Abstract
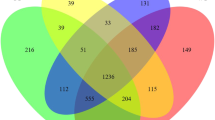
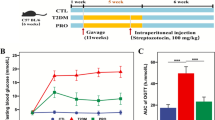
In our previous study, we identified a metabolite of Bacillus subtilis BS-Z15 (a strain with probiotic characteristics) that could improve immunity in mice. In the present study, we examined the effects of B. subtilis BS-Z15 and its metabolites on body weight gain and the intestinal microbiota of mice. Sixty 25-day-old male Kunming white mice were selected and randomly divided into four groups: control group (A), daily saline gavage; B. subtilis-treated group (B), single gavage (1 × 109 CFU/time/animal/day); group D, 14 consecutive gavages (1 × 109 CFU/time/animal/day); and B. subtilis metabolite-treated group (E), 30 consecutive gavages (90 mg kg−1/time/animal/day). High-throughput sequencing technology was used to analyze intergroup differences in the mouse intestinal microbiota. The results showed that the three treated groups had significantly slower body weight gain compared with the control group, which lasted until the 45 days (P < 0.05), and the daily food intake of the treated mice was higher (P < 0.05). The intestinal microbiota structure of the mice in the treated groups was significantly altered compared with that in the control group, suggesting that B. subtilis BS-Z15 may regulate the weight gain of animals by affecting their intestinal bacterial composition. After stop** the gavage of B. subtilis BS-Z15, the abundance of this strain in the small intestine of the mice gradually decreased and its presence was undetectable at 45 days, indicating that B. subtilis BS-Z15 could not colonize the intestine of these mice. These findings suggest that B. subtilis BS-Z15 may regulate intestinal microbiota through its metabolites to reduce weight gain.






Similar content being viewed by others
Availability of Data and Materials
The datasets supporting the conclusions of this article are included within the article and its additional file. Data will be made available on reasonable request. All authors ensure that all data and materials, as well as software applications or custom code, support their published claims and adhere to domain standards.
References
Matsuda M, Shimomura I (2013) Increased oxidative stress in obesity: implications for metabolic syndrome, diabetes, hypertension, dyslipidemia, atherosclerosis, and cancer. Obes Res Clin Pract 7(5):e330–e341. https://doi.org/10.1016/j.orcp.2013.05.004
Baragetti A, Bonacina F, Catapano AL, Norata GD (2021) Effect of lipids and lipoproteins on hematopoietic cell metabolism and commitment in atherosclerosis. Immunometabolism 3(2):e210014. https://doi.org/10.20900/immunometab20210014
Ng M, Fleming T, Robinson M, Thomson B, Graetz N et al (2014) Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the global burden of disease study 2013. Lancet 384(9945):766–781. https://doi.org/10.1016/S0140-6736(14)60460-8
Calle EE, Kaaks R (2004) Overweight, obesity and cancer: epidemiological evidence and proposed mechanisms. Nat Rev Cancer 4(8):579–591. https://doi.org/10.1038/nrc1408
El Aidy S, Derrien M, Merrifield CA et al (2013) Gut bacteria-host metabolic interplay during conventionalisation of the mouse germfree colon. ISME J 7(4):743–755. https://doi.org/10.1038/ismej.2012.142
Ley RE, Turnbaugh PJ, Klein S, Gordon JI (2006) Microbial ecology: human gut microbes associated with obesity. Nature 444(7122):1022–1023. https://doi.org/10.1038/4441022a
Zhao L (2013) The gut microbiota and obesity: from correlation to causality. Nat Rev Microbiol 11(9):639–647. https://doi.org/10.1038/nrmicro3089
Kang JH, Yun SI, Park HO (2010) Effects of Lactobacillus gasseri BNR17 on body weight and adipose tissue mass in diet-induced overweight rats. J Microbiol 48(5):712–714. https://doi.org/10.1007/s12275-010-0363-8
