Abstract
Purpose of review
We investigate the complexities and interplay between the concepts of prognostic uncertainty and patient preferences as they relate to the delivery of goal-concordant care to patients with severe acute brain injuries (SABI) in the Neurological Intensive Care Unit (Neuro-ICU).
Recent findings
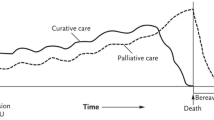
Patients with SABI in the Neuro-ICU have unique palliative care needs due to sudden, often unexpected changes in personhood and quality of life. A substantial amount of uncertainty is inherent and poses a challenge to both the patient’s prognosis and treatment preferences. The delivery of goal-concordant care can be difficult to achieve.
Summary
The uncertainty inherent to both prognosis and patient preferences challenges the provision of goal-concordant care to patients with SABI. The best case/worst case/most likely case scenario is a communication strategy that can aid clinicians when discussing the patient’s uncertain prognosis. A time-limited trial may provide a framework for families and clinicians to pursue aggressive life-sustaining treatment for a certain amount of time, in which prognosis may become more defined, patient goals may become clearer, and clinicians and families may establish a common ground. Although the delivery of goal-concordant care in the Neuro-ICU may be an unachievable, lofty goal, it is a level of care that we should continue to strive for and discuss.
Similar content being viewed by others
Availability of data and materials
Not applicable.
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance
Creutzfeldt CJ, Engelberg RA, Healey L, et al. Palliative care needs in the Neuro-ICU. Crit Care Med. 2015;43(8):1677–84. https://doi.org/10.1097/CCM.0000000000001018.
Curtis JR, White DB. Practical guidance for evidence-based ICU family conferences. Chest. 2008;134(4):835–43. https://doi.org/10.1378/chest.08-0235.
Curtis JR, Vincent JL. Ethics and end-of-life care for adults in the intensive care unit. Lancet. 2010;376(9749):1347–53. https://doi.org/10.1016/S0140-6736(10)60143-2.
Halpern SD. Goal-concordant care - searching for the holy grail. N Engl J Med. 2019;381(17):1603–6. https://doi.org/10.1056/NEJMp1908153.
Creutzfeldt CJ, Holloway RG. Treatment decisions for a future self: ethical obligations to guide truly informed choices. JAMA. 2020;323(2):115–6. https://doi.org/10.1001/jama.2019.19652.
Jones K, Quinn T, Mazor KM, Muehlschlegel S. Prognostic uncertainty in critically ill patients with traumatic brain injury: a multicenter qualitative study. Neurocrit Care. 2021;35(2):311–21. https://doi.org/10.1007/s12028-021-01230-3.
Greenberg SM, Ziai WC, Cordonnier C, et al. 2022 Guideline for the management of patients with spontaneous intracerebral hemorrhage: a guideline from the American Heart Association/American Stroke Association. Stroke. 2022;53(7):e282–361. https://doi.org/10.1161/STR.0000000000000407.
Busl KM, Fried H, Muehlschlegel S, et al. Guidelines for neuroprognostication in adults with guillain-barré syndrome [published correction appears in Neurocrit Care. Neurocrit Care. 2023;38(3):564–583. https://doi.org/10.1007/s12028-023-01707-3.
Rajajee V, Muehlschlegel S, Wartenberg KE, et al. Guidelines for neuroprognostication in comatose adult survivors of cardiac arrest. Neurocrit Care. 2023;38(3):533–63. https://doi.org/10.1007/s12028-023-01688-3.
Becker KJ, Baxter AB, Cohen WA, et al. Withdrawal of support in intracerebral hemorrhage may lead to self-fulfilling prophecies. Neurology. 2001;56(6):766–72. https://doi.org/10.1212/wnl.56.6.766.
Creutzfeldt CJ, Becker KJ, Weinstein JR, et al. Do-not-attempt-resuscitation orders and prognostic models for intraparenchymal hemorrhage. Crit Care Med. 2011;39(1):158–62. https://doi.org/10.1097/CCM.0b013e3181fb7b49.
Huijben JA, Volovici V, Cnossen MC, et al. Variation in general supportive and preventive intensive care management of traumatic brain injury: a survey in 66 neurotrauma centers participating in the Collaborative European NeuroTrauma Effectiveness Research in Traumatic Brain Injury (CENTER-TBI) study. Crit Care. 2018;22(1):90. Published 2018 Apr 13. https://doi.org/10.1186/s13054-018-2000-6.
