Abstract
Background
Life-threatening, space-occupying mass effect due to cerebral edema and/or hemorrhagic transformation is an early complication of patients with middle cerebral artery stroke. Little is known about longitudinal trajectories of laboratory and vital signs leading up to radiographic and clinical deterioration related to this mass effect.
Methods
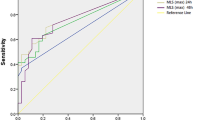
We curated a retrospective data set of 635 patients with large middle cerebral artery stroke totaling 95,463 data points for 10 longitudinal covariates and 40 time-independent covariates. We assessed trajectories of the 10 longitudinal variables during the 72 h preceding three outcomes representative of life-threatening mass effect: midline shift ≥ 5 mm, pineal gland shift (PGS) > 4 mm, and decompressive hemicraniectomy (DHC). We used a “backward-looking” trajectory approach. Patients were aligned based on outcome occurrence time and the trajectory of each variable was assessed before that outcome by accounting for cases and noncases, adjusting for confounders. We evaluated longitudinal trajectories with Cox proportional time-dependent regression.
Results
Of 635 patients, 49.0% were female, and the mean age was 69 years. Thirty five percent of patients had midline shift ≥ 5 mm, 24.3% of patients had PGS > 4 mm, and 10.7% of patients underwent DHC. Backward-looking trajectories showed mild increases in white blood cell count (10–11 K/UL within 72 h), temperature (up to half a degree within 24 h), and sodium levels (1–3 mEq/L within 24 h) before the three outcomes of interest. We also observed a decrease in heart rate (75–65 beats per minute) 24 h before DHC. We found a significant association between increased white blood cell count with PGS > 4 mm (hazard ratio 1.05, p value 0.007).
Conclusions
Longitudinal profiling adjusted for confounders demonstrated that white blood cell count, temperature, and sodium levels appear to increase before radiographic and clinical indicators of space-occupying mass effect. These findings will inform the development of multivariable dynamic risk models to aid prediction of life-threatening, space-occupying mass effect.




Similar content being viewed by others
References
Wu S, Yuan R, Wang Y, et al. Early prediction of malignant brain edema after ischemic stroke. Stroke. 2018;49(12):2918–27.
Miao J, Song X, Sun W, Qiu X, Lan Y, Zhu Z. Predictors of malignant cerebral edema in cerebral artery infarction: a meta-analysis. J Neurol Sci. 2020;409:116607. https://doi.org/10.1016/j.jns.2019.116607.
Ong CJ, Gluckstein J, Laurido-Soto O, Yan Y, Dhar R, Lee JM. Enhanced detection of edema in malignant anterior circulation stroke (EDEMA) score: a risk prediction tool. Stroke. 2017;48(7):1969–72.
Shimoyama T, Kimura K, Uemura J, et al. The DASH score: a simple score to assess risk for development of malignant middle cerebral artery infarction. J Neurol Sci. 2014;338(1–2):102–6.
Huang X, Chen C, Wang H, et al. The ACORNS grading scale: a novel tool for the prediction of malignant brain edema after endovascular thrombectomy. J Neurointerv Surg. 2023;15(e2):e190–7. https://doi.org/10.1136/jnis-2022-019404.
Gerriets T, Stolz E, Konig S, et al. Sonographic monitoring of midline shift in space-occupying stroke: an early outcome predictor. Stroke. 2001;32(2):442–7. https://doi.org/10.1161/01.str.32.2.442.
Kimberly WT, Dutra BG, Boers AMM, et al. Association of reperfusion with brain edema in patients with acute ischemic stroke: a secondary analysis of the MR CLEAN trial. JAMA Neurol. 2018;75(4):453–61. https://doi.org/10.1001/jamaneurol.2017.5162.
McKeown MEPA, Kobsa J, Top I, Snider SB, Kidwell C, Campbell BCV, Davis SM, Donnan GA, Lev M, Sheth KN, Petersen N, Kimberly WT, Bevers MB. Midline shift greater than 3 mm independently predicts outcome after ischemic stroke. Neurocrit Care. 2022;36(1):46–51.
Pullicino PM, Alexandrov AV, Shelton JA, Alexandrova NA, Smurawska LT, Norris JW. Mass effect and death from severe acute stroke. Neurology. 1997;49(4):1090–5. https://doi.org/10.1212/wnl.49.4.1090.
Huang X, Liu L, Ning J, Li L, Shen Y. Estimation of the distribution of longitudinal biomarker trajectories prior to disease progression. Stat Med. 2019;38(11):2030–46. https://doi.org/10.1002/sim.8085.
Ong C, Zhang R, Orfanoudaki A, et al. New methods of natural language processing using machine learning methods to identify ischemic stroke presence, acuity, and location from clinical radiology reports. In: Machine learning for healthcare. Ann Arbor, MI; 2019.
Kasner SE, Chalela JA, Luciano JM, et al. Reliability and validity of estimating the NIH stroke scale score from medical records. Stroke. 1999;30(8):1534–7. https://doi.org/10.1161/01.str.30.8.1534.
Jauch EC, Saver JL, Adams HP Jr, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2013;44(3):870–947. https://doi.org/10.1161/STR.0b013e318284056a.
Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American heart association/American stroke association. Stroke. 2019;50(12):e344–418. https://doi.org/10.1161/STR.0000000000000211.
