Abstract
Purpose of Review
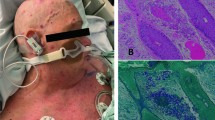
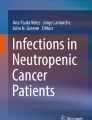
Post-transplant infections present a formidable challenge to the physician due to their varied presentation. Many of these infections begin by inoculation following skin compromise or disseminate to the skin hematogenously, making cutaneous manifestations of infection an important diagnostic clue in the immunocompromised. Quality research in this field is lacking, and this articles seeks to review the literature and present a guide to physicians in order for them to suspect certain infections by their cutaneous presentation.
Recent Findings
The cutaneous presentation of opportunistic infections in transplant patients is extremely varied. However, as more case reports are published, certain patterns specific to individual organisms are emerging. In addition, early recognition is improving outcomes and systemic antibiotic therapy success.
Summary
Early and correct recognition of disseminated infection in the immunocompromised host can be aided by close attention to cutaneous findings. This allows early and correct antibiotic therapy and improves outcomes.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Fishman JA. Infection in renal transplant recipients. Semin Nephrol. 2007;27(4):445–61. https://doi.org/10.1016/j.semnephrol.2007.03.006.
Gentry LO, Zeluff B, Kielhofner MA. Dermatologic manifestations of infectious diseases in cardiac transplant patients. Infect Dis Clin N Am. 1994;8(3):637–54.
Kurnatowski P. Some aspects of multifocal and disseminated mycosis. Wiad Parazytol. 2004;50(3):359–65.
Wolfson JS, Sober AJ, Rubin RH. Dermatologic manifestations of infections in immunocompromised patients. Medicine (Baltimore). 1985;64(2):115–33.
Ray T. Cutaneous signs of systemic disease: fungal infections in the immunocompromised host. Med Clin North Am 1980;64(5):955-68. https://doi.org/10.1016/S0025-7125(16)31576-0
Davies SF, Sarosi GA, Peterson PK, Khan M, Howard RJ, Simmons RL, et al. Disseminated histoplasmosis in renal transplant recipients. Am J Surg. 1979;137(5):686–91.
Alvarez M, Burn T, Luo Y, Pirofski LA, Casadevall A. The outcome of Cryptococcus neoformans intracellular pathogenesis in human monocytes. BMC Microbiol. 2009;9:51. https://doi.org/10.1186/1471-2180-9-51.
Radentz WH. Opportunistic fungal infections in immunocompromised hosts. J Am Acad Dermatol. 1989;20(6):989–1003.
Gao LW, Jiao AX, Wu XR, Zhao SY, Ma Y, Liu G, et al. Clinical characteristics of disseminated cryptococcosis in previously healthy children in China. BMC Infect Dis. 2017;17(1):359. https://doi.org/10.1186/s12879-017-2450-5.
Abel EA. Cutaneous manifestations of immunosuppression in organ transplant recipients. J Am Acad Dermatol. 1989;21(2 Pt 1):167–79.
Sun HY, Alexander BD, Lortholary O, Dromer F, Forrest GN, Lyon GM, et al. Cutaneous cryptococcosis in solid organ transplant recipients. Med Mycol. 2010;48(6):785–91. https://doi.org/10.3109/13693780903496617.
Schupbach CW, Wheeler CE, Briggaman RA, Warner NA, Kanof EP. Cutaneous manifestations of disseminated cryptococcosis. Arch Dermatol. 1976;112(12):1734–40.
Kurowski R, Ostapchuk M. Overview of histoplasmosis. Am Fam Physician. 2002;66(12):2247–52.
Olivero JJ, Lozano-Mendez J, Ghafary EM, Eknoyan G, Suki WN. Mitigation of amphotericin B nephrotoxicity by mannitol. Br Med J. 1975;1(5957):550–1.
Seçkin D, Güleç TO, Demirağ A, Bilgin N. Renal transplantation and skin diseases. Transplant Proc. 1998;30(3):802–4.
Kauffman CA. Diagnosis of histoplasmosis in immunosuppressed patients. Curr Opin Infect Dis. 2008;21(4):421–5. https://doi.org/10.1097/QCO.0b013e328306eb8d.