George BP, Kelly AG, Schneider EB, Holloway RG. Current practices in feeding tube placement for US acute ischemic stroke inpatients. Neurology. 2014;83(10):874–82. https://doi.org/10.1212/WNL.0000000000000764.
Krishnamoorthy V, Hough CL, Vavilala MS, et al. Tracheostomy after severe acute brain injury: trends and variability in the USA. Neurocrit Care. 2019;30(3):546–54. https://doi.org/10.1007/s12028-019-00697-5.
Kelly AG, Zahuranec DB, Holloway RG, Morgenstern LB, Burke JF. Variation in do-not-resuscitate orders for patients with ischemic stroke: implications for national hospital comparisons. Stroke. 2014;45(3):822–7. https://doi.org/10.1161/STROKEAHA.113.004573.
Quill TE, Holloway R. Time-limited trials near the end of life. JAMA. 2011;306(13):1483–4. https://doi.org/10.1001/jama.2011.1413.
VanKerkhoff TD, Viglianti EM, Detsky ME, Kruser JM. Time-limited trials in the intensive care unit to promote goal-concordant patient care. Clin Pulm Med. 2019;26(5):141–5. https://doi.org/10.1097/cpm.0000000000000323.
Leiter RE, Tulsky JA. Time-limited trials and potentially nonbeneficial treatment in the ICU-willing to wait for it. JAMA Intern Med. 2021;181(6):795–6. https://doi.org/10.1001/jamainternmed.2021.0988.
• Chang DW, Neville TH, Parrish J, et al. Evaluation of time-limited trials among critically ill patients with advanced medical illnesses and reduction of nonbeneficial ICU treatments. JAMA Intern Med. 2021;181(6):786–794. https://doi.org/10.1001/jamainternmed.2021.1000. A prospective quality improvement study aiming to evaluate if time-limited trials for patients in the medical intensive care unit was associated with decreased length of stay in the ICU and usage of certain therapies. The use of time-limited trials was associated with less frequent invasive procedures, shorter length of stay in the ICU, and more family meetings that included discourse regarding risk and benefits of treatment options, eliciting of patient values, and establishing signs of clinical improvement.
Bruce CR, Liang C, Blumenthal-Barby JS, et al. Barriers and facilitators to initiating and completing time-limited trials in critical care. Crit Care Med. 2015;43(12):2535–43. https://doi.org/10.1097/CCM.0000000000001307.
Viglianti EM, Ervin JN, Newton CA, Kruser JM, Iwashyna TJ, Valley TS. Time-limited trials in the ICU: a mixed-methods sequential explanatory study of intensivists at two academic centres. BMJ Open. 2022;12(4):e059325. Published 2022 Apr 4. https://doi.org/10.1136/bmjopen-2021-059325.
• Kiker WA, Voumard RR, Plinke W, Longstreth WT Jr, Curtis JR, Creutzfeldt CJ. Prognosis predictions by families, physicians, and nurses of patients with severe acute brain injury: agreement and accuracy. Neurocrit Care. 2022;37(1):38–46. https://doi.org/10.1007/s12028-022-01501-7. The goal of the study was to analyze the prognostic predictions regarding recovery of patients with severe acute brain injury made by families, clinicians, and nurses. Families had significantly more optimistic predictions of recovery compared to both clinicians and nurses.
• Kiker WA, Rutz Voumard R, Andrews LIB, et al. Assessment of discordance between physicians and family members regarding prognosis in patients with severe acute brain injury. JAMA Netw Open. 2021;4(10):e2128991. Published 2021 Oct 1. https://doi.org/10.1001/jamanetworkopen.2021.28991. The goal of the study was to investigate prognosis discordance between clinicians and families of patients with severe acute brain injury. Discordance occurred with 61% of patients and was more common in non-white families compared to white families.
Quinn T, Moskowitz J, Khan MW, et al. What families need and physicians deliver: contrasting communication preferences between surrogate decision-makers and physicians during outcome prognostication in critically ill TBI patients. Neurocrit Care. 2017;27(2):154–62. https://doi.org/10.1007/s12028-017-0427-2.
Goss A, Ge C, Crawford S, et al. Prognostic language in critical neurologic illness: a multicenter mixed-methods study. Neurology. 2023;101(5):e558–69. https://doi.org/10.1212/WNL.0000000000207462.
White DB, Ernecoff N, Buddadhumaruk P, et al. Prevalence of and factors related to discordance about prognosis between physicians and surrogate decision makers of critically ill patients. JAMA. 2016;315(19):2086–94. https://doi.org/10.1001/jama.2016.5351.
