Abstract
The study focused on formulation of carmellose sodium hydrogels and nonionic microemulsions with 5% and 10% of levetiracetam and investigation of drug concentration influence on their physicochemical characteristics and in-use stability as well as influence of drug concentration and carrier type on in vitro drug release and in vivo antihyperalgesic/antiedematous activity in a rat model of localized (intraplantar) carrageenan-induced inflammation. Hydrogels were pseudoplastic semisolids with thixotropy and pH 7.37–7.58. Microemulsions were low viscous Newtonian nanodispersions of oil droplets (13.11–15.11 nm) in water, with pH 4.01–4.64. Physical stability of the investigated systems was preserved over the 3-month storage under ambient conditions. Levetiracetam release followed zero order and Korsmeyer-Peppas models (R2 ≥ 0.99) reflecting the combined effects of drug concentration and carrier viscosity. All levetiracetam-loaded formulations produced significant reduction of hyperalgesia and paw swelling induced by carrageenan (p < 0.001). Their efficacy in exerting antihyperalgesic activity was significantly higher than that observed with the reference 5% ibuprofen hydrogel preparation (up to 6 h) (p < 0.001), while antiedematous activity was comparable with the reference product. No erythema and visible blood vessels were observed in a rat ear test. The study demonstrated percutaneous delivery of levetiracetam as useful and safe therapeutic option for localized inflammatory pain with potential to overcome the insufficient efficacy of topically applied nonsteroidal anti-inflammatory drugs in the form of a hydrogel.

Graphical abstract




Similar content being viewed by others
References
Tomić M, Pecikoza U, Micov A, Vučković S, Stepanović-Petrović R. Antiepileptic drugs as analgesics/adjuvants in inflammatory pain: current preclinical evidence. Pharmacol Ther. 2018;192:42–64.
Wiffen PJ, Derry S, Moore RA, Aldington D, Cole P, Rice AS, et al. Antiepileptic drugs for neuropathic pain and fibromyalgia-an overview of Cochrane reviews. Cochrane Database Syst Rev. 2013;11:CD010567.
Argoff CE. Topical analgesics in the management of acute and chronic pain. Mayo Clin Proc. 2013;88:195–205.
Derry S, Wiffen PJ, Kalso EA, Bell RF, Aldington D, Phillips T, et al. Topical analgesics for acute and chronic pain in adults-an overview of Cochrane Reviews. Cochrane Database Syst Rev. 2017;5:CD008609.
Ali G, Subhan F, Abbas M, Zeb J, Shahid M, Sewell RD. A streptozotocin-induced diabetic neuropathic pain model for static or dynamic mechanical allodynia and vulvodynia: validation using topical and systemic gabapentin. Naunyn Schmiedeberg's Arch Pharmacol. 2015;388:1129–40.
Hiom S, Khot S, Mogford S, Hart C, Patel G, Roberts G, et al. Topical delivery of gabapentin (Gaba Gel™) for neuropathic pain: a ‘proof of concept’ study. Int J Pharm Pract. 2015;23(S2):46.
Shahid M, Subhan F, Ahmad N, Ali G, Akbar S, Fawad K, et al. Topical gabapentin gel alleviates allodynia and hyperalgesia in the chronic sciatic nerve constriction injury neuropathic pain model. Eur J Pain. 2017;21:668–80.
Stepanović-Petrović RM, Micov AM, Tomić MA, Ugrešić ND. The local peripheral antihyperalgesic effect of levetiracetam and its mechanism of action in an inflammatory pain model. Anesth Analg. 2012;115:1457–66.
Rannou F, Pelletier JP, Martel-Pelletier J. Efficacy and safety of topical NSAIDs in the management of osteoarthritis: evidence from real-life setting trials and surveys. Semin Arthritis Rheum. 2016;45(4 Suppl):S18–21.
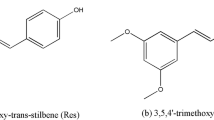
Hu X-B, Kang R-R, Tang T-T, Li Y-J, Wu J-Y, Wang J-M, et al. Topical delivery of 3,5,4′-trimethoxy-trans-stilbene-loaded microemulsion-based hydrogel for the treatment of osteoarthritis in a rabbit model. Drug Deliv Transl Res. 2019;9(1):357–65.
