Abstract
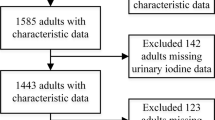
Iodine deficiency results in elevated thyroglobulin (Tg) concentrations, with high iodine Tg being more immunogenic than low iodine Tg. The study investigated the correlation between serum iodine concentration and thyroglobulin autoantibody (TgAb) levels across diverse iodine nutritional statuses as determined by urine iodine concentration (UIC). Demographic information was collected from 1,482 participants through a questionnaire. Blood and spot urine were collected to measure thyroid-stimulating hormone (TSH), TgAb, thyroid anti-peroxidase antibody (TPOAb), serum iodine (SIC), serum non-protein-bound iodine (snPBI), urine iodine (UIC), creatinine (UCr). The median UIC and SIC were 146.5 μg/L and 74.9 μg/L, respectively. A linear relationship was observed between SIC, snPBI, and serum-protein-bound iodine (sPBI) (P < 0.001). The 90% reference intervals for SIC, snPBI, and sPBI were 50.7–120.7 μg/L, 21.9–52.9 μg/L, and 19.7–77.9 μg/L, respectively. The prevalence of elevated TgAb levels was significantly higher in women than in men (P < 0.001). Both low and high levels of snPBI and sPBI were associated with an increased risk of elevated TgAb levels. In women, the risk of positive TgAb in the group below the reference value of snPBI (OR = 2.079, 95%CI: 1.166, 3.705) and sPBI (OR = 2.578, 95%CI: 1.419, 4.684) was higher. In men, the risk of positive TgAb in the group below the reference value of SIC was higher (OR = 3.395, 95%CI: 1.286, 8.962). Iodine might exert an influence on TgAb levels through its binding to proteins, primarily Tg, thereby altering the iodine content of Tg. The interplay of gender factors further enhanced the risk of TgAb emergence.



Similar content being viewed by others
Data Availability
No datasets were generated or analysed during the current study.
Abbreviations
- Tg:
-
Thyroglobulin
- TgAb:
-
Thyroglobulin antibody
- TSH:
-
Thyroid-stimulating hormone
- TPOAb:
-
Thyroid anti-peroxidase antibody
- SIC:
-
Serum iodine concentration
- SnPBI:
-
Serum non-protein-bound iodine
- UIC:
-
Urine iodine concentration
- UCr:
-
Urine creatinine
References
Triggiani V, Tafaro E, Giagulli VA, Sabbà C, Resta F, Licchelli B, Guastamacchia E (2009) Role of iodine, selenium and other micronutrients in thyroid function and disorders. Endocr Metab Immune Disord Drug Targets 9:277–294. https://doi.org/10.2174/187153009789044392
Guastamacchia E, Giagulli V, Licchelli B, Triggiani V (2015) Selenium and Iodine in Autoimmune Thyroiditis. Endocr Metab Immune Disord-Drug Targets 15:288–292. https://doi.org/10.2174/1871530315666150619094242
Zhao J, van der Haar F (2004) Progress in salt iodization and improved iodine nutrition in China, 1995–99. Food Nutr Bull 25:337–343. https://doi.org/10.1177/156482650402500403
Sun D, Codling K, Chang S, Zhang S, Shen H, Su X, Chen Z, Scherpbier RW, Yan J (2017) Eliminating iodine deficiency in China: achievements, challenges and global implications. Nutrients 9:361. https://doi.org/10.3390/nu9040361
Li Y, Teng D, Ba J, Chen B, Du J, He L, Lai X, Teng X, Shi X, Li Y, Chi H, Liao E, Liu C, Liu L, Qin G, Qin Y, Quan H, Shi B, Sun H, Tang X, Tong N, Wang G, Zhang J-A, Wang Y, Xue Y, Yan L, Yang J, Yang L, Yao Y, Ye Z, Zhang Q, Zhang L, Zhu J, Zhu M, Ning G, Mu Y, Zhao J, Shan Z, Teng W (2020) Efficacy and safety of long-term universal salt iodization on thyroid disorders: epidemiological evidence from 31 Provinces of Mainland China. Thyroid Off J Am Thyroid Assoc 30:568–579. https://doi.org/10.1089/thy.2019.0067