Ben-Ami R, Lewis RE, Kontoyiannis DP. Enemy of the (immunosuppressed) state: an update on the pathogenesis of Aspergillus fumigatus infection. Br J Haematol. 2010;150(4):406–17. https://doi.org/10.1111/j.1365-2141.2010.08283.x.
Muldoon EG, Strek ME, Patterson KC. Allergic and noninvasive infectious pulmonary Aspergillosis syndromes. Clin Chest Med. 2017;38(3):521–34. https://doi.org/10.1016/j.ccm.2017.04.012.
• Burke VE, Lopez FA. Approach to skin and soft tissue infections in non-HIV immunocompromised hosts. Curr Opin Infect Dis. 2017;30(4):354–63. https://doi.org/10.1097/QCO.0000000000000378. Comprehensive review of cutanoeus infections in immunocompromised hosts. Article is notable for table detailingl diagnostic steps for each pathogen, as well as table displaying missing part of host immune system that makes host most vulnerable to each pathogen.
Prystowsky SD, Vogelstein B, Ettinger DS, Merz WG, Kaizer H, Sulica VI, et al. Invasive aspergillosis. N Engl J Med. 1976;295(12):655–8. https://doi.org/10.1056/NEJM197609162951206.
•• Ilyas M, Sharma A. Cutaneous fungal infections in solid organ transplant recipients. Transplant Rev (Orlando). 2017;31(3):158–65. https://doi.org/10.1016/j.trre.2017.03.001. Recent review of cutaneous fungal infections in organ transplant patients. Review has helpful table organizing pathogens based on the type of dermatological lesion they cause.
Schwartz RA. Superficial fungal infections. Lancet. 2004;364(9440):1173–82. https://doi.org/10.1016/S0140-6736(04)17107-9.
Goldberg LJ, Wise EM, Miller NS. White piedra caused by Trichosporon inkin: a report of two cases in a northern climate. Br J Dermatol. 2015;173(3):866–8. https://doi.org/10.1111/bjd.13824.
Murray-Leisure KA, Aber RC, Rowley LJ, Applebaum PC, Wisman CB, Pennock JL, et al. Disseminated Trichosporon beigelii (cutaneum) infection in an artificial heart recipient. JAMA. 1986;256(21):2995–8.
Virgili A, Zampino MR, Mantovani L. Fungal skin infections in organ transplant recipients. Am J Clin Dermatol. 2002;3(1):19–35.
Chapman SW, Lin AC, Hendricks KA, Nolan RL, Currier MM, Morris KR, et al. Endemic blastomycosis in Mississippi: epidemiological and clinical studies. Semin Respir Infect. 1997;12(3):219–28.
Saccente M, Woods GL. Clinical and laboratory update on blastomycosis. Clin Microbiol Rev. 2010;23(2):367–81. https://doi.org/10.1128/CMR.00056-09.
Ryan ME, Ochs D, Ochs J. Primary cutaneous mucormycosis: superficial and gangrenous infections. Pediatr Infect Dis. 1982;1(2):110–4.
Meyer RD, Kaplan MH, Ong M, Armstrong D. Cutaneous lesions in disseminated mucormycosis. JAMA. 1973;225(7):737–8.
Kanaan IC, Santos TB, Kac BK, Souza AM, Cerqueira AM. Majocchi's granuloma—case report. An Bras Dermatol. 2015;90(2):251–3. https://doi.org/10.1590/abd1806-4841.20153115.
Virgili A, Zampino MR. Relapsing tinea capitis by Microsporum canis in an adult female renal transplant recipient. Nephron. 1998;80(1):61–2.
Piraccini BM, Morelli R, Stinchi C, Tosti A. Proximal subungual onychomycosis due to Microsporum canis. Br J Dermatol. 1996;134(1):175–7.
Craun GF, Calderon RL, Craun MF. Outbreaks associated with recreational water in the United States. Int J Environ Health Res. 2005;15(4):243–62. https://doi.org/10.1080/09603120500155716.
Greene SL, Su WP, Muller SA. Pseudomonas aeruginosa infections of the skin. Am Fam Physician. 1984;29(1):193–200.
O'Sullivan GM, Worsnop F, Natkunarajah J. Ecthyma gangrenosum, an important cutaneous infection to recognize in the immunosuppressed patient. Clin Exp Dermatol. 2017;43:67–9. https://doi.org/10.1111/ced.13253.
