Abstract
Purpose of review
To describe the biological rationale of peripheral blood cells (PBC)–derived inflammatory indexes and assess the related prognostic scores for patients with advanced non-small cell lung cancer (aNSCLC) treated with immune-checkpoint inhibitors (ICI).
Recent findings
Inflammatory indexes based on PBC may indicate a pro-inflammatory condition affecting the immune response to cancer. The lung immune prognostic index (LIPI), consisting of derived neutrophils-to-lymphocyte ratio (NLR) and lactate dehydrogenase, is a validated prognostic tool, especially for pretreated aNSCLC patients, where the combination of NLR and PD-L1 tumour expression might also be predictive of immunotherapy benefit. In untreated high-PD-L1 aNSCLC patients, the Lung-Immune-Prognostic score (LIPS), including NLR, ECOG PS and concomitant steroids, is prognostic, and its modified version might indicate patients with favourable outcomes despite an ECOG PS of 2. NLR times platelets (i.e., SII), included in the NHS-Lung score, might improve the prognostication for combined chemoimmunotherapy.
Summary
PBC-derived inflammatory indexes and related scores represent accurate, reproducible and non-expensive prognostic tools with clinical and research utility.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454(7203):436–44. https://doi.org/10.1038/nature07205.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–74. https://doi.org/10.1016/j.cell.2011.02.013.
Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010;140(6):883–99. https://doi.org/10.1016/j.cell.2010.01.025.
Negrini S, Gorgoulis VG, Halazonetis TD. Genomic instability—an evolving hallmark of cancer. Nat Rev Mol Cell Biol. 2010;11(3):220–8. https://doi.org/10.1038/nrm2858.
Colotta F, Allavena P, Sica A, Garlanda C, Mantovani A. Cancer-related inflammation, the seventh hallmark of cancer: links to genetic instability. Carcinogenesis. 2009;30(7):1073–81. https://doi.org/10.1093/carcin/bgp127.
Qian BZ, Pollard JW. Macrophage diversity enhances tumor progression and metastasis. Cell. 2010;141(1):39–51. https://doi.org/10.1016/j.cell.2010.03.014.
Mougiakakos D, Choudhury A, Lladser A, Kiessling R, Johansson CC. Chapter 3 - Regulatory T cells in cancer. In: Vande Woude GF, Klein G, editors. Advances in Cancer Research. Academic Press; 2010. p. 57–117.
Hiam-Galvez KJ, Allen BM, Spitzer MH. Systemic immunity in cancer. Nat Rev Cancer. 2021;21(6):345–59. https://doi.org/10.1038/s41568-021-00347-z.
Guner A, Kim HI. Biomarkers for evaluating the inflammation status in patients with cancer. J Gastric Cancer. 2019;19(3):254–77. https://doi.org/10.5230/jgc.2019.19.e29.
Mezquita L, Auclin E, Ferrara R, Charrier M, Remon J, Planchard D, et al. Association of the lung immune prognostic index with immune checkpoint inhibitor outcomes in patients with advanced non-small cell lung cancer. JAMA Oncol. 2018;4(3):351–7. https://doi.org/10.1001/jamaoncol.2017.4771.
Kazandjian D, Gong Y, Keegan P, Pazdur R, Blumenthal GM. Prognostic value of the lung immune prognostic index for patients treated for metastatic non-small cell lung cancer. JAMA Oncol. 2019;5(10):1481–5. https://doi.org/10.1001/jamaoncol.2019.1747. This study validated the lung immune prognostic index in patients with pretreated aNSCLC by a pooled analysis of randomised controlled trials with immunotherapy.
Wang Y, Li Y, Chen P, Xu W, Wu Y, Che G. Prognostic value of the pretreatment systemic immune-inflammation index (SII) in patients with non-small cell lung cancer: a meta-analysis. Ann Transl Med. 2019;7(18):433. https://doi.org/10.21037/atm.2019.08.116.
Lim JU, Yeo CD, Kang HS, Park CK, Kim JS, Kim JW, et al. Elevated pretreatment platelet-to-lymphocyte ratio is associated with poor survival in stage IV non-small cell lung cancer with malignant pleural effusion. Sci Rep. 2019;9(1):4721. https://doi.org/10.1038/s41598-019-41289-9.
Medzhitov R. Inflammation 2010: new adventures of an old flame. Cell. 2010;140(6):771–6. https://doi.org/10.1016/j.cell.2010.03.006.
