Abstract
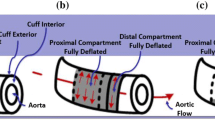
Mechanical circulatory support (MCS) devices have become a standard therapy for heart failure (HF) patients. MCS device designs may differ by level of support, inflow and/or outflow cannulation sites, and mechanism(s) of cardiac unloading and blood flow delivery. Investigation and direct comparison of hemodynamic parameters that help characterize performance of MCS devices has been limited. We quantified cardiac and vascular hemodynamic responses for different types of MCS devices. Continuous flow (CF) left ventricular (LV) assist devices (LVAD) with LV or left atrial (LA) inlet, counterpulsation devices, percutaneous CF LVAD, and intra-aortic rotary blood pumps (IARBP) were quantified using established computer simulation and mock flow loop models. Hemodynamic data were analyzed on a beat-to-beat basis at baseline HF and over a range of MCS support. Results demonstrated that all LVAD greatly diminished vascular pulsatility (P) and LV external work (LVEW). LVAD with LA inflow provided a greater reduction in LVEW compared to LVAD with LV inflow, but at the potential risk for blood stasis/thrombosis in the LV at high support. Counterpulsation provided greater coronary flow (CoF) augmentation, but had a lower reduction in LVEW compared to partial percutaneous LVAD support. IARBP diminished LVEW, but at the expense of diminished CoF due to coronary steal. The hemodynamic benefits for each type of mechanical circulatory support system are unique and clinical decisions on device selection to maximize end organ perfusion and minimize invasiveness needs to be considered for an individual patients’ presentation.






Similar content being viewed by others
References
Bartoli, C. R., et al. A novel subcutaneous counterpulsation device: acute hemodynamic efficacy during pharmacologically induced hypertension, hypotension, and heart failure. Artif. Organs 34:537–545, 2010.
Bresson, D., et al. Preliminary experience with Impella recover LP5.0 in nine patients with cardiogenic shock: a new circulatory support system in the intensive cardiac care unit. Arch. Cardiovasc. Dis. 104:458–464, 2011.
Cheng, A., C. A. Williamitis, and M. S. Slaughter. Comparison of continuous-flow and pulsatile-flow left ventricular assist devices: is there an advantage to pulsatility? Ann. Cardiothorac. Surg. 3:573–581, 2014.
Copeland, III, J. G., et al. Comparison of the CardioWest total artificial heart, the Novacor left ventricular assist system and the Thoratec ventricular assist system in bridge to transplantation. Ann. Thorac. Surg. 71:S92–S97, 2001.
Dekker, A., et al. Efficacy of a new intraaortic propeller pump vs the intraaortic balloon pump: an animal study. Chest 123:2089–2095, 2003.
Engström, A. E., et al. The Impella 2.5 and 5.0 devices for ST-elevation myocardial infarction patients presenting with severe and profound cardiogenic shock: the academic medical center intensive care unit experience. Crit. Care Med. 39:2072–2079, 2011.
Giridharan, G. A., and M. Skliar. Nonlinear controller for ventricular assist devices. Artif. Organs. 26:980–984, 2002.
Giridharan, G. A., and M. Skliar. Control strategy for maintaining physiological perfusion with rotary blood pumps. Artif. Organs. 27:639–648, 2003.
Giridharan, G. A., et al. Modeling and control of a brushless DC axial flow ventricular assist device. ASAIO J. 48:272–289, 2002.
Giridharan, G. A., et al. Predicted hemodynamic benefits of counterpulsation therapy using a superficial surgical approach. ASAIO J. 52:39–46, 2006.
Giridharan, G. A., et al. Miniaturization of mechanical circulatory support systems. Artif. Organs 36:731–739, 2012.
Giridharan, G. A., et al. Control strategies for afterload reduction with an artificial vasculature device. ASAIO J. 58:353–362, 2012.
Giridharan, G. A., et al. Hemodynamic changes and retrograde flow in LVAD failure. ASAIO J. 61:282–291, 2015.
Grabellus, F., et al. Reduction of hypoxia-inducible heme oxygenase-1 in the myocardium after left ventricular mechanical support. J Pathol. 197:230–237, 2002.
Ising, M. S., et al. Flow modulation algorithms for continuous flow left ventricular assist devices to increase vascular pulsatility: a computer simulation study. Cardiovasc. Eng. Technol. 2:90–100, 2011.
Ising, M. S., et al. Flow modulation algorithms for intra-aortic rotary blood pumps to minimize coronary steal. ASAIO J. 59:261–268, 2013.
Kantrowitz, A., et al. Initial clinical experience with intraaortic balloon pum** in cardiogenic shock. J. Am. Med. Assoc. 203:113–118, 1968.