Vaiman M, Lazarovitch T, Heller L, Lotan G. Ecthyma gangrenosum and ecthyma-like lesions: review article. Eur J Clin Microbiol Infect Dis. 2015;34(4):633–9. https://doi.org/10.1007/s10096-014-2277-6.
Chan YH, Chong CY, Puthucheary J, Loh TF. Ecthyma gangrenosum: a manifestation of Pseudomonas sepsis in three paediatric patients. Singap Med J. 2006;47(12):1080–3.
Frey JD, Latkowski JA, Louie E, Chiu ES. Diagnosis and management of ecthyma gangrenosum in chronic renal failure patient. Arch Plast Surg. 2014;41(3):299–301. https://doi.org/10.5999/aps.2014.41.3.299.
Asensio A, Ramos A, Cuervas-Mons V, Cordero E, Sánchez-Turrión V, Blanes M, et al. Effect of antibiotic prophylaxis on the risk of surgical site infection in orthotopic liver transplant. Liver Transpl. 2008;14(6):799–805. https://doi.org/10.1002/lt.21435.
Ramos A, Asensio A, Muñez E, Torre-Cisneros J, Montejo M, Aguado JM, et al. Incisional surgical site infection in kidney transplantation. Urology. 2008;72(1):119–23. https://doi.org/10.1016/j.urology.2007.11.030.
Saliba WR, Goldstein LH, Raz R, Mader R, Colodner R, Elias MS. Subacute necrotizing fasciitis caused by gas-producing Staphylococcus aureus. Eur J Clin Microbiol Infect Dis. 2003;22(10):612–4. https://doi.org/10.1007/s10096-003-1023-2.
Coussement J, Lebeaux D, van Delden C, Guillot H, Freund R, Marbus S, et al. Nocardia infection in solid organ transplant recipients: a multicenter European case-control study. Clin Infect Dis. 2016;63(3):338–45. https://doi.org/10.1093/cid/ciw241.
Lebeaux D, Morelon E, Suarez F, Lanternier F, Scemla A, Frange P, et al. Nocardiosis in transplant recipients. Eur J Clin Microbiol Infect Dis. 2014;33(5):689–702. https://doi.org/10.1007/s10096-013-2015-5.
Kim YK, Oh JR, Choi HK, Kim HY, Park SD, Uh Y. Primary cutaneous nocardiosis caused by Nocardia nova in a kidney transplant recipient. J Med Microbiol. 2014;63(Pt 1):140–3. https://doi.org/10.1099/jmm.0.054239-0.
Singh N, Paterson DL. Mycobacterium tuberculosis infection in solid-organ transplant recipients: impact and implications for management. Clin Infect Dis. 1998;27(5):1266–77.
Voigtländer T, Cornberg M, Gottlieb J, Welte T, Suerbaum S, Bange FC. When a respiratory pathogen turns to the skin: cutaneous tuberculosis in a lung transplant patient. Ther Adv Respir Dis. 2015;9(5):260–2. https://doi.org/10.1177/1753465815581152.
van Zyl L, du Plessis J, Viljoen J. Cutaneous tuberculosis overview and current treatment regimens. Tuberculosis (Edinb). 2015;95(6):629–38. https://doi.org/10.1016/j.tube.2014.12.006.
Parker L, Babu S. Tuberculous gumma: a forgotten entity in the UK. BMJ Case Rep. 2013;2013:bcr2013010462. https://doi.org/10.1136/bcr-2013-010462.
Kothavade RJ, Dhurat RS, Mishra SN, Kothavade UR. Clinical and laboratory aspects of the diagnosis and management of cutaneous and subcutaneous infections caused by rapidly growing mycobacteria. Eur J Clin Microbiol Infect Dis. 2013;32(2):161–88. https://doi.org/10.1007/s10096-012-1766-8.
Pinto-Gouveia M, Gameiro A, Ramos L, Cardoso JC, Brites MM, Tellechea Ó, et al. Mycobacterium chelonae is an ubiquitous atypical Mycobacterium. Case Rep Dermatol. 2015;7(2):207–11. https://doi.org/10.1159/000438898.
