Abstract
Background
Short and long sleep durations are common behaviors that could predict several cardiovascular diseases. However, the association between sleep duration and atrial fibrillation (AF) risk is not well-established. AF is preventable, and risk prevention approaches could reduce its occurrence. Investigating whether sleep duration could predict AF incidence for possible preventive interventions and determining the impact of various lifestyle and clinical characteristics on this association to personalize such interventions are essential. Herein, we investigated the association between sleep duration and AF risk using a prospective cohort study and a meta-analysis of epidemiological evidence.
Methods
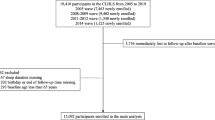
Data of 6898 people, aged 30–84 years, from the Suita Study, were analyzed. AF was diagnosed during the follow-up by ECG, medical records, checkups, and death certificates, while a baseline questionnaire was used to assess sleep duration. The Cox regression was used to compute the hazard ratios (HRs) and 95% confidence intervals (CIs) of AF risk for daily sleep ≤ 6 (short sleep), ≥ 8 (long sleep), and irregular sleep, including night-shift work compared with 7 h (moderate sleep). Then, we combined our results with those from other eligible prospective cohort studies in two meta-analyses for the short and long sleep.
Results
In the Suita Study, within a median follow-up period of 14.5 years, short and irregular sleep, but not long sleep, were associated with the increased risk of AF in the age- and sex-adjusted models: HRs (95% CIs) = 1.36 (1.03, 1.80) and 1.62 (1.16, 2.26) and the multivariable-adjusted models: HRs (95% CIs) = 1.34 (1.01, 1.77) and 1.63 (1.16, 2.30), respectively. The significant associations between short and irregular sleep and AF risk remained consistent across different ages, sex, smoking, and drinking groups. However, they were attenuated among overweight and hypertensive participants. In the meta-analyses, short and long sleep durations were associated with AF risk: pooled HRs (95% CIs) = 1.21 (1.02, 1.42) and 1.18 (1.03, 1.35). No signs of significant heterogeneity across studies or publication bias were detected.
Conclusion
Short, long, and irregular sleep could be associated with increased AF risk. In the context of predictive, preventive, and personalized medicine, sleep duration should be considered in future AF risk scores to stratify the general population for potential personalized lifestyle modification interventions. Sleep management services should be considered for AF risk prevention, and these services should be individualized according to clinical characteristics and lifestyle factors.
Graphical abstract




Similar content being viewed by others
Data availability
Available upon a reasonable request.
Code availability
NA.
Abbreviations
- AF:
-
Atrial fibrillation
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- HR:
-
Hazard ratio
- Metafor:
-
Meta-analysis package for R
- NOS:
-
Newcastle–Ottawa Quality Assessment Scale
- PPPM:
-
Predictive, preventive, and personalized medicine
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analysis
- SBP:
-
Systolic blood pressure
References
Lippi G, Sanchis-Gomar F, Cervellin G. Global epidemiology of atrial fibrillation: an increasing epidemic and public health challenge. Int J Stroke. 2021;16:217–21.
Dai H, Zhang Q, Much AA, Maor E, Segev A, Beinart R, et al. Global, regional, and national prevalence, incidence, mortality, and risk factors for atrial fibrillation, 1990–2017: results from the Global Burden of Disease Study 2017. Eur Heart J Qual Care Clin Outcomes. 2021;7:574–82.
Odutayo A, Wong CX, Hsiao AJ, Hopewell S, Altman DG, Emdin CA. Atrial fibrillation and risks of cardiovascular disease, renal disease, and death: systematic review and meta-analysis. BMJ. 2016;354:i4482.
Golubnitschaja O, Baban B, Boniolo G, Wang W, Bubnov R, Kapalla M, et al. Medicine in the early twenty-first century: paradigm and anticipation - EPMA position paper 2016. EPMA J. 2016;7:23.
Golubnitschaja O, Liskova A, Koklesova L, Samec M, Biringer K, Büsselberg D, et al. Caution, “normal” BMI: health risks associated with potentially masked individual underweight-EPMA Position Paper 2021. EPMA J. 2021;12:1–22.
Wang W, Yan Y, Guo Z, Hou H, Garcia M, Tan X, et al. All around suboptimal health - a joint position paper of the Suboptimal Health Study Consortium and European Association for Predictive Preventive and Personalised Medicine. EPMA J. 2021;12:1–31.
Kokubo Y, Matsumoto C. Traditional cardiovascular risk factors for incident atrial fibrillation. Circ J. 2016;80:2415–22.
Helms TM, Duong G, Zippel-Schultz B, Tilz RR, Kuck KH, Karle CA. Prediction and personalised treatment of atrial fibrillation-stroke prevention: consolidated position paper of CVD professionals. EPMA J. 2014;5:15.
Kokubo Y, Watanabe M, Higashiyama A, Nakao YM, Kusano K, Miyamoto Y. Development of a basic risk score for incident atrial fibrillation in a Japanese general population- the Suita Study. Circ J. 2017;81:1580–8.