Akira S, Uematsu S, Takeuchi O. Pathogen recognition and innate immunity. Cell. 2006;124(4):783–801. https://doi.org/10.1016/j.cell.2006.02.015.
Yano S, Nokihara H, Yamamoto A, Goto H, Ogawa H, Kanematsu T, et al. Multifunctional interleukin-1beta promotes metastasis of human lung cancer cells in SCID mice via enhanced expression of adhesion-, invasion- and angiogenesis-related molecules. Cancer Sci. 2003;94(3):244–52. https://doi.org/10.1111/j.1349-7006.2003.tb01428.x.
Greten FR, Grivennikov SI. Inflammation and cancer: triggers, mechanisms, and consequences. Immunity. 2019;51(1):27–41. https://doi.org/10.1016/j.immuni.2019.06.025.
Joyce JA, Fearon DT. T cell exclusion, immune privilege, and the tumor microenvironment. Science. 2015;348(6230):74–80. https://doi.org/10.1126/science.aaa6204.
** MZ, ** WL. The updated landscape of tumor microenvironment and drug repurposing. Signal Transduct Target Ther. 2020;5(1):166. https://doi.org/10.1038/s41392-020-00280-x.
Bunt SK, Sinha P, Clements VK, Leips J, Ostrand-Rosenberg S. Inflammation induces myeloid-derived suppressor cells that facilitate tumor progression. J Immunol. 2006;176(1):284–90. https://doi.org/10.4049/jimmunol.176.1.284.
Chen L, Huang CF, Li YC, Deng WW, Mao L, Wu L, et al. Blockage of the NLRP3 inflammasome by MCC950 improves anti-tumor immune responses in head and neck squamous cell carcinoma. Cell Mol Life Sci. 2018;75(11):2045–58. https://doi.org/10.1007/s00018-017-2720-9.
Chaudhry SI, Hooper S, Nye E, Williamson P, Harrington K, Sahai E. Autocrine IL-1beta-TRAF6 signalling promotes squamous cell carcinoma invasion through paracrine TNFalpha signalling to carcinoma-associated fibroblasts. Oncogene. 2013;32(6):747–58. https://doi.org/10.1038/onc.2012.91.
Taniguchi K, Karin M. NF-kappaB, inflammation, immunity and cancer: coming of age. Nat Rev Immunol. 2018;18(5):309–24. https://doi.org/10.1038/nri.2017.142.
Elaraj DM, Weinreich DM, Varghese S, Puhlmann M, Hewitt SM, Carroll NM, et al. The role of interleukin 1 in growth and metastasis of human cancer xenografts. Clin Cancer Res. 2006;12(4):1088–96. https://doi.org/10.1158/1078-0432.CCR-05-1603.
Kim JW, Koh Y, Kim DW, Ahn YO, Kim TM, Han SW, et al. Clinical Implications of VEGF, TGF-beta1, and IL-1beta in Patients with advanced non-small cell lung cancer. Cancer Res Treat. 2013;45(4):325–33. https://doi.org/10.4143/crt.2013.45.4.325.
Millares L, Barreiro E, Cortes R, Martinez-Romero A, Balcells C, Cascante M, et al. Tumor-associated metabolic and inflammatory responses in early stage non-small cell lung cancer: local patterns and prognostic significance. Lung Cancer. 2018;122:124–30. https://doi.org/10.1016/j.lungcan.2018.06.015.
de Visser KE, Coussens LM. The inflammatory tumor microenvironment and its impact on cancer development. Contrib Microbiol. 2006;13:118–37. https://doi.org/10.1159/000092969.
Allavena P, Sica A, Solinas G, Porta C, Mantovani A. The inflammatory micro-environment in tumor progression: the role of tumor-associated macrophages. Crit Rev Oncol Hematol. 2008;66(1):1–9. https://doi.org/10.1016/j.critrevonc.2007.07.004.
Balkwill FR, Capasso M, Hagemann T. The tumor microenvironment at a glance. J Cell Sci. 2012;125(Pt 23):5591–6. https://doi.org/10.1242/jcs.116392.
Jang JH, Kim DH, Surh YJ. Dynamic roles of inflammasomes in inflammatory tumor microenvironment. NPJ Precis Oncol. 2021;5(1):18. https://doi.org/10.1038/s41698-021-00154-7.