Banga JP, Schott M (2018) Autoimmune Thyroid Diseases. Horm Metab Res Horm Stoffwechselforschung Horm Metab 50:837–839. https://doi.org/10.1055/a-0799-5068
Hamada N, Noh JY, Okamoto Y, Ueda M, Konishi T, Fujisawa T, Ito K, Ito K (2010) Measuring thyroglobulin autoantibodies by sensitive assay is important for assessing the presence of thyroid autoimmunity in areas with high iodine intake. Endocr J 57:645–649. https://doi.org/10.1507/endocrj.k09e-353
Dong YH, Fu DG (2014) Autoimmune thyroid disease: mechanism, genetics and current knowledge. Eur Rev Med Pharmacol Sci 18:3611–3618
Ragusa F, Fallahi P, Elia G, Gonnella D, Paparo SR, Giusti C, Churilov LP, Ferrari SM, Antonelli A (2019) Hashimotos’ thyroiditis: epidemiology, pathogenesis, clinic and therapy. Best Pract Res Clin Endocrinol Metab 33:101367. https://doi.org/10.1016/j.beem.2019.101367
Tomer Y, Huber A (2009) The etiology of autoimmune thyroid disease: a story of genes and environment. J Autoimmun 32:231–239. https://doi.org/10.1016/j.jaut.2009.02.007
Mariotti S, Caturegli P, Piccolo P, Barbesino G, Pinchera A (1990) Antithyroid peroxidase autoantibodies in thyroid diseases. J Clin Endocrinol Metab 71:661–669. https://doi.org/10.1210/jcem-71-3-661
Chaker L, Razvi S, Bensenor IM, Azizi F, Pearce EN, Peeters RP (2022) Hypothyroidism. Nat Rev Dis Primer 8:30. https://doi.org/10.1038/s41572-022-00357-7
Toyoda N, Nishikawa M, Iwasaka T (1999) Anti-thyroglobulin antibodies. Nihon Rinsho Jpn J Clin Med 57:1810–1814
** M, Zhang Z, Li Y, Teng D, Shi X, Ba J, Chen B, Du J, He L, Lai X, Teng X, Li Y, Chi H, Liao E, Liu C, Liu L, Qin G, Qin Y, Quan H, Shi B, Sun H, Tang X, Tong N, Wang G, Zhang J, Wang Y, Xue Y, Yan L, Yang J, Yang L, Yao Y, Ye Z, Zhang Q, Zhang L, Zhu J, Zhu M, Ning G, Mu Y, Zhao J, Teng W, Shan Z (2020) U-Shaped associations between urinary iodine concentration and the prevalence of metabolic disorders: a cross-sectional study. Thyroid 30:1053–1065. https://doi.org/10.1089/thy.2019.0516
WHO/ICCIDD (2007) Assessment of iodine deficiency disorders and monitoring their elimination: a guide for program managers, 3rd edn. WHO, Geneva
Brix TH, Kyvik KO, Christensen K, Hegedüs L (2001) Evidence for a major role of heredity in Graves’ disease: a population-based study of two Danish twin cohorts. J Clin Endocrinol Metab 86:930–934. https://doi.org/10.1210/jcem.86.2.7242
Wang F, Li C, Li S, Cui L, Zhao J, Liao L (2023) Selenium and thyroid diseases. Front Endocrinol 14:1133000. https://doi.org/10.3389/fendo.2023.1133000
Antonelli A, Ferrari SM, Ragusa F, Elia G, Paparo SR, Ruffilli I, Patrizio A, Giusti C, Gonnella D, Cristaudo A, Foddis R, Shoenfeld Y, Fallahi P (2020) Graves’ disease: epidemiology, genetic and environmental risk factors and viruses. Best Pract Res Clin Endocrinol Metab 34:101387. https://doi.org/10.1016/j.beem.2020.101387
Wang W, Mao J, Zhao J, Lu J, Yan L, Du J, Lu Z, Wang H, Xu M, Bai X, Zhu L, Fan C, Wang H, Zhang H, Shan Z, Teng W (2018) Decreased thyroid peroxidase antibody titer in response to selenium supplementation in autoimmune thyroiditis and the influence of a selenoprotein P Gene Polymorphism: a prospective, multicenter study in China. Thyroid Off J Am Thyroid Assoc 28:1674–1681. https://doi.org/10.1089/thy.2017.0230