Liu R, Hong J, Xu X, Feng Q, Zhang D, Gu Y, Shi J, Zhao S, Liu W, Wang X, **a H, Liu Z, Cui B, Liang P, ** L, ** J, Ying X, Wang X, Zhao X, Li W, Jia H, Lan Z, Li F, Wang R, Sun Y, Yang M, Shen Y, Jie Z, Li J, Chen X, Zhong H, **e H, Zhang Y, Gu W, Deng X, Shen B, Xu X, Yang H, Xu G, Bi Y, Lai S, Wang J, Qi L, Madsen L, Wang J, Ning G, Kristiansen K, Wang W (2017) Gut microbiome and serum metabolome alterations in obesity and after weight-loss intervention. Nat Med 23(7):859–868. https://doi.org/10.1038/nm.4358
Plovier H, Everard A, Druart C, Depommier C, Van Hul M, Geurts L, Chilloux J, Ottman N, Duparc T, Lichtenstein L, Myridakis A, Delzenne NM, Klievink J, Bhattacharjee A, van der Ark KC, Aalvink S, Martinez LO, Dumas ME, Maiter D, Loumaye A, Hermans MP, Thissen JP, Belzer C, de Vos WM, Cani PD (2017) A purified membrane protein from Akkermansia muciniphila or the pasteurized bacterium improves metabolism in obese and diabetic mice. Nat Med 23(1):107–113. https://doi.org/10.1038/nm.4236
Endo H, Niioka M, Kobayashi N, Tanaka M, Watanabe T (2013) Butyrate-producing probiotics reduce nonalcoholic fatty liver disease progression in rats: new insight into the probiotics for the gut-liver axis. PLoS One 8(5):e63388. https://doi.org/10.1371/journal.pone.0063388
Everard A, Matamoros S, Geurts L, Delzenne NM, Cani PD (2014) Saccharomyces boulardii administration changes gut microbiota and reduces hepatic steatosis, low-grade inflammation, and fat mass in obese and type 2 diabetic db/db mice. MBio 5(3):e01011-e1014. https://doi.org/10.1128/mBio.01011-14
Shirvani-Rad S, Tabatabaei-Malazy O, Mohseni S, Hasani-Ranjbar S, Soroush AR, Hoseini-Tavassol Z, Ejtahed HS, Larijani B (2021) Probiotics as a complementary therapy for management of obesity: a systematic review. Evid Based Complement Alternat Med 2021:6688450. https://doi.org/10.1155/2021/6688450
Aoun A, Darwish F, Hamod N (2020) The influence of the gut microbiome on obesity in adults and the role of probiotics, prebiotics, and synbiotics for weight loss. Prev Nutr Food Sci 25(2):113–123. https://doi.org/10.3746/pnf.2020.25.2.113
Meena KR, Sharma A, Kanwar SS (2020) Antitumoral and antimicrobial activity of surfactin extracted from Bacillus subtilis KLP2015. Int J Pept Res 26:423–433. https://doi.org/10.1007/s10989-019-09848-w
Yahav S, Berkovich Z, Ostrov I, Reifen R, Shemesh M (2018) Encapsulation of beneficial probiotic bacteria in extracellular matrix from biofilm-forming Bacillus subtilis. Artif Cells Nanomed Biotechnol 46(sup2):974–982. https://doi.org/10.1080/21691401.2018.1476373
Abdel-Moneim AE, Selim DA, Basuony HA, Sabic EM, Saleh AA, Ebeid TA (2020) Effect of dietary supplementation of Bacillus subtilis spores on growth performance, oxidative status, and digestive enzyme activities in Japanese quail birds. Trop Anim Health Prod 52(2):671–680. https://doi.org/10.1007/s11250-019-02055-1
Bilal M, Si W, Barbe F, Chevaux E, Sienkiewicz O, Zhao X (2021) Effects of novel probiotic strains of bacillus pumilus and Bacillus subtilis on production, gut health, and immunity of broiler chickens raised under suboptimal conditions. Poult Sci 100(3):100871. https://doi.org/10.1016/j.psj.2020.11.048
Fuller R (1989) Probiotics in man and animals. J Appl Bacteriol 66(5):365–378. https://doi.org/10.1111/j.1365-2672.1989.tb05105.x
Hu Y, Dun Y, Li S, Zhao S, Peng N, Liang Y (2014) Effects of Bacillus subtilis KN-42 on growth performance, diarrhea and faecal bacterial flora of weaned piglets. Asian-Australas J Anim Sci 27(8):1131–1140. https://doi.org/10.5713/ajas.2013.13737
Lei K, Li YL, Wang Y, Wen J, Wu HZ, Yu DY, Li WF (2015) Effect of dietary supplementation of Bacillus subtilis B10 on biochemical and molecular parameters in the serum and liver of high-fat diet-induced obese mice. J Zhejiang Univ Sci B 16(6):487–495. https://doi.org/10.1631/jzus.B1400342
