Abstract
Background
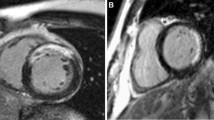
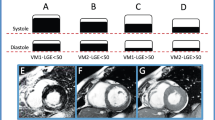
It had not been reported that myocardial scar shown on gated myocardial perfusion SPECT (GMPS) might reduce after cardiac resynchronization therapy (CRT). In this study, we aim to investigate the clinical impact and characteristic of scar reduction (SR) after CRT.
Methods and Results
Sixty-one heart failure patients following standard indication for CRT received twice GMPS as pre- and post-CRT evaluations. The patients with an absolute reduction of scar ≥ 10% after CRT were classified as the SR group while the rest were classified as the non-SR group. The SR group (N = 22, 36%) showed more improvement on LV function (∆LVEF: 18.1 ± 12.4 vs 9.4 ± 9.9 %, P = 0.007, ∆ESV: − 91.6 ± 52.6 vs − 38.1 ± 46.5 mL, P < 0.001) and dyssynchrony (ΔPSD: − 26.19 ± 18.42 vs − 5.8 ± 23.0°, P < 0.001, Δ BW: − 128.7 ± 82.8 vs − 25.2 ± 109.0°, P < 0.001) than non-SR group (N = 39, 64%). Multivariate logistic regression analysis showed baseline QRSd (95% CI 1.019-1.100, P = 0.006) and pre-CRT Reduced Wall Thickening (RWT) (95% CI 1.016-1.173, P = 0.028) were independent predictors for the development of SR.
Conclusion
More than one third of patients showed SR after CRT who had more post-CRT improvement on LV function and dyssynchrony than those without SR. Wider QRSd and higher RWT before CRT were related to the development of SR after CRT.



Similar content being viewed by others
Abbreviations
- ACEi:
-
Angiotensin-converting enzyme inhibitor
- ARB:
-
Angiotensin receptor blockers
- BW:
-
Bandwidth
- CRT:
-
Cardiac resynchronization therapy
- ECG:
-
Electrocardiography
- EDV:
-
End-diastolic volume
- ESV:
-
End-systolic volume
- GMPS:
-
Gated myocardial perfusion SPECT
- HF:
-
Heart failure
- HR:
-
Heart rate
- LVEDD:
-
LV end-diastolic diameter
- LVEF:
-
LV ejection fractions
- MRR:
-
Mechanical reverse remodeling
- NYHA:
-
New York Heart Association
- PSD:
-
Phase standard deviation
- QRSd:
-
QRS duration
- ROC:
-
Receiver operating characteristic
- RWT:
-
Reduced wall thickening
- SR:
-
Scar deduction
References
Lozano I, Bocchiardo M, Achtelik M, Gaita F, Trappe HJ, Daoud E et al. Impact of biventricular pacing on mortality in a randomized crossover study of patients with heart failure and ventricular arrhythmias. Pacing Clin Electrophysiol 2000; 23:1711-12
Abraham WT, Fisher WG, Smith AL, Delurgio DB, Leon AR, Loh E et al. Cardiac resynchronization in chronic heart failure. N Engl J Med 2002; 346:1845-53
Cheng CM, Huang JL, Wu TJ, Hsieh YC, Wang KY, Chen SA. An overview of current cardiac resynchronization therapy. Acta Cardiol Sin 2013; 29:496-04
Chiang KF, Cheng CM, Tsai SC, Lin WY, Chang YC, Huang JL et al. Relationship of myocardial substrate characteristics as assessed by myocardial perfusion imaging and cardiac reverse remodeling levels after cardiac resynchronization therapy. Ann Nucl Med 2016; 30:484-93
Tsai SC, Chang YC, Chiang KF, Lin WY, Huang JL, Hung GU et al. LV Dyssynchrony is helpful in predicting ventricular arrhythmia in ischemic cardiomyopathy after cardiac resynchronization therapy: A preliminary study. Medicine (Baltimore) 2016; 95:e2840
Chiang KF, Hung GU, Tsai SC, Cheng CM, Chang YC, Lin WY et al. Impact of cardiac reverse remodeling after cardiac resynchronization therapy assessed by myocardial perfusion imaging on ventricular arrhythmia. J Nucl Cardiol 2017; 24:1282-88
Ahmed W, Samy W, Tayeh O, Behairy N, Abd El Fattah A. Left ventricular scar impact on left ventricular synchronization parameters and outcomes of cardiac resynchronization therapy. Int J Cardiol 2016; 222:665-70
Chen J, Bax JJ, Henneman MM, Boogers MJ, Garcia EV. Is nuclear imaging a viable alternative technique to assess dyssynchrony? Europace 2008; 10:iii101-5
Chen J, Garcia EV, Lerakis S, Henneman MM, Bax JJ, Trimble MA et al. Left ventricular mechanical dyssynchrony as assessed by phase analysis of ECG-gated SPECT myocardial perfusion imaging. Echocardiography 2008; 25:1186-94
Chen J, Henneman MM, Trimble MA, Bax JJ, Borges-Neto S, Iskandrian AE et al. Assessment of left ventricular mechanical dyssynchrony by phase analysis of ECG-gated SPECT myocardial perfusion imaging. J Nucl Cardiol 2008; 15:127-36
Atchley AE, Trimble MA, Samad Z, Shaw LK, Pagnanelli R, Chen J et al. Use of phase analysis of gated SPECT perfusion imaging to quantify dyssynchrony in patients with mild-to-moderate left ventricular dysfunction. J Nucl Cardiol 2009; 16:888-94
Brandão SC, Nishioka SA, Giorgi MC, Chen J, Abe R, Martinelli Filho M et al. Cardiac resynchronization therapy evaluated by myocardial scintigraphy with 99mTc-MIBI: Changes in left ventricular uptake, dyssynchrony, and function. Eur J Nucl Med Mol Imaging 2009; 36:986-96
Cheng CM, Huang JL, Wu TJ, Su CS, Pai HY, Liao MF et al. Comparison of quick optimization of interventricular delay between simple methods: Intracardiac electrogram and surface electrocardiogram after cardiac resynchronization therapy. Europace 2012; 14:1317-23
