD, Chen CS, Kelly TN, et al. A systematic analysis of worldwide population-based data on the global burden of chronic kidney disease in 2010. Kidney Int. 2015;88(5):950–7.
Verduzco HA, Shirazian S. CKD-Associated Pruritus: New Insights Into Diagnosis, Pathogenesis, and Management. Kidney International Reports. 2020;5(9):1387–402.
• Agarwal P, Garg V, Karagaiah P, Szepietowski JC, Grabbe S, Goldust M. Chronic kidney disease-associated pruritus. Toxins. 2021;13(8):527. Since chronic kidney disease is a common comorbidity among older adults, this article is helpful to remain informed regarding its pathogenesis, cutaneous manifestations, and management.
Mathur VS, Lindberg J, Germain M, Block G, Tumlin J, Smith M, et al. A Longitudinal Study of Uremic Pruritus in Hemodialysis Patients. Clin J Am Soc Nephrol. 2010;5(8):1410–9.
Rayner HC, Larkina M, Wang M, Graham-Brown M, Van Der Veer SN, Ecder T, et al. International Comparisons of Prevalence, Awareness, and Treatment of Pruritus in People on Hemodialysis. CJASN. 2017;12(12):2000–7.
Sukul N, Karaboyas A, Csomor PA, Schaufler T, Wen W, Menzaghi F, et al. Self-reported Pruritus and Clinical, Dialysis-Related, and Patient-Reported Outcomes in Hemodialysis Patients. Kidney Medicine. 2021;3(1):42-53.e1.
Bencini PL, Montagnino G, Citterio A, Graziani G, Crosti C, Ponticelli C. Cutaneous Abnormalities in Uremic Patients. Nephron. 1985;40(3):316–21.
Chou FF, Ho JC, Huang SC, Sheen-Chen SM. A study on pruritus after parathyroidectomy for secondary hyperparathyroidism1. J Am Coll Surg. 2000;190(1):65–70.
Simonsen E, Komenda P, Lerner B, Askin N, Bohm C, Shaw J, et al. Treatment of Uremic Pruritus: A Systematic Review. Am J Kidney Dis. 2017;70(5):638–55.
•• Topf J, Wooldridge T, McCafferty K, Schömig M, Csiky B, Zwiech R, et al. Efficacy of difelikefalin for the treatment of moderate to severe pruritus in hemodialysis patients: pooled analysis of KALM-1 and KALM-2 phase 3 studies. Kidney Med. 2022;4(8):100512. Analysis of a large cohort of diverse patients from two Phase 3 studies suggests Difelikefalin can rapidly improve pruritus symptoms for dialysis patients.
• Wala K, Szepietowski JC. Difelikefalin in the treatment of chronic kidney disease-associated pruritus: a systematic review. Pharmaceuticals. 2022;15(8):934. Systematic review providing further evidence of the efficacy of Difelikefalin for CKD-associated pruritus.
Hawi A, Alcorn H, Berg J, Hines C, Hait H, Sciascia T. Pharmacokinetics of nalbuphine hydrochloride extended release tablets in hemodialysis patients with exploratory effect on pruritus. BMC Nephrol. 2015;16(1):47.
• Zhang P, **ang S, Liu B, Wang X, Yang X, Ye C, et al. Randomized controlled trial of nalfurafine for refractory pruritus in hemodialysis patients. Ren Fail. 2023;45(1):2175590. This study suggests nalfurafine may be used for refractory pruritus in hemodialysis patients although the rate of adverse drug reactions was high.
Gholyaf M, Sheikh V, Yasrebifar F, Mohammadi Y, Mirjalili M, Mehrpooya M. Effect of mirtazapine on pruritus in patients on hemodialysis: a cross-over pilot study. Int Urol Nephrol. 2020;52(6):1155–65.
Rehman IU, Ahmed R, Rahman AU, Wu DBC, Munib S, Shah Y, et al. Effectiveness and safety profiling of zolpidem and acupressure in CKD associated pruritus: An interventional study. Medicine. 2021;100(21): e25995.
Bunchorntavakul C, Reddy KR. Pruritus in Chronic Cholestatic Liver Disease. Clin Liver Dis. 2012;16(2):331–46.
• Nietsche TR, Dotta G, Barcaui CB, Ferraz MLCG. Cholestatic pruritus: a knowledge update. An Bras Dermatol. 2022;97(3):332–7. Cholestatic disease associated pruritus is another common etiology of pruritus in the older adult with need for current understanding of diagnostic approach and management.
Kremer AE, Martens JJWW, Kulik W, Ruëff F, Kuiper EMM, Van Buuren HR, et al. Lysophosphatidic Acid Is a Potential Mediator of Cholestatic Pruritus. Gastroenterology. 2010;139(3):1008-1018.e1.
