Abstract
Introduction
Gastrointestinal symptoms as well as depression and anxiety can negatively affect the effectiveness of military training and combat in general. This cross-sectional study aimed to determine the prevalence of gastrointestinal symptoms in recruits and further validate their associations with depression and anxiety.
Methods
A self-report questionnaire was sent to the recruits in an army in April 2022, which primarily included the Symptom Rating Scale (GSRS) for the assessment of gastrointestinal symptoms, the Bristol Stool Scale (BSS) for stool consistency and shape, the Patient Health Questionnaire-9 (PHQ-9) for depression, and the 7-item Generalized Anxiety Disorder scale (GAD-7) for anxiety. Correlation of gastrointestinal symptoms with depression and anxiety was evaluated.
Results
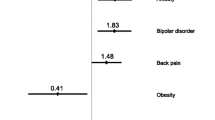
Overall, 467 recruits were included. Their median age was 21.0 years old (range: 18.0–24.0), and 98.1% of them were male. The proportion of gastrointestinal symptoms, abnormal stools, depression, and anxiety was 69.2% (n = 323), 11.3% (n = 53), 17.6% (n = 82), and 12.2% (n = 57), respectively. The recruits with gastrointestinal symptoms evaluated by GSRS had significantly higher prevalence of depression (P < 0.001) and anxiety (P < 0.001) than those without. GSRS score positively correlated with PHQ-9 (rs = 0.440, P < 0.001) and GAD-7 score (rs = 0.386, P < 0.001).
Conclusion
Gastrointestinal symptoms are very common in recruits, and positively correlate with depression and anxiety.
Similar content being viewed by others
Data Availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Wang WF, Guo XX, Yang YS. Gastrointestinal problems in modern wars: clinical features and possible mechanisms. Mil Med Res. 2015;2:15.
Lopes-João A, Costa I, Mesquita JR, et al. Multiple enteropathogenic viruses in a gastroenteritis outbreak in a military exercise of the Portuguese army. J Clin Virol. 2015;68:73–5.
Zhou Q, Verne ML, Zhang B, et al. Evidence for somatic hypersensitivity in veterans with gulf war illness and gastrointestinal symptoms. Clin J Pain. 2018;34(10):944–9.
Valle M, Vieira IA, Fino LC, et al. Immune status, well-being and gut microbiota in military supplemented with synbiotic ice cream and submitted to field training: a randomised clinical trial. Br J Nutr. 2021;126(12):1794–808.
Update: mental health disorders and mental health problems, active component, U.S. Armed Forces, 2016–2020. Msmr, 2021, 28(8): 2–9.
Günlü S, Aktan A. Evaluation of military recruits with complaints of palpitations after physical training: a study from Turkey. Cureus. 2022;14(9): e29284.
Alexopoulos P, Papanastasiou AD, Εconomou P, et al. Associations between APOE-, COMT Val108/158Met- and BDNF Val66Met polymorphisms and variations in depressive and anxiety symptoms, sense of coherence and vital exhaustion in the real-life setting of mandatory basic military training. J Neural Transm (Vienna). 2021;128(1):105–14.
Söderquist F, Syk M, Just D, et al. A cross-sectional study of gastrointestinal symptoms, depressive symptoms and trait anxiety in young adults. BMC Psychiatry. 2020;20(1):535.
Gibson N, Drain JR, Larsen P, et al. Subjective measures of workload and sleep in australian army recruits; potential utility as monitoring tools. Mil Med. 2023;188(3–4):670–7.
Liu T, Liu J, Wang C, et al. Prevalence of gastrointestinal symptoms and their association with psychological problems in youths. Ann Palliat Med. 2023;12(2):311–23.
Raiteri A, Granito A, Giamperoli A, et al. Current guidelines for the management of celiac disease: a systematic review with comparative analysis. World J Gastroenterol. 2022;28(1):154–75.
Souza GS, Sardá FA, Giuntini EB, et al. Translation and validation of the brazilian portuguese version of the gastrointestinal symptom rating scale (GSRS) questionnaire. Arq Gastroenterol. 2016;53(3):146–51.