O’Neal WT, Alonso A. The appropriate use of risk scores in the prediction of atrial fibrillation. J Thorac Dis. 2016;8:1391–4.
Hata J, Nagata T, Sakata S, Oishi E, Furuta Y, Hirakawa Y, et al. Risk prediction model for incident atrial fibrillation in a general Japanese population- the Hisayama Study. Circ J. 2021;85:1373–82.
Han X, Yang Y, Chen Y, Gao L, Yin X, Li H, et al. Association between insomnia and atrial fibrillation in a Chinese population: a cross-sectional study. Clin Cardiol. 2017;40:765–9.
Lee HH, Chen YC, Chen JJ, Lo SH, Guo YL, Hu HY. Insomnia and the risk of atrial fibrillation: a population-based cohort study. Acta Cardiol Sin. 2017;33:165–72.
Linz D, McEvoy RD, Cowie MR, Somers VK, Nattel S, Lévy P, et al. Associations of obstructive sleep apnea with atrial fibrillation and continuous positive airway pressure treatment: a review. JAMA Cardiol. 2018;3:532–40.
Kwon Y, Gadi S, Shah NR, Stout C, Blackwell JN, Cho Y, et al. Atrial fibrillation and objective sleep quality by slow wave sleep. J Atr Fibrillation. 2018;11:2031.
Kwon Y, Gharib SA, Biggs ML, Jacobs DR Jr, Alonso A, Duprez D, et al. Association of sleep characteristics with atrial fibrillation: the Multi-Ethnic Study of Atherosclerosis. Thorax. 2015;70:873–9.
Christensen MA, Dixit S, Dewland TA, Whitman IR, Nah G, Vittinghoff E, et al. Sleep characteristics that predict atrial fibrillation. Heart Rhythm. 2018;15:1289–95.
Chaput JP, Dutil C, Sampasa-Kanyinga H. Slee** hours: what is the ideal number and how does age impact this? Nat Sci Sleep. 2018;10:421–30.
Zhao J, Yang F, Zhuo C, Wang Q, Qu Z, Wang Q, et al. Association of sleep duration with atrial fibrillation and heart failure: a Mendelian randomization analysis. Front Genet. 2021;12:583658.
Kokubo Y, Kobayashi T, Watanbe M, Kusano K, Kamakura S, Miyamoto Y. A prospective study of sleep duration and the risk of incident atrial fibrillation in an urban population: the Suita Study. J Am Coll Cardiol. 2014;12:A1434.
Khawaja O, Sarwar A, Albert CM, Gaziano JM, Djoussé L. Sleep duration and risk of atrial fibrillation (from the Physicians’ Health Study). Am J Cardiol. 2013;111:547–51.
Song Q, Liu X, Hu W, Zhou W, Liu A, Wang X, et al. Long sleep duration is an independent risk factor for incident atrial fibrillation in a Chinese population: a prospective cohort study. Sci Rep. 2017;7:3679.
Genuardi MV, Ogilvie RP, Saand AR, DeSensi RS, Saul MI, Magnani JW, et al. Association of short sleep duration and atrial fibrillation. Chest. 2019;156:544–52.
Morovatdar N, Ebrahimi N, Rezaee R, Poorzand H, Bayat Tork MA, Sahebkar A. Sleep duration and risk of atrial fibrillation: a systematic review. J Atr Fibrillation. 2019;11:2132.
Kokubo Y, Watanabe M, Higashiyama A, Nakao YM, Kobayashi T, Watanabe T, et al. Interaction of blood pressure and body mass index with risk of incident atrial fibrillation in a Japanese urban cohort: the Suita Study. Am J Hypertens. 2015;28:1355–61.
Moher D, Liberati A, Tetzlaff J, Altman D; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:2535.
Wells G, Shea B, O'Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. www.ohri.ca/programs/clinical_epidemiology¥oxford.htm. Accessed 9 Nov 2021.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88.
Higgins J, Thompson S, Deeks J, Altman D. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34.
Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Software. 2010;36:1–48.
Chokesuwattanaskul R, Thongprayoon C, Sharma K, Congrete S, Tanawuttiwat T, Cheungpasitporn W. Associations of sleep quality with incident atrial fibrillation: a meta-analysis. Intern Med J. 2018;48:964–72.
Ozer O, Ozbala B, Sari I, Davutoglu V, Maden E, Baltaci Y, et al. Acute sleep deprivation is associated with increased QT dispersion in healthy young adults. Pacing Clin Electrophysiol. 2008;31:979–84.
Sari I, Davutoglu V, Ozbala B, Ozer O, Baltaci Y, Yavuz S, et al. Acute sleep deprivation is associated with increased electrocardiographic P-wave dispersion in healthy young men and women. Pacing Clin Electrophysiol. 2008;31:438–42.
Açar G, Akçakoyun M, Sari I, Bulut M, Alizade E, Özkan B, et al. Acute sleep deprivation in healthy adults is associated with a reduction in left atrial early diastolic strain rate. Sleep Breath. 2013;17:975–83.
