Abstract
Background
Enhanced recovery programmes in laparoscopic colorectal surgery (LCS) employ combined approaches to achieve postoperative analgesia. Transversus abdominis plane (TAP) block is a locoregional anaesthetic technique that may reduce postoperative pain.
Aims
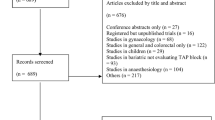
To perform a systematic review and meta-analysis to compare the effectiveness of laparoscopic- versus ultrasound-guided TAP block in LCS.
Methods
Databases were searched for relevant articles from inception until March 2022. All randomised controlled trials (RCTs) that compared laparoscopic (LTB) versus ultrasound-guided (UTB) TAP blocks in LCS were included. The primary outcome was narcotic consumption at 24 h postoperatively, whilst secondary outcomes included pain scores at 24 h postoperatively, operative time, postoperative nausea and vomiting (PONV) and complication rates. Random effects models were used to calculate pooled effect size estimates.
Results
Three RCTs were included capturing 219 patients. Studies were clinically heterogenous. On random effects analysis, LTB was associated with significantly lower narcotic consumption (SMD − 0.30 mg, 95% CI = − 0.57 to − 0.03, p = 0.03) and pain scores (SMD − 0.29, 95% CI = − 0.56 to − 0.03, p = 0.03) at 24 h. However, there were no differences in operative time (SMD − 0.09 min, 95% CI = − 0.40 to 0.22, p = 0.56), PONV (OR = 0.97, 95% CI = 0.36 to 2.65, p = 0.96) or complication (OR = 1.30, 95% CI = 0.64 to 2.64, p = 0.47) rates.
Conclusions
LTB is associated with significantly less narcotic usage and pain at 24 h postoperatively but similar PONV, operative time and complication rates, compared to UTB. However, the data were inconsistent, and our findings require further investigation. LTB obviates the need for ultrasound devices whilst also decreasing procedure logistical complexity.






Similar content being viewed by others
Availability of data and material
N/A.
Code availability
RevMan, version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2012.
References
Muller S, Zalunardo MP, Hubner M et al (2009) A fast-track program reduces complications and length of hospital stay after open colonic surgery. Gastroenterology 136(3):842–847. https://doi.org/10.1053/j.gastro.2008.10.030
Spanjersberg WR, Reurings J, Keus F et al (2011) Fast track surgery versus conventional recovery strategies for colorectal surgery. The Cochrane Database of Systematic Reviews (2):CD007635. https://doi.org/10.1002/14651858.CD007635.pub2
Lassen K, Soop M, Nygren J et al (2009) Consensus review of optimal perioperative care in colorectal surgery: Enhanced Recovery After Surgery (ERAS) Group recommendations. Arch Surg 144(10):961–969. https://doi.org/10.1001/archsurg.2009.170
Wilmore DW, Kehlet H (2001) Management of patients in fast track surgery. BMJ 322(7284):473–476. https://doi.org/10.1136/bmj.322.7284.473
Rafi AN (2001) Abdominal field block: a new approach via the lumbar triangle. Anaesthesia 56(10):1024–1026. https://doi.org/10.1046/j.1365-2044.2001.02279-40.x
McDonnell JG, O’Donnell B, Curley G et al (2007) The analgesic efficacy of transversus abdominis plane block after abdominal surgery: a prospective randomized controlled trial. Anesth Analg 104(1):193–197. https://doi.org/10.1213/01.ane.0000250223.49963.0f
Hain E, Maggiori L, AlDJ P, Panis Y (2018) Transversus abdominis plane (TAP) block in laparoscopic colorectal surgery improves postoperative pain management: a meta-analysis. Colorectal Dis 20(4):279–287. https://doi.org/10.1111/codi.14037