Blake MR, Raker JM, Whelan K. Validity and reliability of the bristol stool form scale in healthy adults and patients with diarrhoea-predominant irritable bowel syndrome. Aliment Pharmacol Ther. 2016;44(7):693–703.
Mufson L, Morrison C, Shea E, et al. Screening for depression with the PHQ-9 in young adults affected by HIV. J Affect Disord. 2022;297:276–82.
Toussaint A, Hüsing P, Gumz A, et al. Sensitivity to change and minimal clinically important difference of the 7-item generalized anxiety disorder questionnaire (GAD-7). J Affect Disord. 2020;265:395–401.
Chang L, Wei Y, Hashimoto K. Brain-gut-microbiota axis in depression: a historical overview and future directions. Brain Res Bull. 2022;182:44–56.
Farshbafnadi M, Agah E, Rezaei N. The second brain: the connection between gut microbiota composition and multiple sclerosis. J Neuroimmunol. 2021;360: 577700.
Yue Q, Cai M, **ao B, et al. The microbiota-gut-brain axis and epilepsy. Cell Mol Neurobiol. 2022;42(2):439–53.
Li X, Kan EM, Lu J, et al. Combat-training increases intestinal permeability, immune activation and gastrointestinal symptoms in soldiers. Aliment Pharmacol Ther. 2013;37(8):799–809.
Jowett SL, Seal CJ, Pearce MS, et al. Influence of dietary factors on the clinical course of ulcerative colitis: a prospective cohort study. Gut. 2004;53(10):1479–84.
Hey H, Schmedes A, Nielsen AA, et al. Effects of five different alcoholic drinks on patients with Crohn’s disease. Scand J Gastroenterol. 2007;42(8):968–72.
Abanes J, Hiers C, Rhoten B, et al. Feasibility and acceptability of a brief acupuncture intervention for service members with perceived stress. Mil Med. 2020;185(1–2):e17–22.
Bulmer S, Drain JR, Tait JL, et al. Quantification of recruit training demands and subjective wellbeing during basic military training. Int J Environ Res Public Health. 2022;19(12).
Chasiropoulou C, Siouti N, Mougiakos T, et al. The diathesis-stress model in the emergence of major psychiatric disorders during military service. Psychiatriki. 2019;30(4):291–8.
Yu XZ, Liu HF, Sun ZX. Investigation of the effect of military stress on the prevalence of functional bowel disorders. World J Gastroenterol. 2012;18(23):3004–7.
Acknowledgements
We thank all the researchers and participants who have participated in this study.
Funding
No funding or sponsorship was received for this study or publication of this article.
Author information
Authors and Affiliations
Contributions
Conception and design: Tingwei Liu, **ngshun Qi, and Jun Liu; Administrative support: **ngshun Qi; Provision of study materials or patients: Jun Liu; Collection and assembly of data: Tingwei Liu and Jun Liu; Data analysis and interpretation: Tingwei Liu, Shaoze Ma, Xueying Wang, and **ngshun Qi; Manuscript writing: All authors; Final approval of manuscript: All authors. All authors have made an intellectual contribution to the manuscript and approved the submission.
Corresponding author
Ethics declarations
Conflict of Interest
Tingwei Liu, Jun Liu, Shaoze Ma, Xueying Wang and **aozhong Guo. **ngshun Qi is an editorial board member of the journal Advances in Therapy. **ngshun Qi was not involved in the selection of peer reviewers for the manuscript nor any of the subsequent editorial decisions.
Ethical Approval
This is a cross-sectional study conducted based on the data from a prospective study, which had been approved by the Medical Ethical Committee of the General Hospital of Northern Theater Command with an ethical approval number [Y (2022) 014].
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, T., Liu, J., Ma, S. et al. Association of Gastrointestinal Symptoms with Depression and Anxiety in Recruits: A Validation Cross-Sectional Study. Adv Ther (2024). https://doi.org/10.1007/s12325-024-02911-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12325-024-02911-z