Abstract
Purpose of Review
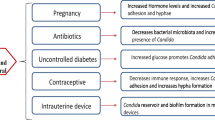
This review includes a detailed overview of the vaginal yeast infection based on current literature available, addressing etiology, epidemiology, risk factors, and pathophysiology, as well as clinical presentation, burden, diagnostic, and treatment strategies.
Recent Findings
There are multiple meta-analyses, systematic reviews, randomized control trials, and critical reviews recently published that have advanced the understanding of pathophysiology and answered questions regarding global burden, prevention, and treatment in a systematic way.
Summary
In the recent years, important work has been made to better understand the pathophysiology and global burden behind the vaginal yeast infection. Diagnostic criteria were proposed for chronic vulvovaginal candidiasis. While fluconazole resistance has been making maintenance suppressive therapy of recurrent vulvovaginal candidiasis difficult and probiotics do not seem to be very effective, significant improvements and advances in the area of antifungal therapeutic innovation research have been made and further results of vaccine trials are pending. There is a need for well-designed RCTs in evidence-based treatment development and research.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Sobel JD. Recurrent vulvovaginal candidiasis. Am J Obstet Gynecol. 2016;214(1):15–21. https://doi.org/10.1016/j.ajog.2015.06.067.
Reichman O, Margesson LJ, Rasmussen CA, Lev-Sagie A, Sobel JD. Algorithms for managing vulvovaginal symptoms-a practical primer. Curr Infect Dis Rep. 2019;21(10):40. https://doi.org/10.1007/s11908-019-0693-6.
Sobel JD. Vulvovaginal candidosis. Lancet. 2007;369(9577):1961–71. https://doi.org/10.1016/S0140-6736(07)60917-9.
Gonçalves B, Ferreira C, Alves CT, Henriques M, Azeredo J, Silva S. Vulvovaginal candidiasis: epidemiology, microbiology and risk factors. Crit Rev Microbiol. 2016;42(6):905–27. https://doi.org/10.3109/1040841X.2015.1091805.
Petrova MI, Lievens E, Malik S, Imholz N, Lebeer S. Lactobacillus species as biomarkers and agents that can promote various aspects of vaginal health. Front Physiol. 2015;6:81. https://doi.org/10.3389/fphys.2015.00081.
Kalia N, Singh J, Kaur M. Microbiota in vaginal health and pathogenesis of recurrent vulvovaginal infections: a critical review. Ann Clin Microbiol Antimicrob. 2020;19(1):5. https://doi.org/10.1186/s12941-020-0347-4.
• Bradford LL, Ravel J. The vaginal mycobiome: a contemporary perspective on fungi in women’s health and diseases. Virulence. 2017;8(3):342–51. https://doi.org/10.1080/21505594.2016.1237332Enlightens vaginal mycobiome and mechanisms of commensalism and disease.
Landers DV, Wiesenfeld HC, Heine RP, Krohn MA, Hillier SL. Predictive value of the clinical diagnosis of lower genital tract infection in women. Am J Obstet Gynecol. 2004;190:1004–10.
Drell T, Lillsaar T, Tummeleht L, Simm J, Aaspõllu A, Väin E, et al. Characterization of the vaginal micro-and mycobiome in asymptomatic reproductive-age estonian women. PLoS One. 2013;8(1):e54379. https://doi.org/10.1371/journal.pone.0054379.
Ene IV, Cheng SC, Netea MG, Brown AJP. Growth of Candida albicans cells on the physiologically relevant carbon source lactate affects their recognition and phagocytosis by immune cells. Infect Immun. 2012;81:238–48. https://doi.org/10.1128/IAI.01092-12.
Niu XX, Li T, Zhang X, Wang SX, Liu ZH. Lactobacillus crispatus modulates vaginal epithelial cell innate response to Candida albicans. Chin Med J. 2017;130(3):273. https://doi.org/10.4103/0366-6999.198927.
Amjadi F, Salehi E, Mehdizadeh M, Aflatoonian R. Role of the innate immunity in female reproductive tract. Adv Biomed Res. 2014;3:1. https://doi.org/10.4103/2277-9175.124626.
Pear GT, French AL, Gilbert D, Zariffard MR, Mirmonsef P, Sullivan TH, et al. Human α-amylase present in lower-genital-tract mucosal fluid processes glycogen to support vaginal colonization by Lactobacillus. J Infect Dis. 2014;210(7):1019–28. https://doi.org/10.1093/infdis/jiu231.