Rachmawati H, Arvin YA, Asyarie S, Anggadiredja K, Tjandrawinata RR, Storm G. Local sustained delivery of bupivacaine HCl from a new castor oil-based nanoemulsion system. Drug Deliv Transl Res. 2018;8(3):515–24.
Bayer GG. Martindale: the complete drug reference. 38th ed. London: Pharmaceutical Press; 2014.
Petruševska M, Berglez S, Krisch I, Legen I, Megusar K, Peternel L, et al. Biowiver monograph biowaiver monographs for immediate release solid oral dosage forms: levetiracetam. J Pharm Sci. 2015;104:2676–87.
Wiedersberg S, Guy RH. Transdermal drug delivery: 30+ years of war and still fighting! J Control Release. 2014;190:150–6.
Aghazadeh-Habashi A, Yang Y, Tang K, Lőbenberg R, Doschak MR. Transdermal drug delivery: feasibility for treatment of superficial bone stress fractures. Drug Deliv Transl Res. 2015;5(6):540–51.
Ahmed EM. Hydrogel: preparation, characterization, and applications. A review. J Adv Res. 2015;6(2):105–21.
Rowe RC, Sheskey PJ, Quinn ME. Handbook of pharmaceutical excipients. 6th ed. London: Pharmaceutical Press; 2009.
Hosny KM, Tayeb MM, Fallatah OM, Mahmoud AA, Mandoura MS, Al-Sawahli MM. Preparation and evaluation of ketorolac tromethamine hydrogel. Int J Pharm Sci Rev Res. 2013;20(2):269–74.
Barbucci R, Leone G, Vecchiullo A. Novel carboxymethylcellulose-based microporous hydrogels suitable for drug delivery. J Biomater Sci Polym Ed. 2004;15(5):607–19.
Djekic L, Martinović M, Dobričić V, Čalija B, Medarević Đ, Primorac M. Comparison of the effect of bioadhesive polymers on stability and drug release kinetics of biocompatible hydrogels for topical application of ibuprofen. J Pharm Sci. 2019;108:1326–33.
Djekic L, Primorac M. Microemulsion systems–application in delivery of poorly soluble drugs. In: Fanun M, editor. Colloids in Drug Delivery. Boca Raton: Taylor & Francis Group, CRC Press; 2010. p. 245–70.
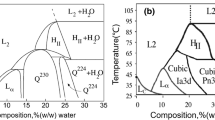
Djekic L, Primorac M, Jocković J. Phase behaviour, microstructure and ibuprofen solubilization capacity of pseudo-ternary nonionic microemulsions. J Mol Liq. 2011;160:81–7.
Djekic L, Martinovic M, Stepanović-Petrović R, Micov A, Tomić M, Primorac M. Formulation of hydrogel-thickened nonionic microemulsions with enhanced percutaneous delivery of ibuprofen assessed in vivo in rats. Eur J Pharm Sci. 2016;92:255–65.
Djekic L, Martinovic M, Stepanović-Petrović R, Tomić M, Micov A, Primorac M. Design of block copolymer costabilized nonionic microemulsions and their in vitro and in vivo assessment as carriers for sustained regional delivery of ibuprofen via topical administration. J Pharm Sci. 2015;104(8):2501–12.
Djekic L, Primorac M, Filipic S, Agbaba D. Investigation of surfactant/cosurfactant synergism impact on ibuprofen solubilization capacity and drug release characteristics of nonionic microemulsions. Int J Pharm. 2012;433:25–33.
Grassi M, Lamberti G, Cascone S, Grassi G. Mathematical modeling of simultaneous drug release and in vivo absorption. Int J Pharm. 2011;418:130–41.
Rao LA, Jahnavi NV. A validated RP-HPLC method for the estimation of levetiracetam in bulk and pharmaceutical formulations. E J Chem. 2010;7:600–4.
Mangelings D, Saevels J, Heyden V. Enantiomeric impurity determination of levetiracetam using capillary electrochromatography. J Sep Sci. 2006;26:2827–36.
