Abstract
Purpose of Review
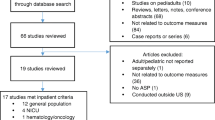
The majority of pediatric antibiotic use occurs in outpatients. However, the optimal strategies for antimicrobial stewardship in this setting are unknown. We sought to identify studies relevant to pediatric outpatient stewardship that have been published in the past decade. The details of this systemic review are presented along with targets for future stewardship efforts and discussion regarding effective outpatient stewardship strategies.
Recent Findings
In 2016, the CDC released the “Core Elements of Outpatient Antibiotic Stewardship” that serve as practical guidelines to develop impactful and sustainable ASP interventions: commitment, action for policy and practice, tracking and reporting, and education and expertise. However, there has not been a recent review of the primary medical literature on pediatric outpatient stewardship. A systematic review of pediatric antibiotic control strategies published in 2007 identified 28 studies overall, 8 of which focused on outpatients. Two subsequent systematic reviews published in 2015 and 2018 intentionally excluded outpatients.
Summary
Outpatient settings are a crucial component of pediatric antimicrobial stewardship in the USA. Establishing effective stewardship interventions can protect children and optimize clinical outcomes in outpatient healthcare settings. Based on our review of the literature, it is clear that the optimal outpatient stewardship strategies remain to be elucidated. However, there is robust literature describing variability in outpatient antibiotic prescribing that can be used to target interventions.

Similar content being viewed by others
Abbreviations
- ABS:
-
Acute bacterial sinusitis
- AOM:
-
Acute otitis media
- ASP:
-
Antimicrobial stewardship program
- AR:
-
Antimicrobial resistance
- CDC:
-
Centers for Disease Control
- CAP:
-
Community-acquired pneumonia
- EMR:
-
Electronic medical record
- GAS:
-
Group A streptococcal pharyngitis
- MeSH:
-
Medical Subject Heading
- NAMCS:
-
National Ambulatory Medical Care Survey
- SSTI:
-
Skin and soft tissue infection
- URTI:
-
Upper respiratory tract infection
- UTI:
-
Urinary tract infection
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Brennan-Krohn T, Ozonoff A, Sandora TJ. Adherence to guidelines for testing and treatment of children with pharyngitis: a retrospective study. BMC Pediatr. 2018;18(1):43.
Frost HM, McLean HQ, Chow BDW. Variability in antibiotic prescribing for upper respiratory illnesses by provider specialty. J Pediatr. 2018;203:76–+.
• Gerber JS, Prasad PA, Fiks AG, Localio AR, Grundmeier RW, Bell LM, et al. Effect of an outpatient antimicrobial stewardship intervention on broad-spectrum antibiotic prescribing by primary care pediatricians a randomized trial. JAMA-J Am Med Assoc. 2013;309(22):2345–52 This is the only randomized trial of a pediatric outpatient stewardship intervention to date.
Gerber JS, Prasad PA, Fiks AG, Localio AR, Bell LM, Keren R, et al. Durability of benefits of an outpatient antimicrobial stewardship intervention after discontinuation of audit and feedback. JAMA-J Am Med Assoc. 2014;312(23):2569–70.
Gerber JS, Prasad PA, Localio AR, et al. Variation in antibiotic prescribing across a pediatric primary care network. J Pediatr Infect Dis Soc. 2015;4(4):297–304.
Godbout EJ, Pakyz AL, Markley JD, Noda AJ, Stevens MP. Pediatric antimicrobial stewardship: state of the art. Curr Infect Dis Rep. 2018;20(10):13.
Handy LK, Bryan M, Gerber JS, Zaoutis T, Feemster KA. Variability in antibiotic prescribing for community-acquired pneumonia. Pediatrics. 2017;139(4):8.
Jaggi P, Wang L, Gleeson S, Moore-Clingenpeel M, Watson JR. Outpatient antimicrobial stewardship targets for treatment of skin and soft-tissue infections. Infect Control Hosp Epidemiol. 2018;39(8):936–40.
Kronman MP, Zhou C, Mangione-Smith R. Bacterial prevalence and antimicrobial prescribing trends for acute respiratory tract infections. Pediatrics. 2014;134(4):e956–65.
Saha D, Patel J, Buckingham D, Thornton D, Barber T, Watson JR. Urine culture follow-up and antimicrobial stewardship in a pediatric urgent care network. Pediatrics. 2017;139(4):7.
Saleh EA, Schroeder DR, Hanson AC, Banerjee R. Guideline-concordant antibiotic prescribing for pediatric outpatients with otitis media, community-acquired pneumonia, and skin and soft tissue infections in a large multispecialty healthcare system. Clin Res Infect Dis. 2015;2(1).
• Sanchez GV, Fleming-Dutra KE, Roberts RM, Hicks LA. Core Elements of Outpatient Antibiotic Stewardship. MMWR Recomm Rep. 2016;65(6):14 This CDC publication outlines key components of outpatient antimicrobial stewardship activities.
Smith MJ, Gerber JS, Hersh AL. Inpatient antimicrobial stewardship in pediatrics: a systematic review. J Pediatr Infect Dis Soc. 2015;4(4):E127–35.
Szymczak JE, Feemster KA, Zaoutis TE, Gerber JS. Pediatrician perceptions of an outpatient antimicrobial stewardship intervention. Infect Control Hosp Epidemiol. 2014;35:S69–78.
Watson JR, Wang L, Klima J, Moore-Clingenpeel M, Gleeson S, Kelleher K, et al. Healthcare claims data: an underutilized tool for pediatric outpatient antimicrobial stewardship. Clin Infect Dis. 2017;64(11):1479–85.
Weddle G, Goldman J, Myers A, Newland J. Impact of an educational intervention to improve antibiotic prescribing for nurse practitioners in a pediatric urgent care center. J Pediatr Health Care. 2017;31(2):184–8.
Funding
Dr. Kilgore was supported by the Foundation of the National Institute of Health (T32-AI007062-40, JW Sleasman, PI, and JT Kilgore, Fellow Trainee).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Jacob T. Kilgore and Michael J. Smith declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Healthcare Associated Infections
Rights and permissions
About this article
Cite this article
Kilgore, J.T., Smith, M.J. Outpatient Pediatric Antibiotic Use: a Systematic Review. Curr Infect Dis Rep 21, 14 (2019). https://doi.org/10.1007/s11908-019-0673-x
Published:
DOI: https://doi.org/10.1007/s11908-019-0673-x