Leach M. Interpretation of the full blood count in systemic disease—a guide for the physician. J R Coll Phys Edinb. 2014;44(1):36–41. https://doi.org/10.4997/JRCPE.2014.109.
Velioglu Y, Yuksel A. Complete blood count parameters in peripheral arterial disease. Aging Male. 2019;22(3):187–91. https://doi.org/10.1080/13685538.2019.1588873.
Zinellu A, Paliogiannis P, Sotgiu E, Mellino S, Mangoni AA, Zinellu E, et al. Blood Cell count derived inflammation indexes in patients with idiopathic pulmonary fibrosis. Lung. 2020;198(5):821–7. https://doi.org/10.1007/s00408-020-00386-7.
Guthrie GJ, Charles KA, Roxburgh CS, Horgan PG, McMillan DC, Clarke SJ. The systemic inflammation-based neutrophil-lymphocyte ratio: experience in patients with cancer. Crit Rev Oncol Hematol. 2013;88(1):218–30. https://doi.org/10.1016/j.critrevonc.2013.03.010.
Sacdalan DB, Lucero JA, Sacdalan DL. Prognostic utility of baseline neutrophil-to-lymphocyte ratio in patients receiving immune checkpoint inhibitors: a review and meta-analysis. Onco Targets Ther. 2018;11:955–65. https://doi.org/10.2147/OTT.S153290.
Diakos CI, Charles KA, McMillan DC, Clarke SJ. Cancer-related inflammation and treatment effectiveness. Lancet Oncol. 2014;15(11):e493-503. https://doi.org/10.1016/S1470-2045(14)70263-3.
Moses K, Brandau S. Human neutrophils: their role in cancer and relation to myeloid-derived suppressor cells. Semin Immunol. 2016;28(2):187–96. https://doi.org/10.1016/j.smim.2016.03.018.
Coffelt SB, Wellenstein MD, de Visser KE. Neutrophils in cancer: neutral no more. Nat Rev Cancer. 2016;16(7):431–46. https://doi.org/10.1038/nrc.2016.52.
Park S, Zhu J, Altan-Bonnet G, Cheng SY. Monocyte recruitment and activated inflammation are associated with thyroid carcinogenesis in a mouse model. Am J Cancer Res. 2019;9(7):1439–53.
Ostroumov D, Fekete-Drimusz N, Saborowski M, Kuhnel F, Woller N. CD4 and CD8 T lymphocyte interplay in controlling tumor growth. Cell Mol Life Sci. 2018;75(4):689–713. https://doi.org/10.1007/s00018-017-2686-7.
Schmied L, Hoglund P, Meinke S. Platelet-Mediated protection of cancer cells from immune surveillance—possible implications for cancer immunotherapy. Front Immunol. 2021;12: 640578. https://doi.org/10.3389/fimmu.2021.640578.
Goubran HA, Stakiw J, Radosevic M, Burnouf T. Platelets effects on tumor growth. Semin Oncol. 2014;41(3):359–69. https://doi.org/10.1053/j.seminoncol.2014.04.006.
Prager GW, Poettler M, Unseld M, Zielinski CC. Angiogenesis in cancer: Anti-VEGF escape mechanisms. Transl Lung Cancer Res. 2012;1(1):14–25. https://doi.org/10.3978/j.issn.2218-6751.2011.11.02.
Stoiber D, Assinger A. Platelet-leukocyte interplay in cancer development and progression. Cells. 2020;9(4). https://doi.org/10.3390/cells9040855.
Lefrancais E, Ortiz-Munoz G, Caudrillier A, Mallavia B, Liu F, Sayah DM, et al. The lung is a site of platelet biogenesis and a reservoir for haematopoietic progenitors. Nature. 2017;544(7648):105–9. https://doi.org/10.1038/nature21706.
Rodriguez-Martinez A, Simon-Saez I, Perales S, Garrido-Navas C, Russo A, de Miguel-Perez D, et al. Exchange of cellular components between platelets and tumor cells: impact on tumor cells behavior. Theranostics. 2022;12(5):2150–61. https://doi.org/10.7150/thno.64252.
In ’t Veld S, Wurdinger T. Tumor-educated platelets. Blood. 2019;133(22):2359–64. https://doi.org/10.1182/blood-2018-12-852830.
