Abstract
Background
Electrographic seizures are frequent and associated with worse outcomes following traumatic brain injury (TBI). Despite this, the use of continuous electroencephalogram (cEEG) remains low. Our study describes cEEG usage and treatment dosing antiseizure medications (ASMs) in an international pediatric TBI population, hypothesizing that children monitored with cEEG have an increased rate of treatment ASMs because of electrographic seizure detection, compared with children who are not monitored with cEEG.
Methods
This subanalysis of the TBI cohort of the international PANGEA study included children, 7 days to 17 years of age, with acute neurological insults admitted to pediatric intensive care units. We analyzed demographics, injury severity, and therapies including prophylactic or treatment ASMs. We evaluated the relationships between cEEG use, seizure frequency, and receipt of treatment ASMs. \(\chi^{2}\) or Fisher’s exact test was used to analyze categorical variables, and the Kruskal–Wallis or Mann–Whitney U-test was used for continuous variables. Multivariable analysis for treatment ASM use was performed using logistic regression.
Results
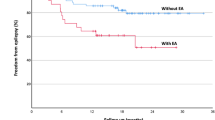
One hundred-twenty-three of 174 patients with TBI were included. Twenty-seven patients (21.9%) underwent cEEG at any point during pediatric intensive care unit admission. Preexisting seizure disorder (18.2% vs. 2.3%, p = 0.014) and neuromuscular blockade use (52.4% vs. 24.1%, p = 0.011) were more frequently observed in the group monitored on cEEG when compared with those that were not. Presenting median Glasgow Coma Scale score was worse in the cEEG group (7 vs. 9, p = 0.044). There was no significant difference in age, use of intracranial pressure monitoring, or hyperosmolar therapy between the cEEG monitored and nonmonitored groups. Patients who were monitored on cEEG were more likely to receive a treatment dose ASM than those without cEEG monitoring (66.7% vs. 28.1%, p = 0.0002). When compared with those without treatment ASM, the treatment ASM group had more electrographic seizures on their first electroencephalogram following injury (51.6% vs. 4%, p = 0.0001) and more clinical seizures (55.8% vs. 0%, p < 0.0001).
Conclusions
Children monitored with cEEG after TBI have an increased prescription of treatment ASMs and clinical and electrographic seizures. The increased rate of treatment ASMs in the cEEG group may indicate increased recognition of electrographic seizures.

Similar content being viewed by others
References
Bell MJ, Adelson PD, Wisniewski SR. Investigators of the AS. Challenges and opportunities for pediatric severe TBI-review of the evidence and exploring a way forward. Childs Nerv Syst. 2017;33:1663–7.
Stanley RM, Bonsu BK, Zhao W, Ehrlich PF, Rogers AJ, **ang H. US estimates of hospitalized children with severe traumatic brain injury: implications for clinical trials. Pediatrics. 2012;129:e24-30.
Dewan MC, Mummareddy N, Wellons JC, Bonfield CM. Epidemiology of global pediatric traumatic brain injury: qualitative review. World Neurosurg. 2016;91:497-509 e1.
Bean JR. Pediatric head injury: a global tragedy and a public policy challenge. World Neurosurg. 2016;91:618–9.
Arndt DH, Lerner JT, Matsumoto JH, et al. Subclinical early posttraumatic seizures detected by continuous EEG monitoring in a consecutive pediatric cohort. Epilepsia. 2013;54:1780–8.
Bennett KS, DeWitt PE, Harlaar N, Bennett TD. Seizures in children with severe traumatic brain injury. Pediatr Crit Care Med. 2017;18:54–63.
Liesemer K, Bratton SL, Zebrack CM, Brockmeyer D, Statler KD. Early post-traumatic seizures in moderate to severe pediatric traumatic brain injury: rates, risk factors, and clinical features. J Neurotrauma. 2011;28:755–62.
O’Neill BR, Handler MH, Tong S, Chapman KE. Incidence of seizures on continuous EEG monitoring following traumatic brain injury in children. J Neurosurg Pediatr. 2015;16:167–76.