Cheng CM, Su CS, Chou P, Liao YC, Wang CY, Zhang JR et al. Prediction of both electrical and mechanical reverse remodeling on acute electrocardiogram changes after cardiac resynchronization therapy. Circ J 2017; 81:1322-28
Sade LE, Saba S, Marek JJ, Onishi T, Schwartzman D, Adelstein EC et al. The association of left ventricular lead position related to regional scar by speckle-tracking echocardiography with clinical outcomes in patients receiving cardiac resynchronization therapy. J Am Soc Echocardiogr 2014; 27:648-56
Ypenburg C, van Bommel RJ, Delgado V, Mollema SA, Bleeker GB, Boersma E et al. Optimal left ventricular lead position predicts reverse remodeling and survival after cardiac resynchronization therapy. J Am Coll Cardiol 2008; 52:1402-09
Zhou W, Garcia EV. Nuclear image-guided approaches for cardiac resynchronization therapy (CRT). Curr Cardiol Rep 2016; 18:7
Luparelli M, Buccheri D, Corrado E, Ajello L, Bentivegna R, Ciaramitaro G et al. The importance of being “responder” in cardiac resynchronization therapy. Int J Cardiol 2016; 223:838-41
Zecchin M, Proclemer A, Magnani S, Vitali-Serdoz L, Facchin D, Muser D et al. Long-term outcome of “super-responder” patients to cardiac resynchronization therapy. Europace 2014; 16:363-71
Hou PN, Tsai SC, Lin WY, Cheng CM, Chiang KF, Chang YC et al. Relationship of quantitative parameters of myocardial perfusion SPECT and ventricular arrhythmia in patients receiving cardiac resynchronization therapy. Ann Nucl Med 2015; 29:772-78
Chen J, Garcia EV, Folks RD, Cooke CD, Faber TL, Tauxe EL et al. Onset of left ventricular mechanical contraction as determined by phase analysis of ECG-gated myocardial perfusion SPECT imaging: Development of a diagnostic tool for assessment of cardiac mechanical dyssynchrony. J Nucl Cardiol 2005; 12:687-95
Garcia EV, Faber TL, Cooke CD, Folks RD, Chen J, Santana C. The increasing role of quantification in clinical nuclear cardiology: The Emory approach. J Nucl Cardiol 2007; 14:420-32
Knaapen P, van Campen LM, de Cock CC, Götte MJ, Visser CA, Lammertsma AA et al. Effects of cardiac resynchronization therapy on myocardial perfusion reserve. Circulation 2004; 110:646-51
Stavrakis S, Lazzara R, Thadani U. The benefit of cardiac resynchronization therapy and QRS duration: A meta-analysis. J Cardiovasc Electrophysiol 2012; 23:163-68
Sassone B, Bertini M, Beltrami M, Malagù M, Pasanisi G, Kuwornu HA et al. Relation of QRS duration to response to cardiac resynchronization therapy in patients with left bundle branch block. Am J Cardiol 2017; 119:1803-08
Fleischmann S, Koepfli P, Namdar M, Wyss CA, Jenni R, Kaufmann PA. Gated (99m)Tc-tetrofosmin SPECT for discriminating infarct from artifact in fixed myocardial perfusion defects. J Nucl Med 2004; 45:754-59
Yang W, Zhang F, Tang H, Shao X, Wang J, Wang X et al. Summed thickening score by myocardial perfusion imaging: A risk factor of left ventricular remodeling in patients with myocardial infarction. J Nucl Cardiol 2018; 25:742-53
Zhang F, Wang J, Shao X, Yang M, Qian Y, Yang X et al. Incremental value of myocardial wall motion and thickening to perfusion alone by gated SPECT myocardial perfusion imaging for viability assessment in patients with ischemic heart failure. J Nucl Cardiol. 2020. https://doi.org/10.1007/s12350-020-02040-4
Hung GU, Huang JL, Lin WY, Tsai SC, Wang KY, Chen SA et al. Impact of right-ventricular apical pacing on the optimal left-ventricular lead positions measured by phase analysis of SPECT myocardial perfusion imaging. Eur J Nucl Med Mol Imaging 2014; 41:1224-31
Disclosures
This study was supported by a Grant from the Taiwan Ministry of Science and Technology (Project Number: 107-2314-B-758-001-MY3, PI: Guang-Uei Hung) and Taichung Veterans General Hospital (Project Number: TCVGH-1093103C, TCVGH-1083104C, TCVGH-1073104C, PI: **-Long Huang). This research was also supported in part by a grant from the American Heart Association (Project Number: 17AIREA33700016, PI: Weihua Zhou) and a new faculty startup grant from Michigan Technological University Institute of Computing and Cybersystems (PI: Weihua Zhou). No other potential conflicts of interest relevant to this article exist.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The authors of this article have provided a PowerPoint file, available for download at SpringerLink, which summarizes the contents of the paper and is free for re-use at meetings and presentations. Search for the article DOI on SpringerLink.com.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wang, CY., Hung, GU., Lo, HC. et al. Clinical impacts of scar reduction on gated myocardial perfusion SPECT after cardiac resynchronization therapy. J. Nucl. Cardiol. 29, 2571–2579 (2022). https://doi.org/10.1007/s12350-021-02722-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-021-02722-7