Abstract
Objectives
This study aims at estimating the prevalence of cirrhotic cardiomyopathy in a cohort of cirrhosis patients in northern India using the World Congress of Gastroenterology 2005 criteria and its relationship with grades of cirrhosis, its complications, and all-cause mortality.
Methods
This was a prospective study in which 53 cirrhosis patients underwent the 2D color Doppler, and tissue Doppler echocardiography. Echocardiography findings were compared with thirty age- and sex-matched healthy controls. Additionally, serum pro-brain natriuretic peptide (pro-BNP) and troponin-T levels were measured. Patients were followed up for 6 months to look for complications and mortality.
Result
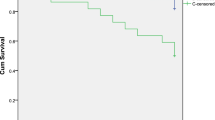
2D echocardiography findings revealed that diastolic cardiomyopathy with no gross systolic dysfunction was significantly prevalent in cirrhosis patients. Using the Montreal criteria, we found the incidence of diastolic cardiomyopathy to be 56.6%. Tissue Doppler echocardiography findings were also correlated. Diastolic dysfunction correlated with the severity of cirrhosis, and patients with higher Child score had more diastolic dysfunction. Serum pro-BNP levels and QTc interval were also higher in patients with diastolic dysfunction. On survival analysis, patients with cirrhotic cardiomyopathy had shorter survival and greater frequency of encephalopathy and hepatorenal syndrome (HRS) episodes as compared with cirrhotic patients without cardiomyopathy, though the differences were not statistically significant.
Conclusion
The study showed that diastolic dysfunction was highly prevalent (56.6% of the study population) in cirrhosis patients. QTc interval and pro-BNP were also significantly raised. Also, complications of cirrhosis like HRS, spontaneous bacterial peritonitis, and hepatic encephalopathy were more common in the cirrhotic cardiomyopathy group.


Similar content being viewed by others
References
Zardi EM, Abbate A, Zardi DM, et al. Cirrhotic cardiomyopathy. J Am Coll Cardiol. 2010;56:539–49.
Ruíz-del-Árbol L, Achécar L, Serradilla R, et al. Diastolic dysfunction is a predictor of poor outcomes in patients with cirrhosis, portal hypertension, and a normal creatinine. Hepatology. 2013;58:1732-41.
Zambruni A, Trevisani F, Caraceni P, Bernardi M. Cardiac electrophysiological abnormalities in patients with cirrhosis. J Hepatol. 2006;44:994–1002.
Cazzaniga M, Salerno F, Pagnozzi G, et al. Diastolic dysfunction is associated with poor survival in patients with cirrhosis with transjugular intrahepatic portosystemic shunt. Gut. 2007;56:869-75.
Alexander J, Mishra P, Desai N, Ambadekar S, Gala B, Sawant P. Cirrhotic cardiomyopathy: Indian scenario. J Gastroenterol Hepatol. 2007;22:395-9.
Møller S, Lee SS. Cirrhotic cardiomyopathy. J Hepatol. 2018;69:958–60.
Voiosu A, Wiese S, Voiosu T, Bendtsen F, Møller S. Bile acids and cardiovascular function in cirrhosis. Liver Int. 2017;37:1420-30.
Møller S, Bendtsen F. The pathophysiology of arterial vasodilatation and hyperdynamic circulation in cirrhosis. Liver Int Off J Int Assoc Study Liver. 2018;38:570–80.
Rombouts K, Niki T, Wielant A, et al. Effect of aldosterone on collagen steady state levels in primary and subcultured rat hepatic stellate cells. J Hepatol. 2001;34:230-8.
Møller S, Henriksen JH. Cardiovascular complications of cirrhosis. Gut. 2008;57:268–78.
Lazzeri C, La Villa G, Laffi G, et al. Autonomic regulation of heart rate and QT interval in nonalcoholic cirrhosis with ascites. Digestion. 1997;58:580-6.
Bernardi M, Maggioli C, Dibra V, Zaccherini G. QT interval prolongation in liver cirrhosis: innocent bystander or serious threat? Expert Rev Gastroenterol Hepatol. 2012;6:57–66.
Henriksen JH, Gøtze JP, Fuglsang S, Christensen E, Bendtsen F, Møller S. Increased circulating pro-brain natriuretic peptide (proBNP) and brain natriuretic peptide (BNP) in patients with cirrhosis: relation to cardiovascular dysfunction and severity of disease. Gut. 2003;52:1511-7.
Saner FH, Neumann T, Canbay A, et al. High brain-natriuretic peptide level predicts cirrhotic cardiomyopathy in liver transplant patients. Transpl Int. 2011;24:425-32.
Møller S, Søndergaard L, Møgelvang J, Henriksen O, Henriksen JH. Decreased right heart blood volume determined by magnetic resonance imaging: evidence of central underfilling in cirrhosis. Hepatology. 1995;22:472-8.
Funding
MD Thesis grant awarded to Dr. Neha Kapoor.
Author information
Authors and Affiliations
Contributions
1. N Kapoor: concept and design of study, acquisition and analysis of data, drafting of manuscript and revising it critically for important intellectual content, final approval of manuscript. 2. V Mehta: acquisition and analysis of data, drafting of manuscript and revising it critically for important intellectual content. 3. B Singh: acquisition and analysis of data, drafting of manuscript and revising it critically for important intellectual content. 4. R Karna: drafting of manuscript and revising it critically for important intellectual content. 5. S Kumar: concept and design of the study, final approval of manuscript. 6. P Kar: concept and design of the study, drafting of manuscript and revising it critically for important intellectual content, final approval of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
NK, VM, BS, RK, SK, and PK declare that they have no conflict of interest.
Ethics statement
The study was performed conforming to the Helsinki declaration of 1975, as revised in 2000 and 2008 concerning human and animal rights, and the authors followed the policy concerning informed consent as shown on Springer.com.
Disclaimer
The authors are solely responsible for the data and the contents of the paper. In no way, the Honorary Editor-in-Chief, Editorial Board Members, the Indian Society of Gastroenterology, or the printer/publishers are responsible for the results/findings and content of this article.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kapoor, N., Mehta, V., Singh, B. et al. Prevalence of cirrhotic cardiomyopathy and its relationship with serum pro-brain natriuretic peptide, hepatorenal syndrome, spontaneous bacterial peritonitis, and mortality. Indian J Gastroenterol 39, 481–486 (2020). https://doi.org/10.1007/s12664-020-01083-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-020-01083-2