Ruzas CM, DeWitt PE, Bennett KS, Chapman KE, Harlaar N, Bennett TD. EEG monitoring and antiepileptic drugs in children with severe TBI. Neurocrit Care. 2017;26:256–66.
Statler KD, Scheerlinck P, Pouliot W, Hamilton M, White HS, Dudek FE. A potential model of pediatric posttraumatic epilepsy. Epilepsy Res. 2009;86:221–3.
Rumalla K, Smith KA, Letchuman V, Gandham M, Kombathula R, Arnold PM. Nationwide incidence and risk factors for posttraumatic seizures in children with traumatic brain injury. J Neurosurg Pediatr. 2018;22:684–93.
Hill CE, Blank LJ, Thibault D, et al. Continuous EEG is associated with favorable hospitalization outcomes for critically ill patients. Neurology. 2019;92:e9–18.
Fink EL, Kochanek PM, Tasker RC, et al. International survey of critically Ill children with acute neurologic insults: the prevalence of acute critical neurological disease in children: a global epidemiological assessment study. Pediatr Crit Care Med. 2017;18:330–42.
Fiser DH. Assessing the outcome of pediatric intensive care. J Pediatr. 1992;121:68–74.
Slater A, Shann F, Pearson G. Paediatric index of mortality Study G. PIM2: a revised version of the Paediatric index of mortality. Intensive Care Med. 2003;29:278–85.
Schreiber JM, Zelleke T, Gaillard WD, Kaulas H, Dean N, Carpenter JL. Continuous video EEG for patients with acute encephalopathy in a pediatric intensive care unit. Neurocrit Care. 2012;17:31–8.
Barlow KM, Spowart JJ, Minns RA. Early posttraumatic seizures in non-accidental head injury: relation to outcome. Dev Med Child Neurol. 2000;42:591–4.
Vaewpanich J, Reuter-Rice K. Continuous electroencephalography in pediatric traumatic brain injury: Seizure characteristics and outcomes. Epilepsy Behav. 2016;62:225–30.
Kochanek PM, Wallisch JS, Bayir H, Clark RSB. Pre-clinical models in pediatric traumatic brain injury-challenges and lessons learned. Childs Nerv Syst. 2017;33:1693–701.
Sharma S, Tiarks G, Haight J, Bassuk AG. Neuropathophysiological mechanisms and treatment strategies for post-traumatic epilepsy. Front Mol Neurosci. 2021;14:612073.
Ostahowski PJ, Kannan N, Wainwright MS, et al. Variation in seizure prophylaxis in severe pediatric traumatic brain injury. J Neurosurg Pediatr. 2016;18:499–506.
Alkhamis F, Nazish S. Electroencephalographic grading of neuronal dysfunction in various etiologies of encephalopathy. Clin EEG Neurosci. 2020;51(6):420–5.
Funding
This study received no funding.
Author information
Authors and Affiliations
Contributions
Dr. Snooks conceptualized and designed the study, interpreted the data analysis, and drafted the initial article. Dr. Hanson, Dr. Farias-Moeller, and Dr. Fink participated in study design, data interpretation, and article revisions. Dr. Fink provided the data for the study. Dr. Yan conceived and provided statistical analysis of the data. Dr. Yan also reviewed and revised the article. All authors approved the final manuscript as submitted.
Corresponding author
Ethics declarations
Conflicts of interest
Ericka L. Fink discloses that the PANGEA study was funded by a Laerdal Foundation Grant. The remaining authors have no disclosures.
Ethical approval/informed consent
This work is adherent with ethical guidelines. The study details were submitted to Children’s Wisconsin Institutional Review Board and was deemed not Human Subjects Research. Submission of further institutional review board application was not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Snooks, K.C., Yan, K., Farias-Moeller, R. et al. Continuous Electroencephalogram and Antiseizure Medication Use in an International Pediatric Traumatic Brain Injury Population. Neurocrit Care 36, 573–583 (2022). https://doi.org/10.1007/s12028-021-01337-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-021-01337-7