Zhu L, Bai X, Teng W, Shan Z, Wang W, Fan C, Wang H, Zhang H (2012) Effects of selenium supplementation on antibodies of autoimmune thyroiditis. Zhonghua Yi Xue Za Zhi 92:2256–2260
Qiu Y, **ng Z, **ang Q, Yang Q, Zhu J, Su A (2021) Insufficient evidence to support the clinical efficacy of selenium supplementation for patients with chronic autoimmune thyroiditis. Endocrine 73:384–397. https://doi.org/10.1007/s12020-021-02642-z
Winther KH, Wichman JEM, Bonnema SJ, Hegedüs L (2017) Insufficient documentation for clinical efficacy of selenium supplementation in chronic autoimmune thyroiditis, based on a systematic review and meta-analysis. Endocrine 55:376–385. https://doi.org/10.1007/s12020-016-1098-z
Rayman MP (2019) Multiple nutritional factors and thyroid disease, with particular reference to autoimmune thyroid disease. Proc Nutr Soc 78:34–44. https://doi.org/10.1017/S0029665118001192
Hess SY, Zimmermann MB, Arnold M, Langhans W, Hurrell RF (2002) Iron deficiency anemia reduces thyroid peroxidase activity in rats. J Nutr 132:1951–1955. https://doi.org/10.1093/jn/132.7.1951
Lu Y, Li J, Li J (2016) Estrogen and thyroid diseases: an update. Minerva Med 107:239–244
Mintziori G, Goulis DG, Toulis KA, Venetis CA, Kolibianakis EM, Tarlatzis BC (2011) Thyroid function during ovarian stimulation: a systematic review. Fertil Steril 96:780–785. https://doi.org/10.1016/j.fertnstert.2011.06.020
Mallawa Kankanamalage O, Zhou Q, Li X (2021) Understanding the pathogenesis of gestational hypothyroidism. Front Endocrinol 12:653407. https://doi.org/10.3389/fendo.2021.653407
Carayanniotis G (2007) Recognition of thyroglobulin by T cells: the role of iodine. Thyroid Off J Am Thyroid Assoc 17:963–973. https://doi.org/10.1089/thy.2007.0199
Medeiros-Neto G, Targovnik HM, Vassart G (1993) Defective thyroglobulin synthesis and secretion causing goiter and hypothyroidism. Endocr Rev 14:165–183. https://doi.org/10.1210/edrv-14-2-165
Mammen JSR, Cappola AR (2021) Autoimmune Thyroid Disease in Women. JAMA 325:2392–2393. https://doi.org/10.1001/jama.2020.22196
Feldt-Rasmussen U (1983) Serum Thyroglobulin and Thyroglobulin Autoantibodies in Thyroid Diseases. Allergy 38:369–387. https://doi.org/10.1111/j.1398-9995.1983.tb05081.x
Zimmermann MB, Jooste PL, Pandav CS (2008) Iodine-deficiency disorders. The Lancet 372:1251–1262. https://doi.org/10.1016/S0140-6736(08)61005-3
Rasmussen LB, Ovesen L, Christiansen E (1999) Day-to-day and within-day variation in urinary iodine excretion. Eur J Clin Nutr 53:401–407. https://doi.org/10.1038/sj.ejcn.1600762
Xu T, Guo W, Ren Z, Wei H, Tan L, Zhang W (2022) Study on the relationship between serum iodine and thyroid dysfunctions: a cross-sectional study. Biol Trace Elem Res. https://doi.org/10.1007/s12011-022-03459-1
Nicola JP, Basquin C, Portulano C, Reyna-Neyra A, Paroder M, Carrasco N (2009) The Na+/I- symporter mediates active iodide uptake in the intestine. Am J Physiol Cell Physiol 296:C654-662. https://doi.org/10.1152/ajpcell.00509.2008
** X, Jiang P, Liu L, Jia Q, Liu P, Meng F, Zhang X, Guan Y, Pang Y, Lu Z, Shen H (2017) The application of serum iodine in assessing individual iodine status. Clin Endocrinol (Oxf) 87:807–814. https://doi.org/10.1111/cen.13421
Peng J, Zheng L, **ng J, Lixiang L, Yi P, Yunfeng G, Hongmei S (2016) A preliminary study on medical reference range of serum iodine in adults of normal thyroid function. Chin J Endem 35:786–789. https://doi.org/10.3760/cma.j.issn.2095-4255.2016.11.002