Yarbrough CK, Ong CJ, Beyer AB, Lipsey K, Derdeyn CP. Endovascular thrombectomy for anterior circulation stroke: systematic review and meta-analysis. Stroke. 2015;46(11):3177–83.
Nogueira RG, Jadhav AP, Haussen DC, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018;378(1):11–21. https://doi.org/10.1056/NEJMoa1706442.
Albers GW, Marks MP, Kemp S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018;378(8):708–18. https://doi.org/10.1056/NEJMoa1713973.
Hofmeijer J, Kappelle LJ, Algra A, et al. Surgical decompression for space-occupying cerebral infarction (the hemicraniectomy after middle cerebral artery infarction with life-threatening edema trial [HAMLET]): a multicentre, open, randomised trial. Lancet Neurol. 2009;8(4):326–33.
Juttler E, Schwab S, Schmiedek P, et al. Decompressive surgery for the treatment of malignant infarction of the middle cerebral artery (DESTINY): a randomized, controlled trial. Stroke. 2007;38(9):2518–25.
Juttler E, Unterberg A, Woitzik J, et al. Hemicraniectomy in older patients with extensive middle-cerebral-artery stroke. N Engl J Med. 2014;370(12):1091–100.
Vahedi K, Vicaut E, Mateo J, et al. Sequential-design, multicenter, randomized, controlled trial of early decompressive craniectomy in malignant middle cerebral artery infarction (DECIMAL Trial). Stroke. 2007;38(9):2506–17.
Ropper AH. Lateral displacement of the brain and level of consciousness in patients with an acute hemispheral mass. N Engl J Med. 1986;314(15):953–8.
Carney N, Totten AM, O’Reilly C, et al. Guidelines for the management of severe traumatic brain injury, fourth edition. Neurosurgery. 2017;80(1):6–15. https://doi.org/10.1227/NEU.0000000000001432.
Kim ISY, Balogun OO, Prescott BR, et al. Quantitative pupillometry and radiographic markers of intracranial midline shift: a pilot study. Front Neurol. 2022;13:1046548. https://doi.org/10.3389/fneur.2022.1046548.
Aalen OO, Johansen S. An empirical transition matrix for non-homogeneous Markov chains based on censored observations. Scand J Stat. 1978;5(3):141–50.
Cheng Y, Wu S, Wang Y, et al. External validation and modification of the EDEMA score for predicting malignant brain edema after acute ischemic stroke. Neurocrit Care. 2020;32(1):104–12. https://doi.org/10.1007/s12028-019-00844-y.
Hofmeijer J, Algra A, Kappelle LJ, van der Worp HB. Predictors of life-threatening brain edema in middle cerebral artery infarction. Cerebrovasc Dis. 2008;25(1–2):176–84. https://doi.org/10.1159/000113736.
Conner SCLS, Lunetta KL, Casas JP, Lubitz SA, Ellinor PT, Anderson CD, Huang Q, Coleman J, White WB, Benjamin EJ, Trinquart L. Refining the association between body mass index and atrial fibrillation: G-formula and restricted mean survival times. J Am Heart Assoc. 2019;8(16):e013011.
Zhang Z, Reinikainen J, Adeleke KA, Pieterse ME, Groothuis-Oudshoorn CGM. Time-varying covariates and coefficients in Cox regression models. Ann Transl Med. 2018;6(7):121. https://doi.org/10.21037/atm.2018.02.12.
Grady PA, Blaumanis OR. Physiologic parameters of the Cushing reflex. Surg Neurol. 1988;29(6):454–61. https://doi.org/10.1016/0090-3019(88)90140-1.
Funding
CJO receives support from NIH/NINDS K23NS116033; American Heart Association 23CDA1041762. EJB receives support from R01HL092577; American Heart Association AF AHA 18SFRN34110082. LT receives support from AHA 18SFRN34150007. DMG receives support from R01 NS102574. SMS receives support from RO1 EY024019.
Author information
Authors and Affiliations
Contributions
CJO, QH, DMG, and SMS conceived the idea of the presented analyses and designed the overall study. JP, IK, and YZ organized and collected the patient data for analysis. IK, BB, CJO, SC, and LAM performed manual reviews of patient notes to extract various features such as stroke onset times, medications, procedures, and outcomes. BB developed algorithms for automated feature extraction from radiology reports. SC, BB, and CJO manually reviewed and radiographic images to measure swelling and determine radiographic outcomes. QH and JP performed statistical analysis, visualization, and interpretation. LT, EJB, and JD provided oversight and review of the statistical analysis. CJO and QH drafted the manuscript. QH, IK, YD, and LAM designed figures. SC, BB, LT, SMS, EJB, JD, and DMG helped with reviews and revisions. CJO provided overall study direction and critical review. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Conflicts of interest
The authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or nonfinancial interest in the subject matter or materials discussed in this article.
Ethical Approval/Informed Consent
The study was approved to be conducted by the Mass General Brigham Institutional Review Board (2017P002564). All methods were performed in accordance with the relevant guidelines and regulations set forth by the institutional review board. Because of the retrospective nature of the study, the Mass General Brigham Institutional Review Board waived the need of obtaining informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ong, C.J., Huang, Q., Kim, I.S.Y. et al. Association of Dynamic Trajectories of Time-Series Data and Life-Threatening Mass Effect in Large Middle Cerebral Artery Stroke. Neurocrit Care (2024). https://doi.org/10.1007/s12028-024-02036-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12028-024-02036-9