Blostein F, Levin-Sparenberg E, Wagner J, Foxman B. Recurrent vulvovaginal candidiasis. Ann Epidemiol. 2017;27:575–582.e3.
Hong E, Dixit S, Fidel PL, Bradford J, Fischer G. Vulvovaginal candidiasis as a chronic disease: diagnostic criteria and definition. J Low Genit Tract Dis. 2014;18(1):31–8. https://doi.org/10.1097/LGT.0b013e318287aced.
•• Denning DW, Kneale M, Sobel JD, Rautemaa-Richardson R. Global burden of recurrent vulvovaginal candidiasis: a systematic review. Lancet Infect Dis. 2018;18(11):e339–47. https://doi.org/10.1016/S1473-3099(18)30103-8Represents global burden of VYI in numbers.
Donders GGG, Ravel J, Vitali B, Netea MG, Salumets A, Unemo M. Role of molecular biology in diagnosis and characterization of vulvo-vaginitis in clinical practice. Gynecol Obstet Investig. 2017;82(6):607–16. https://doi.org/10.1159/000478982.
van der Meijden WI, Boffa MJ, Ter Harmsel WA, et al. 2016 European guideline for the management of vulval conditions. J Eur Acad Dermatol Venereol. 2017;31(6):925–41. https://doi.org/10.1111/jdv.14096.
van Schalkwyk J, Yudin MH. Infectious Disease Committee. Vulvovaginitis: screening for and management of trichomoniasis, vulvovaginal candidiasis, and bacterial vaginosis. J Obstet Gynaecol Can. 2015;37(3):266–74. https://doi.org/10.1016/S1701-2163(15)30316-9.
Pappas PG, Kauffman CA, Andes DR, Clancy CJ, Marr KA, Ostrosky-Zeichner L, et al. Clinical practice guideline for the management of candidiasis: 2016 update by the infectious diseases society of America. Clin Infect Dis. 2016;62:e1–e50. https://doi.org/10.1093/cid/civ933.
Owen MK, Clenney TL. Management of vaginitis. Am Fam Physician. 2004;70:2125–32.
Houang ET, Chappatte O, Byrne D, Macrae PV, Thorpe JE. Fluconazole levels in plasma and vaginal secretions of patients after a 150-milligram single oral dose and rate of eradication of infection in vaginal candidiasis. Antimicrob Agents Chemother. 1990;34:909–10.
Sobel JD, Vazquez JA. Symptomatic vulvovaginitis due to fluconazole-resistant Candida albicans in a female who was not infected with human immunodeficiency virus. Clin Infect Dis. 1996;22:726–7.
Sobel JD, Kapernick PS, Zervos M, Reed BD, Hooton T, Soper D, et al. Treatment of complicated Candida vaginitis: comparison of single and sequential doses of fluconazole. Am J Obstet Gynecol. 2001;185:363–9.
Sobel JD, Faro S, Force RW, Foxman B, Ledger WJ, Nyirjesy PR, et al. Vulvovaginal candidiasis: epidemiologic, diagnostic, and therapeutic considerations. Am J Obstet Gynecol. 1998;178:203–11.
Willems HME, Ahmed SS, Liu J, Xu Z, Peters BM. Vulvovaginal candidiasis: a current understanding and burning questions. J. Fungi. 2020;6:27. https://doi.org/10.3390/jof6010027.
Sobel JD, Kapernick PS, Zervos M, Reed BD, Hooton T, Soper D, et al. Treatment of complicated Candida vaginitis: comparison of single and sequential doses of fluconazole. Am J Obstet Gynecol. 2001;185:363–9.
Collins LM, Moore R, Sobel JD. Prognosis and long-term outcome of women with idiopathic recurrent vulvovaginal candidiasis caused by Candida albicans. J Low Genit Tract Dis. 2020;24:48–52.
Sobel JD. Candida vulvovaginitis: treatment – up to date. Wolters Kluwer. https://www.uptodate.com/contents/candida-vulvovaginitis-treatment?search=vulvovaginitois&source=search_result&selectedTitle=3~150&usage_type=default&display_rank=3 (Accessed in June 2020; last update, Jun 01, 2020).