Boyd EA, Lo B, Evans LR, et al. “It’s not just what the doctor tells me:” factors that influence surrogate decision-makers’ perceptions of prognosis. Crit Care Med. 2010;38(5):1270–5. https://doi.org/10.1097/CCM.0b013e3181d8a217.
Schwarze ML, Kehler JM, Campbell TC. Navigating high risk procedures with more than just a street map. J Palliat Med. 2013;16(10):1169–71. https://doi.org/10.1089/jpm.2013.0221.
Taylor LJ, Nabozny MJ, Steffens NM, et al. A framework to improve surgeon communication in high-stakes surgical decisions: best case/worst case. JAMA Surg. 2017;152(6):531–8. https://doi.org/10.1001/jamasurg.2016.5674.
Schwarze ML, Zelenski A, Baggett ND, et al. Best case/worst case: ICU (COVID-19)-a tool to communicate with families of critically ill patients with COVID-19. Palliat Med Rep. 2020;1(1):3–4. Published 2020 Apr 30. https://doi.org/10.1089/pmr.2020.0038.
• Zimmermann CJ, Zelenski AB, Buffington A, et al. Best case/worst case for the trauma ICU: development and pilot testing of a communication tool for older adults with traumatic injury. J Trauma Acute Care Surg. 2021;91(3):542–51. https://doi.org/10.1097/TA.0000000000003281. The ‘best case/worst case’ communication tool was evaluated in a pre-post study for use with older adults in the trauma intensive care unit. Use of this tool was associated with significant improvement in end-of-life communication score and resulted in less clinicians endorsed providing false hope.
Blumenthaler AN, Robinson KA, Hodge C, et al. Communication frameworks for palliative surgical consultations: a randomized study of advanced cancer patients [published online ahead of print, 2023 Feb 21]. Ann Surg. 2023. https://doi.org/10.1097/SLA.0000000000005823.
Kruser JM, Nabozny MJ, Steffens NM, et al. “Best case/worst case”: qualitative evaluation of a novel communication tool for difficult in-the-moment surgical decisions. J Am Geriatr Soc. 2015;63(9):1805–11. https://doi.org/10.1111/jgs.13615.
Scheunemann LP, Cunningham TV, Arnold RM, Buddadhumaruk P, White DB. How clinicians discuss critically ill patients’ preferences and values with surrogates: an empirical analysis. Crit Care Med. 2015;43(4):757–64. https://doi.org/10.1097/CCM.0000000000000772.
Scheunemann LP, Ernecoff NC, Buddadhumaruk P, et al. Clinician-family communication about patients’ values and preferences in intensive care units. JAMA Intern Med. 2019;179(5):676–84. https://doi.org/10.1001/jamainternmed.2019.0027.
Alonso A, Dörr D, Szabo K. Critical appraisal of advance directives given by patients with fatal acute stroke: an observational cohort study. BMC Med Ethics. 2017;18(1):7. Published 2017 Feb 2. https://doi.org/10.1186/s12910-016-0166-5.
• Rutz Voumard R, Dugger KM, Kiker WA, et al. Goal-concordant care after severe acute brain injury. Front Neurol. 2021;12:710783. Published 2021 Sep 17. https://doi.org/10.3389/fneur.2021.710783. This study compared the goals-of-care of patients with severe acute brain injury with the treatment that they received in the intensive care unit. 88% of patients who had the goal of extending life were receiving care that was in line with this goal, while only 27% of patients who prioritized receiving care that optimized comfort and quality of life received such care.
Taylor LJ, Johnson SK, Nabozny MJ, et al. Barriers to goal-concordant care for older patients with acute surgical illness: communication patterns extrinsic to decision aids. Ann Surg. 2018;267(4):677–82. https://doi.org/10.1097/SLA.0000000000002282.
Ahmad SR, Tarabochia AD, Budahn L, et al. Determining goal concordant care in the intensive care unit using electronic health records. J Pain Symptom Manage. 2023;65(3):e199–205. https://doi.org/10.1016/j.jpainsymman.2022.11.002.
Hwang DY, Knies AK, Mampre D, et al. Concerns of surrogate decision makers for patients with acute brain injury: a US population survey. Neurology. 2020;94(19):e2054–68. https://doi.org/10.1212/WNL.0000000000009406.
