Abstract
Objectives
To examine the feasibility, efficacy, and safety of sustained low-efficiency dialysis (SLED) in hemodynamically unstable, critically ill children.
Methods
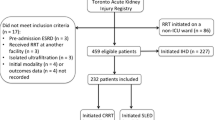
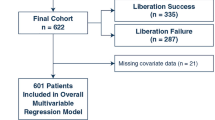
Critically ill patients, 1–18 y old with hemodynamic instability (≥ 1 vasoactive drugs) and severe acute kidney injury (AKI) requiring kidney replacement therapy (KRT) in a tertiary care pediatric intensive care unit were prospectively enrolled. Patients weighing ≤ 8 kg or with mean arterial pressure < 5th percentile despite > 3 vasoactive drugs, were excluded. Patients underwent SLED until hemodynamically stable and off vasoactive drugs, or lack of need for dialysis. The primary outcome was the proportion of patients in whom the first session of SLED was initiated within 12 h of its indication and completed without premature (< 6 h) termination. Efficacy was estimated by ultrafiltration, urea reduction ratio (URR), and equilibrated Kt/V. Other outcomes included: changes in hemodynamic scores, circuit clotting, adverse events, and changes in indices on point-of-care ultrasonography and echocardiography.
Results
Between November 2018 and March 2020, 18 patients with median age 8.6 y and vasopressor dependency index of 83.2, underwent 41 sessions of SLED. In 16 patients, SLED was feasible within 12 h of indication. No session was terminated prematurely. Ultrafiltration achieved was 4.0 ± 2.2 mL/kg/h, while URR was 57.7 ± 16.2% and eKt/V 1.17 ± 0.56. Hemodynamic scores did not change significantly. Asymptomatic hypokalemia was the chief adverse effect. Sessions were associated with a significant improvement in indices on ultrasound and left ventricular function. Fourteen patients died.
Conclusions
SLED is feasible, safe, and effective in enabling KRT in hemodynamically unstable children with severe AKI.

Similar content being viewed by others
References
Mehta P, Sinha A, Sami A, et al. Incidence of acute kidney injury in hospitalized children. Indian Pediatr. 2012;49:537–42.
Roy JP, Devarajan P. Acute kidney injury: diagnosis and management. Indian J Pediatr. 2020;87:600–7.
Sethi SK, Mittal A, Nair N, et al. Pediatric Continuous Renal Replacement Therapy (PCRRT) expert committee recommendation on prescribing prolonged intermittent renal replacement therapy (PIRRT) in critically ill children. Hemodial Int. 2020;24:237–51.
Lee CY, Yeh HC, Lin CY. Treatment of critically ill children with kidney injury by sustained low-efficiency daily diafiltration. Pediatr Nephrol. 2012;27:2301–9.
Sethi SK, Bansal SB, Khare A, et al. Heparin free dialysis in critically sick children using sustained low efficiency dialysis (SLEDD-f): A new hybrid therapy for dialysis in develo** world. PLOS One. 2018;13:e0195536.
Sethi SK, Sinha R, Jha P, et al. Feasibility of sustained low efficiency dialysis in critically sick pediatric patients: A multicentric retrospective study. Hemodial Int. 2018;22:228–34.
Marshall MR, Ma T, Galler D, Rankin AP, Williams AB. Sustained low-efficiency daily diafiltration (SLEDD-f) for critically ill patients requiring renal replacement therapy: towards an adequate therapy. Nephrol Dial Transplant. 2004;19:877–84.
Abe M, Okada K, Suzuki M, et al. Comparison of sustained hemodiafiltration with continuous venovenous hemodiafiltration for the treatment of critically ill patients with acute kidney injury. Artif Organs. 2010;34:331–8.
Abe M, Maruyama N, Matsumoto S, et al. Comparison of sustained hemodiafiltration with acetate-free dialysate and continuous venovenous hemodiafiltration for the treatment of critically ill patients with acute kidney injury. Int J Nephrol. 2011;2011:432094.
Basu RK, Zappitelli M, Brunner L, et al. Derivation and validation of the renal angina index to improve the prediction of acute kidney injury in critically ill children. Kidney Int. 2014;85:659–67.
Davis AL, Carcillo JA, Aneja RK, et al. American college of critical care medicine clinical practice parameters for hemodynamic support of pediatric and neonatal septic shock. Crit Care Med. 2017;45:1061–93.
Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315:801–10.
Bouchard J, Soroko SB, Chertow GM, et al. Program to Improve Care in Acute Renal Disease (PICARD) Study Group. Fluid accumulation, survival and recovery of kidney function in critically ill patients with acute kidney injury. Kidney Int. 2009;76:422–7.
Gaudry S, Hajage D, Schortgen F, et al. AKIKI Study Group. Initiation strategies for renal-replacement therapy in the intensive care unit. N Engl J Med. 2016;375:122–33.
Lobo V. Sustained Low-Efficiency Dialysis (SLED) and Hybrid Therapies in Children. In: Deep A, Goldstein SL, editors. Critical Care Nephrology and Renal Replacement Therapy in Children. Cham: Springer International Publishing; 2018. p. 291–306.