Peng B, Wang YH, Liu YM, Ma LX. Prognostic significance of the neutrophil to lymphocyte ratio in patients with non-small cell lung cancer: a systemic review and meta-analysis. Int J Clin Exp Med. 2015;8(3):3098–106.
Gu XB, Tian T, Tian XJ, Zhang XJ. Prognostic significance of neutrophil-to-lymphocyte ratio in non-small cell lung cancer: a meta-analysis. Sci Rep. 2015;5:12493. https://doi.org/10.1038/srep12493.
Templeton AJ, McNamara MG, Seruga B, Vera-Badillo FE, Aneja P, Ocana A, et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J Natl Cancer Inst. 2014;106(6):dju124. https://doi.org/10.1093/jnci/dju124.
Jiang T, Bai Y, Zhou F, Li W, Gao G, Su C, et al. Clinical value of neutrophil-to-lymphocyte ratio in patients with non-small-cell lung cancer treated with PD-1/PD-L1 inhibitors. Lung Cancer. 2019;130:76–83. https://doi.org/10.1016/j.lungcan.2019.02.009.
Nakaya A, Kurata T, Yoshioka H, Takeyasu Y, Niki M, Kibata K, et al. Neutrophil-to-lymphocyte ratio as an early marker of outcomes in patients with advanced non-small-cell lung cancer treated with nivolumab. Int J Clin Oncol. 2018;23(4):634–40. https://doi.org/10.1007/s10147-018-1250-2.
Li M, Spakowicz D, Burkart J, Patel S, Husain M, He K, et al. Change in neutrophil to lymphocyte ratio during immunotherapy treatment is a non-linear predictor of patient outcomes in advanced cancers. J Cancer Res Clin Oncol. 2019;145(10):2541–6. https://doi.org/10.1007/s00432-019-02982-4.
Zhang N, Jiang J, Tang S, Sun G. Predictive value of neutrophil-lymphocyte ratio and platelet-lymphocyte ratio in non-small cell lung cancer patients treated with immune checkpoint inhibitors: a meta-analysis. Int Immunopharmacol. 2020;85: 106677. https://doi.org/10.1016/j.intimp.2020.106677.
Xu H, He A, Liu A, Tong W, Cao D. Evaluation of the prognostic role of platelet-lymphocyte ratio in cancer patients treated with immune checkpoint inhibitors: a systematic review and meta-analysis. Int Immunopharmacol. 2019;77: 105957. https://doi.org/10.1016/j.intimp.2019.105957.
Jiang M, Peng W, Pu X, Chen B, Li J, Xu F, et al. Peripheral blood biomarkers associated with outcome in non-small cell lung cancer patients treated with nivolumab and durvalumab monotherapy. Front Oncol. 2020;10:913. https://doi.org/10.3389/fonc.2020.00913.
Wang Y, Huang D, Xu WY, Wang YW, Che GW. Prognostic value of pretreatment lymphocyte-to-monocyte ratio in non-small cell lung cancer: a meta-analysis. Oncol Res Treat. 2019;42(10):523–31. https://doi.org/10.1159/000501726.
Katayama Y, Yamada T, Chihara Y, Tanaka S, Tanimura K, Okura N, et al. Significance of inflammatory indexes in atezolizumab monotherapy outcomes in previously treated non-small-cell lung cancer patients. Sci Rep. 2020;10(1):17495. https://doi.org/10.1038/s41598-020-74573-0.
Sekine K, Kanda S, Goto Y, Horinouchi H, Fujiwara Y, Yamamoto N, et al. Change in the lymphocyte-to-monocyte ratio is an early surrogate marker of the efficacy of nivolumab monotherapy in advanced non-small-cell lung cancer. Lung Cancer. 2018;124:179–88. https://doi.org/10.1016/j.lungcan.2018.08.012.
Sanchez-Gastaldo A, Munoz-Fuentes MA, Molina-Pinelo S, Alonso-Garcia M, Boyero L, Bernabe-Caro R. Correlation of peripheral blood biomarkers with clinical outcomes in NSCLC patients with high PD-L1 expression treated with pembrolizumab. Transl Lung Cancer Res. 2021;10(6):2509–22. https://doi.org/10.21037/tlcr-21-156.