Lee MR, Sheng WH, Hung CC, Yu CJ, Lee LN, Hsueh PR. Mycobacterium abscessus complex infections in humans. Emerg Infect Dis. 2015;21(9):1638–46. https://doi.org/10.3201/2109.141634.
Sette CS, Wachholz PA, Masuda PY, da Costa Figueira RB, de Oliveira Mattar FR, Ura DG. Mycobacterium marinum infection: a case report. J Venom Anim Toxins Incl Trop Dis. 2015;21:7. https://doi.org/10.1186/s40409-015-0008-9.
Arduino PG, Porter SR. Herpes simplex virus type 1 infection: overview on relevant clinico-pathological features. J Oral Pathol Med. 2008;37(2):107–21. https://doi.org/10.1111/j.1600-0714.2007.00586.x.
Tan HH, Goh CL. Viral infections affecting the skin in organ transplant recipients: epidemiology and current management strategies. Am J Clin Dermatol. 2006;7(1):13–29.
Hiok-Hee T, Chee-Leok G. Viral infections affecting the skin in organ transplant recipients: epidemiology and current management strategies. Am J Clin Dermatol. 2006;7(1):13–29.
Smith SR, Butterly DW, Alexander BD, Greenberg A. Viral infections after renal transplantation. Am J Kidney Dis. 2001;37(4):659–76.
Brennan DC. Cytomegalovirus in renal transplantation. J Am Soc Nephrol. 2001;12(4):848–55.
Lesher JL. Cytomegalovirus infections and the skin. J Am Acad Dermatol. 1988;18(6):1333–8.
Camargo JF, Komanduri KV. Emerging concepts in cytomegalovirus infection following hematopoietic stem cell transplantation. Hematol Oncol Stem Cell Ther. 2017;10:233–8. https://doi.org/10.1016/j.hemonc.2017.05.001.
Mccarthy JT, Hoagland RJ. Cutaneous manifestations of infectious mononucleosis. JAMA. 1964;187:153–4.
Greenspan JS, Greenspan D, Webster-Cyriaque J. Hairy leukoplakia; lessons learned: 30-plus years. Oral Dis. 2016;22(Suppl 1):120–7. https://doi.org/10.1111/odi.12393.
Jenkins FJ, Hoffman LJ, Liegey-Dougall A. Reactivation of and primary infection with human herpesvirus 8 among solid-organ transplant recipients. J Infect Dis. 2002;185(9):1238–43. https://doi.org/10.1086/340237.
Andrei G, Snoeck R. Kaposi's sarcoma-associated herpesvirus: the role of lytic replication in targeted therapy. Curr Opin Infect Dis. 2015;28(6):611–24. https://doi.org/10.1097/QCO.0000000000000213.
•• Ilyas M, Maganty N, Sharma A. Cutaneous infections from viral sources in solid organ transplant recipients. J Clin Virol. 2017;97:33–7. https://doi.org/10.1016/j.jcv.2017.08.007. Recent review of cutaneous viral infection in organ transplant patients. Review is notable for table listing pathogens along with their major dermatologic syndromes.
Rüdlinger R, Smith IW, Bunney MH, Hunter JA. Human papillomavirus infections in a group of renal transplant recipients. Br J Dermatol. 1986;115(6):681–92.
Euvrard S, Kanitakis J, Cochat P, Cambazard F, Claudy A. Skin diseases in children with organ transplants. J Am Acad Dermatol. 2001;44(6):932–9. https://doi.org/10.1067/mjd.2001.113465.
Puri N. A study on the use of imiquimod for the treatment of genital molluscum contagiosum and genital warts in female patients. Indian J Sex Transm Dis. 2009;30(2):84–8. https://doi.org/10.4103/0253-7184.62763.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Cory J Pettit, Katherine Mazurek, and Benjamin Kaffenberger declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Transplant and Oncology
Rights and permissions
About this article
Cite this article
Pettit, C.J., Mazurek, K. & Kaffenberger, B. Cutaneous Manifestations of Infections in Solid Organ Transplant Recipients. Curr Infect Dis Rep 20, 16 (2018). https://doi.org/10.1007/s11908-018-0621-1
Published:
DOI: https://doi.org/10.1007/s11908-018-0621-1