** XY, Khan TM. Quality of life among patients suffering from cholestatic liver disease-induced pruritus: A systematic review. J Formos Med Assoc. 2016;115(9):689–702.
Kremer AE, Beuers U, Oude-Elferink RPJ, Pusl T. Pathogenesis and Treatment of Pruritus in Cholestasis: Drugs. 2008;68(15):2163–82.
• Loomes KM, Squires RH, Kelly D, Rajwal S, Soufi N, Lachaux A, et al. Maralixibat for the treatment of PFIC: Long-term, IBAT inhibition in an open-label, Phase 2 study. Hepatol Commun. 2022;6(9):2379–90. Maralixibat may be used for the treatment of progressive familial intrahepatic cholestasis however, treatment response seems to dependent on the specific disease subtype.
Mayo MJ, Pockros PJ, Jones D, Bowlus CL, Levy C, Patanwala I, et al. A Randomized, Controlled, Phase 2 Study of Maralixibat in the Treatment of Itching Associated With Primary Biliary Cholangitis. Hepatol Commun. 2019;3(3):365–81.
Hirschfield GM, Beuers U, Corpechot C, Invernizzi P, Jones D, Marzioni M, et al. EASL Clinical Practice Guidelines: The diagnosis and management of patients with primary biliary cholangitis. J Hepatol. 2017;67(1):145–72.
• Chovatiya R, Brieva J, Hung A. Dupilumab treatment for cholestatic pruritus. Dermatol Ther [Internet]. 2022. https://doi.org/10.1111/dth.15296. Cited 2 Feb 2024. This case study suggests dupilumab may have a role in treating cholestatic pruritus although additional high-quality evidence is lacking.
Yosipovitch G. Chronic pruritus: a paraneoplastic sign: Chronic pruritus. Dermatol Ther. 2010;23(6):590–6.
Siegel FP, Tauscher J, Petrides PE. Aquagenic pruritus in polycythemia vera: Characteristics and influence on quality of life in 441 patients. American J Hematol. 2013;88(8):665–9.
Kılıç A, Gül Ü, Soylu S. Skin findings in internal malignant diseases. Int J Dermatology. 2007;46(10):1055–60.
Rowe B, Yosipovitch G. Malignancy-associated pruritus. Eur J Pain. 2016;20(1):19–23.
Vannucchi AM, Antonioli E, Guglielmelli P, Rambaldi A, Barosi G, Marchioli R, et al. Clinical profile of homozygous JAK2 617V>F mutation in patients with polycythemia vera or essential thrombocythemia. Blood. 2007;110(3):840–6.
Wang H, Yosipovitch G. New insights into the pathophysiology and treatment of chronic itch in patients with end-stage renal disease, chronic liver disease, and lymphoma. Int J Dermatology. 2010;49(1):1–11.
Etter L, Myers SA. Pruritus in systemic disease: mechanisms and management. Dermatol Clin. 2002;20(3):459–72.
Dawn AG, Yosipovitch G. Butorphanol for treatment of intractable pruritus. J Am Acad Dermatol. 2006;54(3):527–31.
Demierre MF, Taverna J. Mirtazapine and gabapentin for reducing pruritus in cutaneous T-cell lymphoma. J Am Acad Dermatol. 2006;55(3):543–4.
Cedeno-Laurent F, Singer EM, Wysocka M, Benoit BM, Vittorio CC, Kim EJ, et al. Improved pruritus correlates with lower levels of IL-31 in CTCL patients under different therapeutic modalities. Clin Immunol. 2015;158(1):1–7.
Saini KS, Patnaik MM, Tefferi A. Polycythemia vera-associated pruritus and its management. Eur J Clin Investigation. 2010;40(9):828–34.
• Koschmieder S, Isfort S, Wolf D, Heidel FH, Hochhaus A, Schafhausen P, et al. Efficacy and safety of ruxolitinib in patients with newly-diagnosed polycythemia vera: futility analysis of the RuxoBEAT clinical trial of the GSG-MPN study group. Ann Hematol. 2023;102(2):349–58. Ruxolitinib may be useful in treating patients with polycythemia vera and improve quality of life. However, rate of drug related adverse events were reported to be very high.
• Wachuku CI, Barrera T, Jackson T, Sow Y, Mollanazar N, Taylor SC. Upadacitinib as a treatment for chronic pruritus secondary to polycythemia vera after failure with dupilumab. JAAD Case Rep. 2023;35:87–9. This case report suggests that another JAK inhibitor Upadacitinib may be helpful in treating pruritus secondary to polycythemia vera among those who have not responded to dupilumab.
Carstens E, Akiyama T. Itch: mechanisms and treatment [Internet]. Boca Raton, Florida; CRC Press, 2014. Available from: https://catalog.lib.unc.edu/catalog/UNCb7711583.