Park W, Kwon D, Saravia D, Desai A, Vargas F, El Dinali M, et al. Develo** a Predictive model for clinical outcomes of advanced non-small cell lung cancer patients treated with nivolumab. Clin Lung Cancer. 2018;19(3):280-8 e4. https://doi.org/10.1016/j.cllc.2017.12.007.
Park W, Mezquita L, Okabe N, Chae YK, Kwon D, Saravia D, et al. Association of the prognostic model iSEND with PD-1/L1 monotherapy outcome in non-small-cell lung cancer. Br J Cancer. 2020;122(3):340–7. https://doi.org/10.1038/s41416-019-0643-y.
Kasahara N, Sunaga N, Tsukagoshi Y, Miura Y, Sakurai R, Kitahara S, et al. Post-treatment glasgow prognostic score predicts efficacy in advanced non-small-cell lung cancer treated with anti-PD1. Anticancer Res. 2019;39(3):1455–61. https://doi.org/10.21873/anticanres.13262.
Naqash AR, Stroud CRG, Butt MU, Dy GK, Hegde A, Muzaffar M, et al. Co-relation of overall survival with peripheral blood-based inflammatory biomarkers in advanced stage non-small cell lung cancer treated with anti-programmed cell death-1 therapy: results from a single institutional database. Acta Oncol. 2018;57(6):867–72. https://doi.org/10.1080/0284186X.2017.1415460.
Minami S, Ihara S, Ikuta S, Komuta K. Gustave Roussy immune score and royal marsden hospital prognostic score are biomarkers of immune-checkpoint inhibitor for non-small cell lung cancer. World J Oncol. 2019;10(2):90–100. https://doi.org/10.14740/wjon1193.
Wu Y, Wu H, Lin M, Liu T, Li J. Factors associated with immunotherapy respond and survival in advanced non-small cell lung cancer patients. Transl Oncol. 2022;15(1): 101268. https://doi.org/10.1016/j.tranon.2021.101268.
Prelaj A, Lo Russo G, Proto C, Signorelli D, Ferrara R, Galli G, et al. DiM: prognostic score for second- or further-line immunotherapy in advanced non-small-cell lung cancer: an external validation. Clin Lung Cancer. 2020;21(5):e337–48. https://doi.org/10.1016/j.cllc.2020.01.005.
Dimitrakopoulos FI, Nikolakopoulos A, Kottorou A, Kalofonou F, Liolis E, Frantzi T, et al. PIOS (Patras Immunotherapy Score) score is associated with best overall response, progression-free survival, and post-immunotherapy overall survival in patients with advanced non-small-cell lung cancer (NSCLC) treated with anti-program cell death-1 (PD-1) inhibitors. Cancers. 2020;12(5). https://doi.org/10.3390/cancers12051257.
Mountzios G, Samantas E, Senghas K, Zervas E, Krisam J, Samitas K, et al. Association of the advanced lung cancer inflammation index (ALI) with immune checkpoint inhibitor efficacy in patients with advanced non-small-cell lung cancer. ESMO Open. 2021;6(5): 100254. https://doi.org/10.1016/j.esmoop.2021.100254.
Li C, Shi M, Lin X, Zhang Y, Yu S, Zhou C, et al. Novel risk scoring system for immune checkpoint inhibitors treatment in non-small cell lung cancer. Transl Lung Cancer Res. 2021;10(2):776–89. https://doi.org/10.21037/tlcr-20-832.
Tang Y, Cui Y, Li LL, Guan YP, Feng DF, Yin BB, et al. Dynamics of early serum tumour markers and neutrophil-to-lymphocyte ratio predict response to PD-1/PD-L1 inhibitors in advanced non-small-cell lung cancer. Cancer Manag Res. 2021;13:8241–55. https://doi.org/10.2147/CMAR.S329963.
Song P, Yang D, Cui X, Wang H, Si X, Zhang X, et al. NLCIPS: non-small cell lung cancer immunotherapy prognosis score. Cancer Manag Res. 2020;12:5975–85. https://doi.org/10.2147/CMAR.S257967.
Ruiz-Banobre J, Areses-Manrique MC, Mosquera-Martinez J, Cortegoso A, Afonso-Afonso FJ, de Dios-Alvarez N, et al. Evaluation of the lung immune prognostic index in advanced non-small cell lung cancer patients under nivolumab monotherapy. Transl Lung Cancer Res. 2019;8(6):1078–85. https://doi.org/10.21037/tlcr.2019.11.07.