Dilaveris PE, Gialafos JE. P-wave dispersion: a novel predictor of paroxysmal atrial fibrillation. Ann Noninvasive Electrocardiol. 2001;6:159–65.
Mandyam MC, Soliman EZ, Alonso A, Dewland TA, Heckbert SR, Vittinghoff E, et al. The QT interval and risk of incident atrial fibrillation. Heart Rhythm. 2013;10:1562–8.
Chen PS, Chen LS, Fishbein MC, Lin SF, Nattel S. Role of the autonomic nervous system in atrial fibrillation: pathophysiology and therapy. Circ Res. 2014;114:1500–15.
Rebecchi M, Panattoni G, Edoardo B, de Ruvo E, Sciarra L, Politano A, et al. Atrial fibrillation and autonomic nervous system: a translational approach to guide therapeutic goals. J Arrhythm. 2021;37:320–30.
Qin M, Zeng C, Liu X. The cardiac autonomic nervous system: a target for modulation of atrial fibrillation. Clin Cardiol. 2019;42:644–52.
Sardana M, Lessard D, Tsao CW, Parikh NI, Barton BA, Nah G, et al. Association of left atrial function index with atrial fibrillation and cardiovascular disease: the Framingham Offspring Study. J Am Heart Assoc. 2018;7:e008435.
Needleman M, Calkins H. The role of obesity and sleep apnea in atrial fibrillation. Curr Opin Cardiol. 2011;26:40–5.
Thomas MC, Dublin S, Kaplan RC, Glazer NL, Lumley T, Longstreth WT Jr, et al. Blood pressure control and risk of incident atrial fibrillation. Am J Hypertens. 2008;21:1111–6.
Soliman EZ, Rahman AF, Zhang ZM, Rodriguez CJ, Chang TI, Bates JT, et al. Effect of intensive blood pressure lowering on the risk of atrial fibrillation. Hypertension. 2020;75:1491–6.
Wang N, Sun Y, Zhang H, Wang B, Chen C, Wang Y, et al. Long-term night shift work is associated with the risk of atrial fibrillation and coronary heart disease. Eur Heart J. 2021;42:4180–8.
Hayter EA, Wehrens SMT, Van Dongen HPA, Stangherlin A, Gaddameedhi S, Crooks E, et al. Distinct circadian mechanisms govern cardiac rhythms and susceptibility to arrhythmia. Nat Commun. 2021;12:2472.
Acker J, Golubnitschaja O, Büttner-Teleaga A, Richter K. Wrist actigraphic approach in primary, secondary and tertiary care based on the principles of predictive, preventive and personalised (3P) medicine. EPMA J. 2021;12:1–15.
Richter K, Kellner S, Hillemacher T, Golubnitschaja O. Sleep quality and COVID-19 outcomes: the evidence-based lessons in the framework of predictive, preventive and personalised (3P) medicine. EPMA J. 2021;12:1–21.
Midelet A, Bailly S, Tamisier R, Borel JC, Baillieul S, Le Hy R, et al. Hidden Markov model segmentation to demarcate trajectories of residual apnoea-hypopnoea index in CPAP-treated sleep apnoea patients to personalize follow-up and prevent treatment failure. EPMA J. 2021;12(4):535–44.
Risso TT, Poyares D, Rizzi CF, Pulz C, Guilleminault C, Tufik S, et al. The impact of sleep duration in obstructive sleep apnea patients. Sleep Breath. 2013;17:837–43.
Acknowledgements
We would like to thank Drs. Kawanishi and Misaki, the former and current presidents of the Suita Medical Association, the members of Suita City Health Center, all cohort members, and staff. We also express our gratitude to Prof. Iso from Osaka University.
Funding
This study was supported by the Intramural Research Fund (20–4-9) for the cardiovascular diseases of the National Cerebral and Cardiovascular Center, JST Grant Number JPMJPF2018, the Meiji Yasuda Research Institute, Inc., and Meiji Yasuda Life Insurance Company.
Author information
Authors and Affiliations
Contributions
AA (draft writing, review literature, and data analysis), YK (resources, funding acquisition, and supervision), and all authors (visualization, validation, critical revision, and editing).
Corresponding author
Ethics declarations
Ethics approval
The Institutional Review Board of the National Cerebral and Cardiovascular Center, Suita, Japan, approved the study protocol (M25-043–4). The study was conducted per the Declaration of Helsinki.
Consent to participate
Written informed consent was obtained from all participants.
Consent for publication
All authors had full access to all the data in the study and accept responsibility to submit for publication.
Conflict of interest
The authors declare no competing interests.
Role of the funder
The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Arafa, A., Kokubo, Y., Shimamoto, K. et al. Sleep duration and atrial fibrillation risk in the context of predictive, preventive, and personalized medicine: the Suita Study and meta-analysis of prospective cohort studies. EPMA Journal 13, 77–86 (2022). https://doi.org/10.1007/s13167-022-00275-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13167-022-00275-4