Rosen JD, Fostini AC, Yosipovitch G. Diagnosis and Management of Neuropathic Itch. Dermatol Clin. 2018;36(3):213–24.
• Keenan M. Pharmacotherapeutics of aprepitant and pregabalin in neuropathic pain and refractory pruritus in a patient diagnosed with a cutaneous T-cell lymphoma. J Prescr Pract. 2022;4(8):362–7. This case report suggests aprepitant and pregabalin may be used in refractory pruritus. However, these treatments may not be appropriate for all patients given the extensive drug side effects.
• Lou K, Murphy S, Talbot C. Cannabinoids for the treatment of refractory neuropathic pruritus in amyotrophic lateral sclerosis: a case report. Palliat Med. 2022;36(1):208–11. This case report suggests cannabinoids may help with refractory pruritus in ALS patients. However, standardized response measures are lacking and further high quality research is needed to establish true efficacy.
• Kwatra SG, Kambala A, Cornman H, Reddy SV, Cohen SP. Ketamine infusions for treatment-resistant neuropathic pruritus. JAMA Dermatol. 2023;159(9):1011. This case report suggests Ketamine infusions can provide prolonged relief from neuropathic pruritus. However, this treatment may not be feasible for many due to lack of insurance coverage and need for multiple infusions at high doses.
Portugal DM, Ferreira EF, Camões-Barbosa A. Botulinum toxin type A therapy for bilateral focal neuropathic pruritus in multiple sclerosis: a case report. Int J Rehabil Res. 2021;44(4):382–3.
Abel MK, Ashbaugh AG, Stone HF, Murase JE. The use of dupilumab for the treatment of recalcitrant brachioradial pruritus. JAAD Case Reports. 2021;10:69–71.
Buteau A, Reichenberg J. Psychogenic Pruritus and Its Management. Dermatol Clin. 2018;36(3):309–14.
Allan CE, Valkanova V, Ebmeier KP. Depression in older people is underdiagnosed. Practitioner. 2014;258(1771):19–22, 2–3.
Weisshaar E, Szepietowski J, Darsow U, Misery L, Wallengren J, Mettang T, et al. European Guideline on Chronic Pruritus. Acta Derm Venerol. 2012;92(5):563–81.
Mazeh D, Melamed Y, Cholostoy A, Aharonovitzch V, Weizman A, Yosipovitch G. Itching in the Psychiatric Ward. Acta Derm Venereol. 2008;88(2):128–31.
Kretzmer GE, Gelkopf M, Kretzmer G, Melamed Y. Idiopathic pruritus in psychiatric inpatients: an explorative study. Gen Hosp Psychiatry. 2008;30(4):344–8.
• Hwang AS, Campbell EH, Sartori-Valinotti JC. Evidence of N-acetylcysteine efficacy for skin picking disorder: a retrospective cohort study. J Am Acad Dermatol. 2022;87(1):148–50. This small retrospective cohort study suggests N-acetylcysteine may help with skin picking disorder. However, the sample size was small, the majority of participants were women, and positive response occurred for only about 60% of patients.
Grant JE, Chamberlain SR, Redden SA, Leppink EW, Odlaug BL, Kim SW. N -Acetylcysteine in the Treatment of Excoriation Disorder: A Randomized Clinical Trial. JAMA Psychiat. 2016;73(5):490.
Reich A, Ständer S, Szepietowski J. Drug-induced Pruritus: A Review. Acta Derm Venerol. 2009;89(3):236–44.
Halli-Tierney AD, Scarbrough C, Carroll D. Polypharmacy: Evaluating Risks and Deprescribing. Am Fam Physician. 2019;100(1):32–8.
Huang AH, Kaffenberger BH, Reich A, Szepietowski JC, Ständer S, Kwatra SG. Pruritus Associated with Commonly Prescribed Medications in a Tertiary Care Center. Medicines. 2019;6(3):84.
• Zhou T, Zhang Y, Ma Y, Ma W, Wu X, Huang L, et al. Comparison of aprepitant versus desloratadine for EGFR-TKI-induced pruritus: a randomized phase 2 clinical trial. Cancer. 2022;128(22):3969–76. This randomized trial indicates aprepitant may be superior to desloratadine for epidermal growth factor receptor-tyrosine kinase inhibitors-induced pruritus due to shorter response time and mild side effects.
• Nguyen E, Lim G, Ross SE. Evaluation of therapies for peripheral and neuraxial opioid-induced pruritus based on molecular and cellular discoveries. Anesthesiology. 2021;135(2):350–65. Opioids are commonly prescribed medications in the elderly. This review highlights the most recent discoveries in understanding the pathomechanisms of opioid-induced pruritus and the newest treatments being evaluated for its management.