Zhang Y, Sun Q, Li ZW, Wang HY, Li JP, Wan XY (2019) Fermented soybean powder containing Bacillus subtilis sjlh001 protects against obesity in mice by improving transport function and inhibiting angiogenesis. J Funct Foods 59:60–70. https://doi.org/10.1016/j.jff.2019.05.033
Do HJ, Chung JH, Hwang JW, Kim OY, Lee JY, Shin MJ (2015) 1-Deoxynojirimycin isolated from Bacillus subtilis improves hepatic lipid metabolism and mitochondrial function in high-fat-fed mice. Food Chem Toxicol 75:1–7. https://doi.org/10.1016/j.fct.2014.11.001
Zouari R, Hamden K, Feki AE, Chaabouni K, Makni-Ayadi F, Kallel C, Sallemi F, Ellouze-Chaabouni S, Ghribi-Aydi D (2016) Protective and curative effects of Bacillus subtilis SPB1 biosurfactant on high-fat-high-fructose diet induced hyperlipidemia, hypertriglyceridemia and deterioration of liver function in rats. Biomed Pharmacother 84:323–329. https://doi.org/10.1016/j.biopha.2016.09.023
Zhao QQ, Wu MJ, Dong YY, Wang QY (2018) Antifungal activity of BS-Z15 metabolites and safety evaluation of its safety in mice. Nat Prod Res Dev 30:1608–1613. https://doi.org/10.16333/j.1001-6880.2018.9.023
Chen ZY, Li JY, Ge FW, Abuduaini X, Zhao JJ, Ning HC, Zhao HP, Zhao HX (2020) The effect of Bacillus subtilis BS-Z15 metabolites in the treatment of Candida albicans-infected Kunming mice. Nat Prod Res Dev 09:1608–1613. http://kns.cnki.net/kcms/detail/51.1335.Q.20201230.1528.002.html. Accessed 5 Oct 2021
Verrucci M, Iacobino A, Fattorini L, Marcoaldi R, Maggio A, Piccaro G (2019) Use of probiotics in medical devices applied to some common pathologies. Ann Ist Super Sanita 55(4):380–385. https://doi.org/10.4415/ANN_19_04_12
Reichelt AC, Loughman A, Bernard A, Raipuria M, Abbott KN, Dachtler J, Van TTH, Moore RJ (2020) An intermittent hypercaloric diet alters gut microbiota, prefrontal cortical gene expression and social behaviours in rats. Nutr Neurosci 23(8):613–627. https://doi.org/10.1080/1028415X.2018.1537169
Cai W, Xu J, Li G, Liu T, Guo X, Wang H, Luo L (2019) Ethanol extract of propolis prevents high-fat diet-induced insulin resistance and obesity in association with modulation of gut microbiota in mice. Food Res Int 130:108939. https://doi.org/10.1016/j.foodres.2019.108939
Lee CJ, Sears CL, Maruthur N (2020) Gut microbiome and its role in obesity and insulin resistance. Ann N Y Acad Sci 1461(1):37–52. https://doi.org/10.1111/nyas.14107
Goffredo M, Mass K, Parks EJ, Wagner DA, McClure EA, Graf J, Savoye M, Pierpont B, Cline G, Santoro N (2016) Role of gut microbiota and short chain fatty acids in modulating energy harvest and fat partitioning in youth. J Clin Endocrinol Metab 101(11):4367–4376. https://doi.org/10.1210/jc.2016-1797
Abenavoli L, Scarpellini E, Colica C, Boccuto L, Salehi B, Sharifi-Rad J, Aiello V, Romano B, De Lorenzo A, Izzo AA, Capasso R (2019) Gut microbiota and obesity: a role for probiotics. Nutrients 11(11):2690. https://doi.org/10.3390/nu11112690
Hwang I, Park YJ, Kim YR, Kim YN, Ka S, Lee HY, Seong JK, Seok YJ, Kim JB (2015) Alteration of gut microbiota by vancomycin and bacitracin improves insulin resistance via glucagon-like peptide 1 in diet-induced obesity. FASEB J 29(6):2397–2411. https://doi.org/10.1096/fj.14-265983
Stojanov S, Berlec A, Štrukelj B (2020) The influence of probiotics on the Firmicutes/Bacteroidetes ratio in the treatment of obesity and inflammatory bowel disease. Microorganisms 8(11):1715. https://doi.org/10.3390/microorganisms8111715
Donaldson GP, Lee SM, Mazmanian SK (2016) Gut biogeography of the bacterial microbiota. Nat Rev Microbiol 14(1):20–32. https://doi.org/10.1038/nrmicro3552