Fields AC, Weiner SG, Maldonado LJ et al (2020) Implementation of liposomal bupivacaine transversus abdominis plane blocks into the colorectal enhanced recovery after surgery protocol: a natural experiment. Int J Colorectal Dis 35(1):133–138. https://doi.org/10.1007/s00384-019-03457-1
Milan Z, Tabor D, McConnell P et al (2011) Three different approaches to Transversus abdominis planeblock: a cadaveric study. Med Glas (Zenica) 8(2):181–184
Oh TK, Yim J, Kim J et al (2017) Effects of preoperative ultrasound-guided transversus abdominis plane block on pain after laparoscopic surgery for colorectal cancer: a double-blind randomized controlled trial. Surg Endosc 31(1):127–134. https://doi.org/10.1007/s00464-016-4941-7
Walter CJ, Maxwell-Armstrong C, Pinkney TD et al (2013) A randomised controlled trial of the efficacy of ultrasound-guided transversus abdominis plane (TAP) block in laparoscopic colorectal surgery. Surg Endosc 27(7):2366–2372. https://doi.org/10.1007/s00464-013-2791-0
Devane LA, Khan F, Murphy E et al (2020) Laparoscopic guided transversus abdominis plane block for abdominal surgery - a video vignette. Colorectal Dis 22(2):221–222. https://doi.org/10.1111/codi.14848
Favuzza J, Delaney CP (2013) Laparoscopic-guided transversus abdominis plane block for colorectal surgery. Dis Colon Rectum 56(3):389–391. https://doi.org/10.1097/DCR.0b013e318280549b
Favuzza J, Brady K, Delaney CP (2013) Transversus abdominis plane blocks and enhanced recovery pathways: making the 23-h hospital stay a realistic goal after laparoscopic colorectal surgery. Surg Endosc 27(7):2481–2486. https://doi.org/10.1007/s00464-012-2761-y
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700. https://doi.org/10.1136/bmj.b2700
Shea BJ, Grimshaw JM, Wells GA et al (2007) Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol 7:10. https://doi.org/10.1186/1471-2288-7-10
DerSimonian R, Laird N (2015) Meta-analysis in clinical trials revisited. Contemp Clin Trials 45(Pt A):139–145. https://doi.org/10.1016/j.cct.2015.09.002
Jadad AR, Moore RA, Carroll D et al (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17(1):1–12. https://doi.org/10.1016/0197-2456(95)00134-4
Colibaseanu DT, Osagiede O, Merchea A et al (2019) Randomized clinical trial of liposomal bupivacaine transverse abdominis plane block versus intrathecal analgesia in colorectal surgery. Br J Surg 106(6):692–699. https://doi.org/10.1002/bjs.11141
Nagata J, Watanabe J, Sawatsubashi Y et al (2018) A novel transperitoneal abdominal wall nerve block for postoperative pain in laparoscopic colorectal surgery. Asian J Surg 41(5):417–421. https://doi.org/10.1016/j.asjsur.2017.02.006
Park SY, Park JS, Choi GS et al (2017) Comparison of analgesic efficacy of laparoscope-assisted and ultrasound-guided transversus abdominis plane block after laparoscopic colorectal operation: a randomized, single-blind, non-inferiority trial. J Am Coll Surg 225(3):403–410. https://doi.org/10.1016/j.jamcollsurg.2017.05.017
Wong DJ, Curran T, Poylin VY et al (2019) Surgeon-delivered laparoscopic transversus abdominis plane blocks are non-inferior to anesthesia-delivered ultrasound-guided transversus abdominis plane blocks: a blinded, randomized non-inferiority trial. Surg Endosc. https://doi.org/10.1007/s00464-019-07097-y
Zaghiyan KN, Mendelson BJ, Eng MR et al (2019) Randomized clinical trial comparing laparoscopic versus ultrasound-guided transversus abdominis plane block in minimally invasive colorectal surgery. Dis Colon Rectum 62(2):203–210. https://doi.org/10.1097/DCR.0000000000001292
Peltrini R, Cantoni V, Green R et al (2020) Efficacy of transversus abdominis plane (TAP) block in colorectal surgery: a systematic review and meta-analysis. Tech Coloproctol 24(8):787–802
