Abstract
Purpose
This study aimed to assess the impact of biodegradable polyurethane meniscus scaffold implantation (BPMSI) on muscle strength and balance in comparison with the healthy contralateral knee in patients with irreparable medial meniscus defect.
Methods
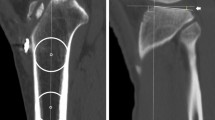
This observational and prospective case-cohort study was conducted with patients who had irreparable meniscal defects and underwent arthroscopic meniscus scaffold implantation. Surgeries were carried out on the medial meniscus of 16 right and 4 left knees. Visual analog scale (VAS) was used to assess the degree of pain relief. Knee Injury and Osteoarthritis Outcome Score (KOOS) and Lysholm (LYS) score were used to evaluate the functional improvement at weeks 12, 24 and 36. Concentric and eccentric quadriceps and hamstring peak torque (PT) as well as the peak torque-to-body weight (PTB) ratio, anterior–posterior, mediolateral and overall stability indexes were assessed at the same time points.
Results
Twenty male patients with a mean age and body mass index of 32.2 ± 8.8 years and 26.2 ± 4.2 kg/m2, respectively, were included in the study. The amount of pain decreased from 7.6 ± 1.5% to 2.9 ± 1.5% at postoperative week 36. Range of motion, Lysholm score and KOOS increased from 87.0ο ± 9.5ο to 115.0ο ± 15.1ο, 30.8 ± 4.3 to 81.5 ± 5.3 and 37.4 ± 5.3 to 74.1 ± 7.2, respectively. Concentric quadriceps and hamstring peak torque values and peak torque/body weight ratios were improved in the knees that received a meniscus scaffold implant. Anterior/posterior, medial/lateral, and overall stability indexes with or without biofeedback exhibited a slight improvement, which was not statistically significant.
Conclusion
BPMSI led to decreased pain and improved function at postoperative week 36. Although muscle strength almost returned to normal, balance parameters did not recover within 36 weeks after the procedure.




Similar content being viewed by others
References
Papalia R et al (2013) Scaffolds for partial meniscal replacement: an updated systematic review. Br Med Bull 107:19–40
Vrancken AC, Buma P, van Tienen TG (2013) Synthetic meniscus replacement: a review. Int Orthop 37(2):291–299
Kaleka CC et al (2014) Updates in biological therapies for knee injuries: menisci. Curr Rev Musculoskelet Med 7(3):247–255
Moran CJ et al (2015) Clinical application of scaffolds for partial meniscus replacement. Sports Med Arthrosc 23(3):156–161
Efe T et al (2012) The safety and short-term efficacy of a novel polyurethane meniscal scaffold for the treatment of segmental medial meniscus deficiency. Knee Surg Sports Traumatol Arthrosc 20(9):1822–1830
Spencer SJ et al (2012) Meniscal scaffolds: early experience and review of the literature. Knee 19(6):760–765
Kon E et al (2014) Biodegradable polyurethane meniscal scaffold for isolated partial lesions or as combined procedure for knees with multiple comorbidities: clinical results at 2 years. Knee Surg Sports Traumatol Arthrosc 22(1):128–134
Bulgheroni E et al (2016) Comparative Study of Collagen versus Synthetic-Based Meniscal Scaffolds in Treating Meniscal Deficiency in Young Active Population. Cartilage 7(1):29–38
Bulgheroni P et al (2013) Polyurethane scaffold for the treatment of partial meniscal tears. Clinical results with a minimum two-year follow-up. Joints 1(4):161–166
Leroy A et al (2015) PLA-poloxamer/poloxamine copolymers for ligament tissue engineering: sound macromolecular design for degradable scaffolds and MSC differentiation. Biomater Sci 3(4):617–626
Leroy A et al (2017) Actifit(R) polyurethane meniscal scaffold: MRI and functional outcomes after a minimum follow-up of 5 years. Orthop Traumatol Surg Res 103(4):609–614
Schuttler KF et al (2015) Improvement in outcomes after implantation of a novel polyurethane meniscal scaffold for the treatment of medial meniscus deficiency. Knee Surg Sports Traumatol Arthrosc 23(7):1929–1935
Schuttler KF et al (2016) Midterm follow-up after implantation of a polyurethane meniscal scaffold for segmental medial meniscus loss: maintenance of good clinical and MRI outcome. Knee Surg Sports Traumatol Arthrosc 24(5):1478–1484
Verdonk R et al (2011) Tissue ingrowth after implantation of a novel, biodegradable polyurethane scaffold for treatment of partial meniscal lesions. Am J Sports Med 39(4):774–782
