Abstract
Tuberculosis (TB) has remained a global health challenge despite the availability of effective anti-tubercular drugs and various treatment strategies. Apart from the complications related to TB disease per se, adverse effects of antitubercular therapy (ATT) also contribute to morbidity. In addition to the adverse effects, the long duration of the treatment regimen also reduces the patient’s acceptability of ATT. The available “short-course treatment regimens” are still relatively long, thereby adversely affecting treatment compliance. There is a need for effective, safe, short and intensive regimens for TB which can reduce the treatment cost and adverse effects, thereby improving its acceptance. With the emergence of new evidence, the World Health Organization (WHO) has recently endorsed 4 mo short duration ATT regimen for non-severe, drug-sensitive cases of tuberculosis. Even in severe forms of disease like tubercular meningitis (TBM), trials are underway evaluating efficacy and safety of shorter regimens. Inclusion of fluroquinolones and rifapentine help shorten the regimens. These shortened regimens, however, need more close monitoring for adverse effects and may need to be converted to longer course if there is inadequate clinical response. Thus, shorter regimens for pediatric TB are likely to not only decrease the burden on patients and healthcare but also improve compliance and lower the side effects of the drugs due to prolonged exposure. This article reviews the current evidence and the guidelines pertaining to the shortened, intensive regimens for drug-sensitive tuberculosis.
Similar content being viewed by others
References
WHO Operational Handbook on Tuberculosis. Module 5: Management of Tuberculosis in Children and Adolescents [Internet]. Available at: https://www.who.int/publications/i/item/9789240046832. Accessed on 16 Aug 2023.
Guidelines on Pediatric TB: Central TB Division [Internet]. Available at: https://tbcindia.gov.in/index1.php?lang=1&level=2&sublinkid=4200&lid=2848. Accessed on 16 Aug 2023.
World Health Organization. – 2017 - Guidelines for Treatment of Drug-Susceptible Tuberculosis and Patient Care.pdf [Internet]. Available at: https://apps.who.int/iris/bitstream/handle/10665/255052/9789241550000-eng.pdf. Accessed on 17 Aug 2023.
Grace AG, Mittal A, Jain S, et al. Shortened treatment regimens versus the standard regimen for drug-sensitive pulmonary tuberculosis. Cochrane Database Syst Rev. 2019;12:CD012918.
Chiang SS, Khan FA, Milstein MB, et al. Treatment outcomes of childhood tuberculous meningitis: a systematic review and meta-analysis. Lancet Infect Dis. 2014;14:947–57.
Peloquin C. What is the right dose of rifampin? Int J Tuberc Lung Dis. 2003;7:3–5.
Svensson EM, Svensson RJ, Te Brake LHM, et al. The potential for treatment shortening with higher rifampicin doses: relating drug exposure to treatment response in patients with pulmonary tuberculosis. Clin Infect Dis. 2018;67:34–41.
Trébucq A, Schwoebel V, Kashongwe Z, et al. Treatment outcome with a short multidrug-resistant tuberculosis regimen in nine African countries. Int J Tuberc Lung Dis. 2018;22:17–25.
Tang S, Yao L, Hao X, et al. Clofazimine for the treatment of multidrug-resistant tuberculosis: prospective, multicenter, randomized controlled study in China. Clin Infect Dis. 2015;60:1361–7.
Grosset JH, Tyagi S, Almeida DV, et al. Assessment of clofazimine activity in a second-line regimen for tuberculosis in mice. Am J Respir Crit Care Med. 2013;188:608–12.
Ammerman NC, Swanson RV, Bautista EM, et al. Impact of clofazimine dosing on treatment shortening of the first-line regimen in a mouse model of tuberculosis. Antimicrob Agents Chemother. 2018;62:e00636–18.
Saini V, Ammerman NC, Chang YS, et al. Treatment-shortening effect of a novel regimen combining clofazimine and high-dose rifapentine in pathologically distinct mouse models of tuberculosis. Antimicrob Agents Chemother. 2019;63:e00388-19.
Dalcolmo M, Gayoso R, Sotgiu G, et al. Effectiveness and safety of clofazimine in multidrug-resistant Tuberculosis: a nationwide report from Brazil. Eur Respir J. 2017;49:1602445.
Sotgiu G, Centis R, D’Ambrosio L, et al. Efficacy, safety and tolerability of linezolid containing regimens in treating MDR-TB and XDR-TB: systematic review and meta-analysis. Eur Respir J. 2012;40:1430–42.
Centers for Disease Control and Prevention., 2023. Tuberculosis (TB) - Treatment for TB Disease. Available at: https://www.cdc.gov/tb/topic/treatment/tbdisease.htm. Accessed on 16 Aug 2023.
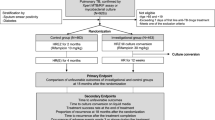
Turkova A, Wills GH, Wobudeya E, et al; SHINE Trial Team. Shorter treatment for nonsevere Tuberculosis in African and Indian children. N Engl J Med. 2022;386:911–22.
Dorman SE, Nahid P, Kurbatova EV, et al. Four-month rifapentine regimens with or without moxifloxacin for tuberculosis. N Engl J Med. 2021;384:1705–18.
Muniyandi M, Karikalan N, Velayutham B, Rajsekar K, Padmapriyadarsini C. Cost effectiveness of a shorter moxifloxacin based regimen for treating drug sensitive tuberculosis in India. Trop Med Infect Dis. 2022;7:288.
van Toorn R, Schaaf HS, Laubscher JA, van Elsland SL, Donald PR, Schoeman JF. Short intensified treatment in children with drug-susceptible tuberculous meningitis. Pediatr Infect Dis J. 2014;33:248–52.
van Well GTJ, Paes BF, Terwee CB, et al. Twenty years of pediatric tuberculous meningitis: a retrospective cohort study in the western cape of South Africa. Pediatrics. 2009;123:e1-8.
Sulis G, Tavaziva G, Gore G, et al. Comparative effectiveness of regimens for drug-susceptible tuberculous meningitis in children and adolescents: a systematic review and aggregate-level data meta-analysis. Open Forum Infect Dis. 2022;9:ofac108.
ISRCTN - ISRCTN40829906. SURE: Short Intensive Treatment for Children with tuberculous meningitis. Available at: https://www.isrctn.com/ISRCTN40829906. Accessed on 16 Aug 2023.
Muniyandi M, Thomas BE, Karikalan N, et al. Association of Tuberculosis with household catastrophic expenditure in South India. JAMA Netw Open. 2020;3:e1920973.
Author information
Authors and Affiliations
Contributions
KKS: Finding relevant articles, review of articles, development of the manuscript and integration of information; MS: Compiling relevant articles, review of articles and participation in the development of the manuscript. KKS will act as the guarantor for this manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Singhal, K.K., Shinde, M. Shortened Treatment Regimens for Drug Sensitive TB. Indian J Pediatr 91, 724–729 (2024). https://doi.org/10.1007/s12098-023-04943-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-023-04943-9