Allaix ME, Degiuli M, Bonino MA et al (2019) Intracorporeal or extracorporeal ileocolic anastomosis after laparoscopic right colectomy: a double-blinded randomized controlled trial. Ann Surg 270(5):762–767. https://doi.org/10.1097/SLA.0000000000003519
Arthur R, Feldman H, Covino B (1988) Comparative pharmacokinetics of bupivacaine and ropivacaine, a new amide local anesthetic. Anesth Analg 67(11):1053–1058
Byrnes K, Sahebally S, Burke J (2020) Effect of liposomal bupivacaine on opioid requirements and length of stay in colorectal enhanced recovery pathways: a systematic review and network meta-analysis. Colorectal Dis 23(3):603–613
Stokes A, Adhikary S, Quintili A, Puleo F (2017) Liposomal bupivacaine use in transversus abdominis plane blocks reduces pain and postoperative intravenous opioid requirement after colorectal surgery. Dis Colon Rectum 60(2):170–177
Chahar P, Cummings KC (2012) Liposomal bupivacaine: a review of a new bupivacaine formulation. J Pain Res 5:257–264
Escudero-Fung M, Lehman E, Karamchandani K (2020) Timing of transversus abdominis plane block and postoperative pain management. Local Reg Anesth 13:185–193
Joris J, Thiry E, Paris P et al (1995) Pain after laparoscopic cholecystectomy: characteristics and effect of intraperitoneal bupivacaine. Anesth Analg 81(2):379–384. https://doi.org/10.1097/00000539-199508000-00029
Mouton WG, Bessell JR, Otten KT et al (1999) Pain after laparoscopy. Surg Endosc 13(5):445–448. https://doi.org/10.1007/s004649901011
Lee IO, Kim SH, Kong MH et al (2001) Pain after laparoscopic cholecystectomy: the effect and timing of incisional and intraperitoneal bupivacaine. Can J Anaesth 48(6):545–550. https://doi.org/10.1007/BF03016830
Tam T, Harkins G, Wegrzyniak L et al (2014) Infiltration of bupivacaine local anesthetic to trocar insertion sites after laparoscopy: a randomized, double-blind, stratified, and controlled trial. J Minim Invasive Gynecol 21(6):1015–1021. https://doi.org/10.1016/j.jmig.2014.04.013
Yoshiyama S, Ueshima H, Sakai R et al (2016) A posterior TAP block provides more effective analgesia than a lateral TAP block in patients undergoing laparoscopic gynecologic surgery: a retrospective study. Anesthesiol Res Pract 2016:4598583. https://doi.org/10.1155/2016/4598583
Emile SH, Abdel-Razik MA, Elbahrawy K et al (2019) Impact of ultrasound-guided transversus abdominis plane block on postoperative pain and early outcome after laparoscopic bariatric surgery: a randomized double-blinded controlled trial. Obes Surg 29(5):1534–1541. https://doi.org/10.1007/s11695-019-03720-y
Ruiz-Tovar J, Albrecht E, Macfarlane A, Coluzzi F (2019) The TAP block in obese patients: pros and cons. Minerva Anestesiol 85(9):1024–1031. https://doi.org/10.23736/S0375-9393.19.13545-6
Vial F, Mory S, Guerci P et al (2015) Évaluation de la courbe d'apprentissage du bloc du plan transverse abdominal: étude prospective observationnelle. Evaluating the learning curve for the transversus abdominal plane block: A prospective observational study. Can J Anaesth 62(6):627–33. French. https://doi.org/10.1007/s12630-015-0338-7
Author information
Authors and Affiliations
Contributions
Conceived and designed experiments: SMS, AC. Performed the experiments: SMS, AC. Analysed the data: All authors. Wrote the manuscript: All authors.
Corresponding author
Ethics declarations
Ethics approval
N/A.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Copperthwaite, A., Sahebally, S.M., Raza, Z.M. et al. A meta-analysis of laparoscopic versus ultrasound-guided transversus abdominis plane block in laparoscopic colorectal surgery. Ir J Med Sci 192, 795–803 (2023). https://doi.org/10.1007/s11845-022-03017-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11845-022-03017-7