Meng L-H, Chen C-H, Liu Y, Liang X-H, Zhou J, **an J, Li L, Zhang J, Huang Z-X, Qin Y-F (2022) Epidemiological survey of the status of iodine nutrition and thyroid diseases in Guangxi, China. J Trace Elem Med Biol Organ Soc Miner Trace Elem GMS 70:126918. https://doi.org/10.1016/j.jtemb.2021.126918
Andersen S, Iversen F, Terpling S, Pedersen KM, Gustenhoff P, Laurberg P (2009) More hypothyroidism and less hyperthyroidism with sufficient iodine nutrition compared to mild iodine deficiency–a comparative population-based study of older people. Maturitas 64:126–131. https://doi.org/10.1016/j.maturitas.2009.08.007
McGrogan A, Seaman HE, Wright JW, de Vries CS (2008) The incidence of autoimmune thyroid disease: a systematic review of the literature. Clin Endocrinol (Oxf) 69:687–696. https://doi.org/10.1111/j.1365-2265.2008.03338.x
Zhang X, Yuan N, Sun J, Zhao X, Du J, Nan M, Zhang Q, Ji L (2022) Association between iodine nutritional status and adverse pregnancy outcomes in Bei**g, China: a single-center cohort study. Biol Trace Elem Res 200:2620–2628. https://doi.org/10.1007/s12011-021-02887-9
Hurrell RF (1997) Bioavailability of iodine. Eur J Clin Nutr 51(Suppl 1):S9-12
Citterio CE, Targovnik HM, Arvan P (2019) The role of thyroglobulin in thyroid hormonogenesis. Nat Rev Endocrinol 15:323–338. https://doi.org/10.1038/s41574-019-0184-8
Dunn AD, Corsi CM, Myers HE, Dunn JT (1998) Tyrosine 130 is an important outer ring donor for thyroxine formation in thyroglobulin. J Biol Chem 273:25223–25229. https://doi.org/10.1074/jbc.273.39.25223
Acknowledgements
We would like to express our gratitude to the School of Public Health, Tian** Medical University, Tian** Key Laboratory of Environment, Nutrition, and Public Health, and the Center for International Collaborative Research on Environment, Nutrition, and Public Health for creating a conducive environment for sample testing and facilitating the writing of this paper. Their support has been invaluable in the successful execution of our research.
Funding
This work was supported by grants from the National Science Foundation of China (grant numbers 82073549 and 81703218).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Qiuyi Song, Tingting Xu, Yu Wang, and Hongyan Wei. Feng Tan assists with sample collection and clinical diagnosis. The first draft of the manuscript was written by Qiuyi Song and Tingting Xu, and all authors commented on the previous manuscript. All authors read and approved the final manuscript.
Song Qiuyi and Tingting Xu make an equal contribution to the article.
Corresponding author
Ethics declarations
Ethics Approval
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving research study participants were approved by the Medical Ethics Committee of Tian** Medical University (serial number: IRB[2013]115). Informed consent was obtained from all individual participants included in the study.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Consent to Publish
Participants have consented to the submission of this cross-sectional study to the journal.
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Song, Q., Xu, T., Wang, Y. et al. Exploring the Correlation Between Varied Serum Iodine Nutritional Levels and Anti-Thyroglobulin Antibodies. Biol Trace Elem Res (2024). https://doi.org/10.1007/s12011-024-04275-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12011-024-04275-5