• Lírio J, Giraldo PC, Amaral RL, Sarmento ACA, APF C, Gonçalves AK. Antifungal (oral and vaginal) therapy for recurrent vulvovaginal candidiasis: a systematic review protocol. BMJ Open. 2019;9(5):e027489. https://doi.org/10.1136/bmjopen-2018-027489Pending to identify the most effective and safe oral and intravaginal antifungal agents.
•• Zhang Z, Zhang X, Zhou YY, Jiang CM, Jiang HY. The safety of oral fluconazole during the first trimester of pregnancy: a systematic review and meta-analysis. BJOG. 2019;126(13):1546–52. https://doi.org/10.1111/1471-0528.15913In pregnancy oral fluconazole during the first trimester may be associated with heart malformations and spontaneous abortion.
US Food and Drug Administration. Safety communication: Oral fluconazole in pregnancy. http://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm497656.htm?source=gov delivery&utm_medium=email&utm_source=govdelivery (Accessed in June 2020, released on April 26, 2016).
Sobel JD, Chaim W. Treatment of Torulopsis glabrata vaginitis: retrospective review of boric acid therapy. Clin Infect Dis. 1997;24:649–52.
Sobel JD, Chaim W, Nagappan V, Leaman D. Treatment of vaginitis caused by Candida glabrata: use of topical boric acid and flucytosine. Am J Obstet Gynecol. 2003;189:1297–300.
•• Alves IA, Savi FM, de Vasconcelos C, Braz J, Quintans Junior LJ, Serafini MR. The patenting and technological trends in candidiasis treatment: a systematic review (2014–2018). Curr Top Med Chem. 2019;19(28):2629–39. https://doi.org/10.2174/1568026619666191030091211Identified significant improvements and advances in the area of antifungal therapeutic innovation research.
Cassone A. Vulvovaginal Candida albicans infections: pathogenesis, immunity and vaccine prospects. BJOG. 2015;122:785–94.
•• Edwards JE Jr, Schwartz MM, Schmidt CS, et al. A fungal immunotherapeutic vaccine (NDV-3A) for treatment of recurrent vulvovaginal candidiasis-a phase 2 randomized, double-blind, placebo-controlled trial. Clin Infect Dis. 2018;66(12):1928–36. https://doi.org/10.1093/cid/ciy185Therapeutic vaccine could enhance or rectify tolerance/inflammation imbalance in the vagina.
•• van de Wijgert J, Verwijs MC. Lactobacilli-containing vaginal probiotics to cure or prevent bacterial or fungal vaginal dysbiosis: a systematic review and recommendations for future trial designs. BJOG. 2020;127(2):287–99. https://doi.org/10.1111/1471-0528.15870Vaginal probiotics don’t seem to be very effective.
Hillier SL. The need for better evidence to support probiotics for vaginitis. BJOG. 2020;127(2):300. https://doi.org/10.1111/1471-0528.15910.
Ali S, Ashraf U, Shah F, Ali O, Hayes K, Oakeshott P. Re: lactobacilli-containing vaginal probiotics to cure or prevent bacterial or fungal vaginal dysbiosis: a systematic review and recommendations for future trial designs. BJOG. 2020;127(2):304–5. https://doi.org/10.1111/1471-0528.15961.
•• **e HY, Feng D, Wei DM, et al. Probiotics for vulvovaginal candidiasis in non-pregnant women. Cochrane Database Syst Rev. 2017;11(11):CD010496. Published 2017 Nov 23. https://doi.org/10.1002/14651858.CD010496.pub2Vaginal probiotics don’t bring a higher frequency of long-term clinical or mycological cure.
Russo R, Superti F, Karadja E, De Seta F. Randomised clinical trial in women with recurrent Vulvovaginal candidiasis: efficacy of probiotics and lactoferrin as maintenance treatment. Mycoses. 2019;62(4):328–35. https://doi.org/10.1111/myc.12883.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Mija Blaganje and Matija Barbič declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Inflammatory/Infectious Bladder Disorders
Rights and permissions
About this article
Cite this article
Blaganje, M., Barbič, M. Vaginal Yeast Infection. Curr Bladder Dysfunct Rep 15, 325–331 (2020). https://doi.org/10.1007/s11884-020-00606-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11884-020-00606-z