Clerc C, Misery L. A Literature Review of Senile Pruritus: From Diagnosis to Treatment. Acta Derm Venerol. 2017;97(4):433–40.
•• Chen S, Zhou F, **ong Y. Prevalence and risk factors of senile pruritus: a systematic review and meta-analysis. BMJ Open. 2022;12(2):e051694. This systematic review and pooled analysis indicates a high prevalence of senile pruritus and highlights potential risk factors.
Namer B. Age related changes in human C-fiber function. Neurosci Lett. 2010;470(3):185–7.
Ma X, Lu L, Zhao Z, Cai M, Gao N, Han G. Lipidomics profiling of skin surface lipids in senile pruritus. Lipids Health Dis. 2020;19(1):171.
Huang Y, Liu J, Zhang X, Li Y, Xu Y, **ong X, et al. Patients with senile pruritus have a distinct skin microbiota and epidermal barrier in comparison with healthy controls. J Dermatol. 2021;48(12):1892–9.
Du X, Chen S, Zhang X, Chen D, Wang C, **ang M. Effect of behavioral intervention on scratching behavior in patients with senile pruritus. Chinese Journal of Behavioral Medicine and Brain Science. 2020;148–52.
Lacarrubba F, Verzì AE, Dinotta F, Micali G. 10% urea cream in senile xerosis: Clinical and instrumental evaluation. J of Cosmetic Dermatology. 2021;20(S1):5–8.
Yahya YF, Vani O, Putra DE, Sovianti CS, Trislinawati D, Marina T, Riviati N, et al. The Efficacy and Safety of Plant Oil Mixtures in the Treatment of Xerosis with Pruritus in Elderly People: Randomized double blind Controlled Trial. Bioscmed. 2020;5(3):255–62.
Baricitinib rapidly relieves senile pruritus without significant adverse effects: 2 cases - 프로그램북(구 초록집) - 대한피부과학회 - KISS [Internet]. Available from: https://kiss.kstudy.com/Detail/Ar?key=3942515. Cited 2 Feb 2024.
Ostlere LS, Taylor CR, Harris DWS, Rustin MHA, Wright S, Johnson M. Skin surface lipids in HIV-positive patients with and without seborrheic dermatitis. Int J Dermatology. 1996;35(4):276–9.
Papp K, Szepietowski JC, Kircik L, Toth D, Eichenfield LF, Leung DYM, et al. Efficacy and safety of ruxolitinib cream for the treatment of atopic dermatitis: Results from 2 phase 3, randomized, double-blind studies. J Am Acad Dermatol. 2021;85(4):863–72.
Reich K, Kabashima K, Peris K, Silverberg JI, Eichenfield LF, Bieber T, et al. Efficacy and Safety of Baricitinib Combined With Topical Corticosteroids for Treatment of Moderate to Severe Atopic Dermatitis: A Randomized Clinical Trial. JAMA Dermatol. 2020;156(12):1333.
• Zareie E, Mansouri P, Hosseini H, Sadeghpour O, Shirbeigi L, Hejazi S, et al. Effect of oral administration of Triphala, a polyphenol-rich prebiotic, on scalp sebum in patients with scalp seborrhea a randomized clinical trial. J Dermatol Treat. 2022;33(2):1011–6. This small randomized trial demonstrates Triphala may improve scalp sebum levels although strength of results is limited by small sample size and wide confidence intervals.
Funding
None.
Author information
Authors and Affiliations
Contributions
RBS performed the literature review and drafted the manuscript. MBL and CJS critically reviewed the manuscript and provided their clinical expertise and input. All authors contributed substantially to the manuscript.
Corresponding author
Ethics declarations
Conflicts of Interest
RBS and MBL report no conflict of interests. CJS reports being an investigator for AbbVie, ChemoCentryx, Incyte, InflaRx, Novartis and UCB Pharma; consultancy fees from AbbVie, Alumis, Astrazeneca, InflaRx, Sandoz, Incyte, Logical Images, Sonoma Biotherapeutics and UCB Pharma; speaker for AbbVie and Novartis. CJS also reports being a section editor for the Dermatology and Wound Care section of Current Geriatrics Report 2024 volume.
Human/Animal Studies Informed Consent Statement
This article does not contain any studies with human or animal subjects performed by any of the authors.
IRB Approval Status
IRB not required.
Patient Consent
Not required.
Reprint Requests
Chris J. Sayed, MD.
Disclaimer
We certify that the figure and table provided in this manuscript are original. They have been drafted and edited by all authors of this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shams, R.B., Lipner, M.B. & Sayed, C.J. Title: Pruritus in the Elderly: Differential Diagnosis and Management. Curr Geri Rep (2024). https://doi.org/10.1007/s13670-024-00418-7
Accepted:
Published:
DOI: https://doi.org/10.1007/s13670-024-00418-7