Hill-Burns EM, Debelius JW, Morton JT, Wissemann WT, Lewis MR, Wallen ZD, Peddada SD, Factor SA, Molho E, Zabetian CP, Knight R, Payami H (2017) Parkinson’s disease and Parkinson’s disease medications have distinct signatures of the gut microbiome. Mov Disord 32(5):739–749. https://doi.org/10.1002/mds.26942
Magro DO, de Oliveira LM, Bernasconi I, Ruela Mde S, Credidio L, Barcelos IK, Leal RF, Ayrizono Mde L, Fagundes JJ, Teixeira Lde B, Ouwehand AC, Coy CS (2014) Effect of yogurt containing polydextrose, Lactobacillus acidophilus NCFM and Bifidobacterium lactis HN019: a randomized, double-blind, controlled study in chronic constipation. Nutr J 13:75. https://doi.org/10.1186/1475-2891-13-75
Biagia G, Cipollini I, Paulicks BR, Roth FX (2010) Effect of tannins on growth performance and intestinal ecosystem in weaned piglets. Arch Anim Nutr 64(2):121–135. https://doi.org/10.1080/17450390903461584
Wang K, Cao G, Zhang H, Li Q, Yang C (2019) Effects of clostridium butyricum and Enterococcus faecalis on growth performance, immune function, intestinal morphology, volatile fatty acids, and intestinal flora in a piglet model. Food Funct 10(12):7844–7854. https://doi.org/10.1039/c9fo01650c
Wa Y, Yin B, He Y, ** W, Huang Y, Wang C, Guo F, Gu R (2019) Effects of single probiotic- and combined probiotic-fermented milk on lipid metabolism in hyperlipidemic rats. Front Microbiol 10:1312. https://doi.org/10.3389/fmicb.2019.01312
Yan F, Li N, Shi J, Li H, Yue Y, Jiao W, Wang N, Song Y, Huo G, Li B (2019) Lactobacillus acidophilus alleviates type 2 diabetes by regulating hepatic glucose, lipid metabolism and gut microbiota in mice. Food Funct 10(9):5804–5815. https://doi.org/10.1039/C9FO01062a
Kaspar F, Neubauer P, Gimpel M (2019) Bioactive secondary metabolites from Bacillus subtilis: a comprehensive review. J Nat Prod 82(7):2038–2053. https://doi.org/10.1021/acs.jnatprod.9b00110
Acknowledgements
Thanks to the support of Key Laboratory of Special Environment Biodiversity Application and Regulation in **njiang, The Key Discipline Biology, **njiang Normal University. Thanks to researcher Dao-Yuan Zhang of the Institute of Ecology and Geography, **njiang Branch of the Chinese Academy of Sciences for providing good guidance in the implementation of the project.
Funding
This work was supported by grants from Scientific Research Program of Colleges and Universities in **njiang (No. XJEDU2021I023), Natural Science Foundation of China (No.32160074), and the Open Project of Key Laboratory in **njiang (No. 2020D4010).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Hui-**n Zhao and He-** Zhao conceived of and designed the experiments. Jun Yang and Huan-Chen Ning performed the experiments and wrote the articles. Jun-Qi Yue and Qi Zhang helped to perform the experiments and collected the data. Huan-Chen Ning and **-Yu Li participated in the statistical analysis. **-Yuan Cao helped with the chart processing. Hui-**n Zhao and Ling Liu contributed to manuscript discussion and revision. Hui-**n Zhao is the first corresponding author, and Professor He-** Zhao and Associate Professor Ling Liu are the co-corresponding authors. Jun Yang, Huan-Chen Ning, and Qi Zhang are co-contributing authors. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics Approval and Consent to Participate
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed. This article does not contain any studies with human participants performed by any of the authors. Animal protocol approval: **njiang Medical University, SYXK (**n) 2018–0003.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yang, J., Ning, HC., Zhang, Q. et al. Effects of Bacillus subtilis BS-Z15 on Intestinal Microbiota Structure and Body Weight Gain in Mice. Probiotics & Antimicro. Prot. 15, 706–715 (2023). https://doi.org/10.1007/s12602-021-09897-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12602-021-09897-y