Garg A, Soto AL, Knies AK, et al. Predictors of surrogate decision makers selecting life-sustaining therapy for severe acute brain injury patients: an analysis of US population survey data. Neurocrit Care. 2021;35(2):468–79. https://doi.org/10.1007/s12028-021-01200-9.
Young MJ, Regenhardt RW, Sokol LL, Leslie-Mazwi TM. When should neuroendovascular care for patients with acute stroke be palliative? AMA J Ethics. 2021;23(10):E783–E793. Published 2021 Oct 1. https://doi.org/10.1001/amajethics.2021.783.
McHugh DC, George BP, Bender MT, et al. Reversal of advanced directives in neurologic emergencies. Neurohospitalist. 2022;12(4):651–8. https://doi.org/10.1177/19418744221097348.
Plinke WV, Buchbinder SA, Brumback LC, et al. Identification of palliative care needs and mental health outcomes among family members of patients with severe acute brain injury. JAMA Netw Open. 2023;6(4):e239949. Published 2023 Apr 3. https://doi.org/10.1001/jamanetworkopen.2023.9949.
Wendlandt B, Olm-Shipman C, Ceppe A, et al. Surrogates of patients with severe acute brain injury experience persistent anxiety and depression over the 6 months after ICU admission. J Pain Symptom Manage. 2022;63(6):e633–9. https://doi.org/10.1016/j.jpainsymman.2022.02.336.
RutzVoumard R, Kiker WA, Dugger KM, et al. Adapting to a new normal after severe acute brain injury: an observational cohort using a sequential explanatory design. Crit Care Med. 2021;49(8):1322–32. https://doi.org/10.1097/CCM.0000000000004947.
White DB, Angus DC, Shields AM, et al. A randomized trial of a family-support intervention in intensive care units. N Engl J Med. 2018;378(25):2365–75. https://doi.org/10.1056/NEJMoa1802637.
Torke AM, Varner-Perez SE, Burke ES, et al. Effects of spiritual care on well-being of intensive care family surrogates: a clinical trial. J Pain Symptom Manage. 2023;65(4):296–307. https://doi.org/10.1016/j.jpainsymman.2022.12.007.
Curtis JR, Treece PD, Nielsen EL, et al. Randomized trial of communication facilitators to reduce family distress and intensity of end-of-life care. Am J Respir Crit Care Med. 2016;193(2):154–62. https://doi.org/10.1164/rccm.201505-0900OC.
Goss AL, Voumard RR, Engelberg RA, Curtis JR, Creutzfeldt CJ. Do they have a choice? Surrogate decision-making after severe acute brain injury. Crit Care Med. 2023;51(7):924–35. https://doi.org/10.1097/CCM.0000000000005850.
Lou W, Granstein JH, Wabl R, Singh A, Wahlster S, Creutzfeldt CJ. Taking a chance to recover: families look back on the decision to pursue tracheostomy after severe acute brain injury. Neurocrit Care. 2022;36(2):504–10. https://doi.org/10.1007/s12028-021-01335-9.
Connors AF, Dawson NV, Desbiens NA, et al. A controlled trial to improve care for seriously ill hospitalized patients: the study to understand prognoses and preferences for outcomes and risks of treatments (support). JAMA. 1995;274:1591–8. https://doi.org/10.1001/jama.1995.03530200027032.
Comer AR, Hickman SE, Slaven JE, et al. Assessment of discordance between surrogate care goals and medical treatment provided to older adults with serious illness. JAMA Netw Open. 2020;3(5):e205179. Published 2020 May 1. https://doi.org/10.1001/jamanetworkopen.2020.5179.
Funding
National Institutes of Health, R01 NR019268.
Author information
Authors and Affiliations
Contributions
KAH and CJC were responsible for the preparation and conceptualization of the first draft of the manuscript. All authors contributed equally to the revision of subsequent drafts and approval of the final manuscript.
Corresponding author
Ethics declarations
Ethical Approval
Not applicable.
Conflict of Interest
Kristopher A. Hendershot declares that he has no conflict of interest. Maya N. Elias declares that she has no conflict of interest. Breana L. Taylor declares that she has no conflict of interest. Sarah Wahlster declares that she has no conflict of interest. Claire J. Creutzfeldt declares that she has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subject performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hendershot, K.A., Elias, M.N., Taylor, B.L. et al. An Update on Palliative Care in Neurocritical Care: Providing Goal-Concordant Care in the Face of Prognostic Uncertainty. Curr Treat Options Neurol 25, 517–529 (2023). https://doi.org/10.1007/s11940-023-00778-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11940-023-00778-z