Verdonk P et al (2012) Successful treatment of painful irreparable partial meniscal defects with a polyurethane scaffold: two-year safety and clinical outcomes. Am J Sports Med 40(4):844–853
Bouyarmane H et al (2014) Polyurethane scaffold in lateral meniscus segmental defects: clinical outcomes at 24 months follow-up. Orthop Traumatol Surg Res 100(1):153–157
Dhollander A, Verdonk P, Verdonk R (2016) Treatment of painful, irreparable partial meniscal defects with a polyurethane scaffold: midterm clinical outcomes and survival analysis. Am J Sports Med 44(10):2615–2621
Baynat C et al (2014) Actifit synthetic meniscal substitute: experience with 18 patients in Brest, France. Orthop Traumatol Surg Res 100(8 Suppl):S385–S389
Brophy RH, Matava MJ (2012) Surgical options for meniscal replacement. J Am Acad Orthop Surg 20(5):265–272
Gelber PE et al (2015) The magnetic resonance aspect of a polyurethane meniscal scaffold is worse in advanced cartilage defects without deterioration of clinical outcomes after a minimum two-year follow-up. Knee 22(5):389–394
Vrancken AC et al (2016) Functional biomechanical performance of a novel anatomically shaped polycarbonate urethane total meniscus replacement. Knee Surg Sports Traumatol Arthrosc 24(5):1485–1494
Vaquero J, Forriol F (2016) Meniscus tear surgery and meniscus replacement. Muscles Ligaments Tendons J 6(1):71–89
Leroy A et al (2017) Actifit((R)) polyurethane meniscal scaffold: MRI and functional outcomes after a minimum follow-up of 5 years. Orthop Traumatol Surg Res 103(4):609–614
Shin YS et al (2018) Polyurethane meniscal scaffolds lead to better clinical outcomes but worse articular cartilage status and greater absolute meniscal extrusion. Knee Surg Sports Traumatol Arthrosc 26(8):2227–2238
Filardo G et al (2017) Polyurethane-based cell-free scaffold for the treatment of painful partial meniscus loss. Knee Surg Sports Traumatol Arthrosc 25(2):459–467
De Coninck T et al (2014) In-vivo evaluation of the kinematic behavior of an artificial medial meniscus implant: a pilot study using open-MRI. Clin Biomech (Bristol, Avon) 29(8):898–905
Condello V et al (2019) Polyurethane scaffold implants for partial meniscus lesions: delayed intervention leads to an inferior outcome. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-019-05760-4
Nelson WE et al (1996) Isokinetic strength following knee arthroscopy. Orthopedics 19(6):501–504
Stensrud S, Risberg MA, Roos EM (2015) Effect of exercise therapy compared with arthroscopic surgery on knee muscle strength and functional performance in middle-aged patients with degenerative meniscus tears: a 3-mo follow-up of a randomized controlled trial. Am J Phys Med Rehabil 94(6):460–473
Houck DA et al (2018) Similar clinical outcomes following collagen or polyurethane meniscal scaffold implantation: a systematic review. Knee Surg Sports Traumatol Arthrosc 26(8):2259–2269
Mueller BT et al (2016) Rehabilitation following meniscal root repair: a clinical commentary. J Orthop Sports Phys Ther 46(2):104–113
Ganderup T et al (2017) Recovery of lower extremity muscle strength and functional performance in middle-aged patients undergoing arthroscopic partial meniscectomy. Knee Surg Sports Traumatol Arthrosc 25(2):347–354
Ericsson YB, Roos EM, Dahlberg L (2006) Muscle strength, functional performance, and self-reported outcomes four years after arthroscopic partial meniscectomy in middle-aged patients. Arthritis Rheum 55(6):946–952
Hall M et al (2015) Knee extensor muscle strength in middle-aged and older individuals undergoing arthroscopic partial meniscectomy: a systematic review and meta-analysis. Arthritis Care Res (Hoboken) 67(9):1289–1296
Hall M et al (2013) A longitudinal study of strength and gait after arthroscopic partial meniscectomy. Med Sci Sports Exerc 45(11):2036–2043
Karahan M et al (2010) Effect of partial medial meniscectomy on the proprioceptive function of the knee. Arch Orthop Trauma Surg 130(3):427–431
Malliou P et al (2012) Proprioception and functional deficits of partial meniscectomized knees. Eur J Phys Rehabil Med 48(2):231–236
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Akkaya, M., Gursoy, S., Ozberk, N. et al. Muscle strength but not balance improves after arthroscopic biodegradable polyurethane meniscus scaffold application. Musculoskelet Surg 106, 145–153 (2022). https://doi.org/10.1007/s12306-020-00681-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12306-020-00681-9