Klotz, S., et al. Partial mechanical long-term support with the CircuLite Synergy pump as bridge-to-transplant in congestive heart failure. Thorac. Cardiov. Surg. 58:S173–S178, 2010.
Koenig, S. C., et al. Hemodynamic and pressure-volume responses to continuous and pulsatile ventricular assist in an adult mock circulation. ASAIO J. 50:15–24, 2004.
Koenig, S. C., et al. Acute hemodynamic efficacy of a 32-ml subcutaneous counterpulsation device in a calf model of diminished cardiac function. ASAIO J. 54:578–584, 2008.
Kolyva, C., et al. Discerning aortic waves during intra-aortic balloon pum** and their relation to benefits of counterpulsation in humans. J. Appl. Physiol. 107:1497–1503, 2009.
Li, G., et al. Preliminary in vivo study of an intra-aortic impeller pump driven by an extracorporeal whirling magnet. Artif. Organs 26:890–893, 2002.
Mohite, P. N., et al. Does CircuLite Synergy assist device as partial ventricular support have a place in modern management of advanced heart failure? Expert Rev. Med. Device 12:49–60, 2015.
Olsen, D. Sixth international symposium for rotary blood pumps. Artif. Organs. 23:475–476, 1999.
Reitan, O., S. Steen, and H. Ohlin. Hemodynamic effects of a new percutaneous circulatory support device in a left ventricular failure model. ASAIO J. 49:731–736, 2003.
Rich, M. W. Congestive heart failure in older adults: epidemiology, pathophysiology and etiology of congestive heart failure in older adults. J. Am. Geriatr. Soc. 45:968–974, 1997.
Schroeder, M. J., et al. HEART: an automated beat-to-beat cardiovascular analysis package using Matlab. Comput. Biol. Med. 34:371–388, 2004.
Shah, A. P., et al. Clinical and economic effectiveness of percutaneous ventricular assist devices for high-risk patients undergoing percutaneous coronary intervention. J. Invasive Cardiol. 27:148–154, 2015.
Slaughter, M. S., et al. Advanced heart failure treated with continuous-flow left ventricular assist devices. N. Engl. J. Med. 361:2241–2251, 2009.
Smith, E. J., et al. A first-in-man study of the Reitan catheter pump for circulatory support in patients undergoing high-risk percutaneous coronary intervention. Catheter. Cardiovasc. Interv. 73:859–865, 2009.
Soucy, K. G., et al. Defining pulsatility during continuous-flow ventricular assist device support. J. Heart Lung Transpl. 32:581–587, 2013.
Soucy, K. G., et al. Fault detection in rotary blood pumps using motor speed response. ASAIO J. 59:410–419, 2013.
Starling, R. C., et al. Results of the post-U.S. Food and Drug Administration-approval study with a continuous flow left ventricular assist device as a bridge to heart transplantation: a prospective study using the INTERMACS (Interagency Registry for Mechanically Assisted Circulatory Support). J. Am. Coll. Cardiol. 57:1890–1898, 2011.
Syed, A. I., et al. Prophylactic use of intra-aortic balloon pump for high-risk percutaneous coronary intervention: will the Impella LP 2.5 device show superiority in a clinical randomized study? Cardiovasc. Revasc. Med. 91:91–97, 2010.
Wang, Y., et al. Rotary blood pump control strategy for preventing left ventricular suction. ASAIO J. 61:21–30, 2015.
Wang, Y., et al. Suction prevention and physiologic control of continuous flow left ventricular assist devices using intrinsic pump parameters. ASAIO J. 61:170–177, 2015.
Acknowledgments
Funding for this project was provided in part by NIH R15 Grant (1R15HL115556–01A1), and the University of Louisville Cardiac Implant Science Endowment.
Conflict of interest
All authors declare that they have no conflict of interest.
Human Studies/Informed Consent
No human studies were carried out by the authors for this article.
Animal Studies
No animal studies were carried out by the authors for this article.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editors John Timothy Baldwin and Ajit P. Yoganathan oversaw the review of this article.
Associate Editor John Timothy Baldwin and Ajit P. Yoganathan oversaw the review of this article.
Rights and permissions
About this article
Cite this article
Wang, Y., Koenig, S.C., Sobieski, M.A. et al. Hemodynamic Benefits of Counterpulsation, Implantable, Percutaneous, and Intraaortic Rotary Blood Pumps: An In-Silico and In Vitro Study. Cardiovasc Eng Tech 8, 439–452 (2017). https://doi.org/10.1007/s13239-017-0314-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13239-017-0314-1