Sorich MJ, Rowland A, Karapetis CS, Hopkins AM. Evaluation of the lung immune prognostic index for prediction of survival and response in patients treated with atezolizumab for NSCLC: pooled analysis of clinical trials. J Thoracic Oncol. 2019;14(8):1440–6. https://doi.org/10.1016/j.jtho.2019.04.006. This study validated the lung immune prognostic index in patients with pretreated aNSCLC by a pooled analysis of randomised controlled trials with atezolizumab.
Moor R, Roberts K, Mason R, Ladwa R, Lwin Z, Hughes B, et al. P1.01–119 Modified Lung Immune Prognostic Index (mLIPI) as a predictive tool of nivolumab outcomes in advanced NSCLC patients. J Thoracic Oncol. 2019;14(10, Supplement):S408–9. https://doi.org/10.1016/j.jtho.2019.08.834.
Cortellini A, Ricciuti B, Borghaei H, Naqash AR, D'Alessio A, Fulgenzi CAM, et al. Differential prognostic effect of systemic inflammation in patients with non-small cell lung cancer treated with immunotherapy or chemotherapy: a post hoc analysis of the phase 3 OAK trial. Cancer. 2022. https://doi.org/10.1002/cncr.34348. This post-hoc analysis of a randomised controlled trial with atezolizumab for pretreated aNSCLC showed a potential predictive factor for treatment with atezolizumab of the combination of NLR and PD-L1 tumour expression.
Prelaj A, Ferrara R, Rebuzzi SE, Proto C, Signorelli D, Galli G, et al. EPSILoN: a prognostic score for immunotherapy in advanced non-small-cell lung cancer: a validation cohort. Cancers. 2019;11(12). https://doi.org/10.3390/cancers11121954.
Prelaj A, Rebuzzi SE, Pizzutilo P, Bilancia M, Montrone M, Pesola F, et al. EPSILoN: a prognostic score using clinical and blood biomarkers in advanced non-small-cell lung cancer treated with immunotherapy. Clin Lung Cancer. 2020;21(4):365-77 e5. https://doi.org/10.1016/j.cllc.2019.11.017.
Hopkins AM, Kichenadasse G, Garrett-Mayer E, Karapetis CS, Rowland A, Sorich MJ. Development and validation of a prognostic model for patients with advanced lung cancer treated with the immune checkpoint inhibitor atezolizumab. Clin Cancer Res. 2020;26(13):3280–6. https://doi.org/10.1158/1078-0432.CCR-19-2968.
Bigot F, Castanon E, Baldini C, Hollebecque A, Carmona A, Postel-Vinay S, et al. Prospective validation of a prognostic score for patients in immunotherapy phase I trials: The Gustave Roussy Immune Score (GRIm-Score). Eur J Cancer. 2017;84:212–8. https://doi.org/10.1016/j.ejca.2017.07.027.
Mielgo Rubio X, Gomez Rueda A, Antoñanzas M, Falagan S, Núñez JA, Sánchez Peña AM, et al. 1509P—applicability of lung immune prognostic index (LIPI) to predict efficacy of first-line pembrolizumab in advanced non-small cell lung cancer (NSCLC). Ann Oncol. 2019;30:v619–20. https://doi.org/10.1093/annonc/mdz260.031.
Tanaka S, Uchino J, Yokoi T, Kijima T, Goto Y, Suga Y, et al. Prognostic nutritional index and lung immune prognostic index as prognostic predictors for combination therapies of immune checkpoint inhibitors and cytotoxic anticancer chemotherapy for patients with advanced non-small cell lung cancer. Diagnostics. 2022;12(2). https://doi.org/10.3390/diagnostics12020423.
Wang W, Huang Z, Yu Z, Zhuang W, Zheng W, Cai Z, et al. prognostic value of the lung immune prognostic index may differ in patients treated with immune checkpoint inhibitor monotherapy or combined with chemotherapy for non-small cell lung cancer. Front Oncol. 2020;10: 572853. https://doi.org/10.3389/fonc.2020.572853.
Blanc-Durand F, Auclin E, Planchard D, Aix SP, Hendriks L, Sullivan IG, et al. 17P—association of lung immune prognostic index (LIPI) with survival of first line immune checkpoint inhibitors single agent or in combination with chemotherapy in untreated advanced NSCLC patients. Ann Oncol. 2019;30:xi5. https://doi.org/10.1093/annonc/mdz447.015.
