Abstract
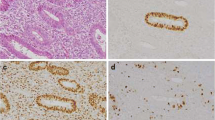
Clinicopathologic classification of endometrial cancer imperfectly reflects the tumor biology. Pathologic categorization — especially in high-grade tumors — results in an imprecise estimation of the risk of disease, recurrence, and death. Molecular subty** is emerging as the standard of care in diagnosis and treatment of endometrial cancers. Molecular markers are important prognostic factors in tumor dissemination and early recurrence of endometrial cancers. TP53 mutation is an important prognostic factor for both serous and endometrioid cancers. The study aims to compare the clinical profile and overall survival of endometrial cancers with and without p53 mutation. Sixty-three patients who underwent surgical staging for carcinoma endometrium were included in the study.TP53 mutation status was determined based on p53 expression by immunohistochemistry (IHC) as a p53 wild or p53 mutant type. Data were analyzed for the clinical profile, p53 mutation status on IHC, histological pattern, tumor grade, stage of the disease, lymph node spread, recurrence pattern, treatment received, 2-year disease-free survival, and overall survival. Recurrence was noted in 12.7% patients after 2-year follow-up, of which 75% patients had p53 mutation. Significant association was seen between p53 expression and high-grade tumors, stage, cervical involvement, and adnexal involvement. The 2-year overall survival of the p53 wild type was 97.2% and the p53 mutant type was 91.7%. The 2-year disease-free survival for the p53 wild type was 94.3% and the disease-free survival of the p53 mutant variety was 83.5%. The 2-year disease-free survival for endometrioid carcinoma with p53 wild type was 100% and p53 mutant variety was 86.2% (p value 0.033). About 15.9% (10) patients were reassigned to the high-risk group needing chemotherapy and radiation according to the ESGO ESTRO 2021 consensus classification, due to their p53 mutation status. IHC to assess somatic p53 mutation may be done in endometrial biopsies irrespective of their histology. This may help to identify that the aggressive tumors thereby help in tailoring surgery, planning adjuvant treatment, and follow-up.



Similar content being viewed by others
Data Availability
The data and material are available for review.
Code Availability
The data was coded and analyzed with SPSS software.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: a cancer journal for clinicians 71(3):209–49.
Mathew A, George PS, Kalavathy MC, Padmakumari G, Jagathnath Krishna KM, Sebastian P (2017) Cancer incidence and mortality: district cancer registry, Trivandrum, South India. Asian Pacific Journal of Cancer Prevention: APJCP 18(6):1485
Sohaib SA, Houghton SL, Meroni R, Rockall AG, Blake P, Reznek RH (2007) Recurrent endometrial cancer: patterns of recurrent disease and assessment of prognosis. Clin Radiol 62(1):28–34
Pecorelli S (2009) Revised FIGO staging for carcinoma of the vulva, cervix, and endometrium. Int J Gynaecol Obstet 105(2):103–104
Werner HM, Salvesen HB (2014) Current status of molecular biomarkers in endometrial cancer. Curr Oncol Rep 16(9):403
Kandoth C, Schultz N, Cherniack AD, Akbani R, Liu Y, Shen H, Robertson AG, Pashtan I, Shen R, Benz CC et al (2013) Integrated genomic characterization of endometrial carcinoma. Nature 497(7447):67–73
Zhao D, Tahaney WM, Mazumdar A, Savage MI, Brown PH (2017) Molecularly targeted therapies for p53-mutant cancers. Cell Mol Life Sci 74(22):4171–4187
Muller PA, Vousden KH (2013) p53 mutations in cancer. Nat Cell Biol 15(1):2–8
Matias-Guiu X, Prat J (2013) Molecular pathology of endometrial carcinoma. Histopathology 62(1):111–123
Levine DA, Cancer Genome Atlas Research Network (2013) Integrated genomic characterization of endometrial carcinoma. Nature 497(7447):67–73
Remmerie M, Janssens V (2018) Targeted therapies in type II endometrial cancers: too little, but not too late. Int J Mol Sci 19(8):2380
Köbel M, Ronnett BM, Singh N, Soslow RA, Gilks CB, McCluggage WG (2019) Interpretation of p53 immunohistochemistry in endometrial carcinomas: toward increased reproducibility. Int J Gynecol Pathol 38(1 Suppl 1):S123
Razumova Z, Bizzarri N, Kacperczyk-Bartnik J, Pletnev A, Martin AG, Persson J. Report from the European Society of Gynaecological Oncology (ESGO) 2020 State-of-the-Art Virtual Meeting. International Journal of Gynecologic Cancer. 2021;31(5).
van den Heerik AS, Horeweg N, Nout RA, Lutgens LC, van der Steen-Banasik EM, Westerveld GH, van den Berg HA, Slot A, Koppe FL, Kommoss S, Mens JW (2020) PORTEC-4a: international randomized trial of molecular profile-based adjuvant treatment for women with high-intermediate risk endometrial cancer. International Journal of Gynecologic Cancer:ijgc-2020.
Colombo N, Creutzberg C, Amant F, Bosse T, González-Martín A, Ledermann J, Marth C, Nout R, Querleu D, Mirza MR, Sessa C (2016) ESMO-ESGO-ESTRO consensus conference on endometrial cancer: diagnosis, treatment and follow-up. International Journal of Gynecologic Cancer. 26(1)
Ray S, Jha A, Islam AA, Sengupta M (2020) Study of prognostic and diagnostic significance of P53 and PTEN mutation in proliferative lesions of endometrium. Journal of Current Medical Research and Opinion 3(08):563–9
Watanabe T, Nanamiya H, Kojima M, Nomura S, Furukawa S, Soeda S, Tanaka D, Isogai T, Imai JI, Watanabe S, Fujimori K. Clinical relevance of oncogenic driver mutations identified in endometrial carcinoma
Schultheis AM, Martelotto LG, De Filippo MR, Piscuoglio S, Ng CK, Hussein YR, Reis-Filho JS, Soslow RA, Weigelt B (2016) TP53 mutational spectrum in endometrioid and serous endometrial cancers. International journal of gynecological pathology: official journal of the International Society of Gynecological Pathologists 35(4):289
Garg K, Leitao MM, Wynveen CA, Sica GL, Shia J, Shi W, Soslow RA (2010) p53 overexpression in morphologically ambiguous endometrial carcinomas correlates with adverse clinical outcomes. Mod Pathol 23(1):80–92
Akiyama A, Minaguchi T, Fujieda K, Hosokawa Y, Nishida K, Shikama A, Tasaka N, Sakurai M, Ochi H, Satoh T (2019) Abnormal accumulation of p53 predicts radioresistance leading to poor survival in patients with endometrial carcinoma. Oncol Lett 18(6):5952–5958
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
The study was conducted after institutional scientific and research board approval.
Consent to Participate
The study has been conducted after attaining consent to participate.
Consent for Publication
All authors consent for publication once it is accepted.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tresa, A., Sambasivan, S., Rema, P. et al. Clinical Profile and Survival Outcome of Endometrial Cancer with p53 Mutation. Indian J Surg Oncol 13, 580–586 (2022). https://doi.org/10.1007/s13193-022-01523-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13193-022-01523-9