Bowman BJ, Ofner CM III, Schott H. Colloidal dispersions. In: Troy D, editor. Remington: the science and practice of pharmacy. 21st ed. Philadelphia: Lippincott Williams & Wilkins; 2005. p. 293–318.
Baumgartner S, Kristl J, Peppas NA. Network structure of cellulose ethers used in pharmaceutical applications during swelling and at equilibrium. Pharm Res. 2002;19(8):1084–90.
Michailova V, Titeva S, Kotsilkova R, Krusteva E, Minkov E. Influence of aqueous medium on viscoelastic properties of carboxymethylcellulose sodium, hydroxypropylmethyl cellulose, and thermally pre-gelatinized starch gels. Colloids Surf A Physicochem Eng Asp. 1999;149(1–3):515–20.
All SM, Yosipovitch G. Skin pH: from basic science to basic skin care. Acta Derm Venereol. 2013;93:261–7.
Blanco MD, Olmo RM, Teijón JM. Hydrogels. In: Swarbrick J, editor. Encyclopedia of pharmaceutical technology, vol. 3. 3rd ed. New York: Informa Healthcare; 2007. p. 2021–39.
Salome CA, Godswill O, Ikechukwu OI. Kinetics and mechanisms of drug release from swellable and non swellable matrices: a review. Res J Pharm Biol Chem Sci. 2013;4(2):97–103.
Szymańska E, Czajkowska-Kośnik A, Winnicka K. Comparison of rheological, drug release, and mucoadhesive characteristics upon storage between hydrogels with unmodified or beta-glycerophosphate-crosslinked chitosan. Int J Polym Sci. 2018:12. https://doi.org/10.1155/2018/3592843.
Micov A, Tomić M, Popović B, Stepanović-Petrović R. The antihyperalgesic effect of levetiracetam in an inflammatory model of pain in rats: mechanism of action. Br J Pharmacol. 2010;161:384–92.
Haghikia A, Ladage K, Hinkerohe D, Vollmar P, Heupel K, Dermietzel R, et al. Implications of antiinflammatory properties of the anticonvulsant drug levetiracetam in astrocytes. J Neurosci Res. 2008;86:1781–8.
Mohammad HMF, Sami MM, Makary S, Toraih EA, Mohamed AO, El-Ghaiesh SH. Neuroprotective effect of levetiracetam in mouse diabetic retinopathy: effect on glucose transporter-1 and GAP43 expression. Life Sci. 2019;232:116588.
Abed El-Gaphar OAM, Abo-Youssef AM, Halal GK. Levetiracetam mitigates lipopolysaccharide-induced JAK2/STAT3 and TLR4/MAPK signaling pathways activation in a rat model of adjuvant-induced arthritis. Eur J Pharmacol. 2018;826:85–95.
Mbizvo GK, Dixon P, Hutton JL, Marson AG. The adverse effects profile of levetiracetam in epilepsy: a more detailed look. Int J Neurosci. 2014;124:627–34.
Uttley M, van Abbé NJ. Primary irritation of the skin: mouse ear test and human patch test procedures. J Soc Cosmet Chem. 1973;24:217–27.
Acknowledgments
The authors acknowledge a levetiracetam sample from Hemofarm A.D./Stada Grupa (Serbia).
Author contribution statement
Radica Stepanović-Petrović and Ljiljana Djekic contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Ljiljana Djekic, Bojan Marković, Ana Micov, Maja Tomić, Uroš Pecikoza, and Radica Stepanović-Petrović. All authors drafted the manuscript and commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
This work was supported by the Ministry of Education, Science and Technological Development of the Republic of Serbia (grant numbers III46010, OI175045).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics statement
All institutional and national guidelines for the care and use of laboratory animals were followed. All data generated or analyzed during this study are included in this published article.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Djekic, L., Marković, B., Micov, A. et al. Percutaneous delivery of levetiracetam as an alternative to topical nonsteroidal anti-inflammatory drugs: formulation development, in vitro and in vivo characterization. Drug Deliv. and Transl. Res. 11, 227–241 (2021). https://doi.org/10.1007/s13346-020-00787-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13346-020-00787-4