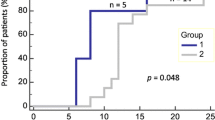
Banna GL, Cortellini A, Cortinovis DL, Tiseo M, Aerts J, Barbieri F, et al. The lung immuno-oncology prognostic score (LIPS-3): a prognostic classification of patients receiving first-line pembrolizumab for PD-L1 >/= 50% advanced non-small-cell lung cancer. ESMO Open. 2021;6(2):100078. https://doi.org/10.1016/j.esmoop.2021.100078. This study validated the NLR cut-off of 4 in aNSCLC and showed the prognostic value of the lung immuno-oncology prognostic score (LIPS-3) in real-world patients with high PD-L1 aNSCLC.
Banna GL, Tiseo M, Cortinovis DL, Facchinetti F, Aerts J, Baldessari C, et al. Host immune-inflammatory markers to unravel the heterogeneous outcome and assessment of patients with PD-L1 >/=50% metastatic non-small cell lung cancer and poor performance status receiving first-line immunotherapy. Thoracic Cancer. 2022;13(3):483–8. https://doi.org/10.1111/1759-7714.14256.
Banna GL, Signorelli D, Metro G, Galetta D, De Toma A, Cantale O, et al. Neutrophil-to-lymphocyte ratio in combination with PD-L1 or lactate dehydrogenase as biomarkers for high PD-L1 non-small cell lung cancer treated with first-line pembrolizumab. Transl Lung Cancer Res. 2020. https://doi.org/10.21037/tlcr-19-583.
Banna GL, Cantale O, Muthuramalingam S, Cave J, Comins C, Cortellini A, et al. Efficacy outcomes and prognostic factors from real-world patients with advanced non-small-cell lung cancer treated with first-line chemoimmunotherapy: the Spinnaker retrospective study. Int Immunopharmacol. 2022;110: 108985. https://doi.org/10.1016/j.intimp.2022.108985. This manuscript suggests SII might have better prognostic value than NLR in patients with aNSCLC treated with chemoimmunotherapy.
Author information
Authors and Affiliations
Contributions
Conceptualisation and methodology: G.L.B. A.A. L.M.; writing—original draft preparation: all authors; writing—review and editing and supervision: G.L.B., L.M. and A.A. All authors have made substantial contributions to this review, have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
G.L.B. reports personal fees from AstraZeneca, Astellas, travel and conference expenses from Janssen. A.F. reports personal fee from BMS, MSD, Astellas, Pfizer, Janssen, Roche, Boehringer Ingelheim, GSK, Bayer, outside the submitted work. M.T. reports personal fees from Novartis, Amgen, MSD, travel and conference expenses from Roche, BMS, Takeda, AstraZeneca, Eli Lilly. A.C. reports personal fees rom Roche, Astrazeneca, Novartis, MSD, BMS, EISAI, outside the submitted work. A.P. reports personal fees from Bristol Myers Squibb, AstraZeneca, Italfarma, grants from Roche, outside the submitted work. E.A. reports personal fees from Amgen, Sanofi, grants from Nuovo Soldati, outside the submitted work. L.M.: Research grant/Funding (self): Bristol Myers Squibb, Boehringer Ingelheim, Amgen, Stilla, Inivata; Advisory/Consultancy: Roche, Takeda; Honoraria (self): Bristol Myers Squibb, Takeda, Roche, AstraZeneca; Travel/Accommodation/Expenses: Bristol Myers Squibb, Takeda, Roche, AstraZeneca; Non-remunerated activity/ies: AstraZeneca. A.A. reports grants, personal fees and non-financial support from Bristol Myers Squibb, grants from Boehringer Ingelheim, Amgen, Stilla, Inivata, personal fees and non-financial support from Roche, Takeda, AstraZeneca, outside the submitted work. All the other authors report no disclosures.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Lung Cancer
Laura Mezquita and Alfredo Addeo equally contributed as last authors.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Banna, G.L., Friedlaender, A., Tagliamento, M. et al. Biological Rationale for Peripheral Blood Cell–Derived Inflammatory Indices and Related Prognostic Scores in Patients with Advanced Non-Small-Cell Lung Cancer. Curr Oncol Rep 24, 1851–1862 (2022). https://doi.org/10.1007/s11912-022-01335-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11912-022-01335-8