Kramer H, Yee J, Weiner DE, et al. Ultrafiltration rate thresholds in maintenance hemodialysis: An NKF-KDOQI controversies report. Am J Kidney Dis. 2016;68:522–32.
Mushatt DM, Mihm LB, Dreisbach AW, Simon EE. Antibiotic dosing in slow extended daily dialysis. Clin Infect Dis. 2009;49:433–7.
Schwartz GJ, Muñoz A, Schneider MF, et al. New equations to estimate GFR in children with CKD. J Am Soc Nephrol. 2009;20:629–37.
Tattersall JE, DeTakats D, Chamney P, Greenwood RN, Farrington K. The post-hemodialysis rebound: predicting and quantifying its effect on Kt/V. Kidney Int. 1996;50:2094–102.
Daugirdas JT. Physiologic principles and urea kinetic modeling. In: Daugirdas JT, Blake PG, Ing TS, editors. Handbook of dialysis, Fifth Edition. Philadelphia, PA:Wolters Kluwer Health; 2015;34–65.
Mishra SB, Azim A, Prasad N, et al. A pilot randomized controlled trial of comparison between extended daily hemodialysis and continuous veno-venous hemodialysis in patients of acute kidney injury with septic shock. Indian J Crit Care Med. 2017;21:262–7.
Chacko J, Brar G. Bedside ultrasonography: Applications in critical care: Part I. Indian J Crit Care Med. 2014;18:301–9.
Furtado S, Reis L. Inferior vena cava evaluation in fluid therapy decision making in intensive care: practical implications. Rev Bras Ter Intensiva. 2019;31:240–7.
Ostermann M, Bellomo R, Burdmann EA, et al. Controversies in acute kidney injury: conclusions from a kidney disease: improving global outcomes (KDIGO) conference. Kidney Int. 2020;98:294–309.
Kellum JA, Lameire N. KDIGO AKI Guideline Work Group. Diagnosis, evaluation, and management of acute kidney injury: a KDIGO summary (Part 1). Crit Care. 2013;17:204.
WHO. Application tools: WHO AnthroPlus software. Available at: http://www.who.int/growthref/tools/en/. Accessed on 11 Nov 2021.
Zhang L, Yang J, Eastwood GM, Zhu G, Tanaka A, Bellomo R. Extended daily dialysis versus continuous renal replacement therapy for acute kidney injury: a meta-analysis. Am J Kidney Dis. 2015;66:322–30.
Nash DM, Przech S, Wald R, O’Reilly D. Systematic review and meta-analysis of renal replacement therapy modalities for acute kidney injury in the intensive care unit. J Crit Care. 2017;41:138–44.
Ali US, Arya MK. Efficacy and safety of prolonged daily hemodialysis in critically ill children weighing less than 10 kg. Hemodial Int. 2020;24:108–13.
Messmer AS, Zingg C, Müller M, Gerber JL, Schefold JC, Pfortmueller CA. Fluid overload and mortality in adult critical care patients-a systematic review and meta-analysis of observational studies. Crit Care Med. 2020;48:1862–70.
Zhang L, Chen Z, Diao Y, Yang Y, Fu P. Associations of fluid overload with mortality and kidney recovery in patients with acute kidney injury: a systematic review and meta-analysis. J Crit Care. 2015;30:860.
VA/NIH Acute Renal Failure Trial Network, Palevsky PM, Zhang JH, O’Connor TZ, et al. Intensity of renal support in critically ill patients with acute kidney injury. N Engl J Med. 2008;359:7–20.
Douvris A, Malhi G, Hiremath S, et al. Interventions to prevent hemodynamic instability during renal replacement therapy in critically ill patients: a systematic review. Crit Care. 2018;22:41.
Acknowledgements
The authors acknowledge the commitment and support of the nursing staff of pediatric hemodialysis and intensive care units.
Funding
The Indian Council of Medical Research provided funding to the Advanced Center for Research in Pediatric Kidney Diseases, Division of Nephrology, Department of Pediatrics, AIIMS [5/7/1090/2013-RHN].
Author information
Authors and Affiliations
Contributions
MY made substantial contribution to the acquisition, analysis, and interpretation of data and drafted the manuscript; ANT and PK helped in clinical work; ANT supervised dialysis sessions; AS, PH, JS, RL, and AB made substantial contributions to the conception and design of the work; revised the work critically for important intellectual content. AB will act as the guarantor for this paper.
Corresponding author
Ethics declarations
Ethics Approval
Institute Ethics Committee, All India Institute of Medical Sciences, Ansari Nagar, New Delhi; IECPG-465/27.09.2018, RT-12/18.10.2018/RT-5/14.11.2018.
Conflict of Interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yadav, M., Tiwari, A.N., Lodha, R. et al. Feasibility and Efficacy of Sustained Low-Efficiency Dialysis in Critically Ill Children with Severe Acute Kidney Injury. Indian J Pediatr 90, 355–361 (2023). https://doi.org/10.1007/s12098-022-04214-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12098-022-04214-z