Abstract
Purpose
The physical frailty phenotype identifies individuals at risk for adverse health outcomes but has rarely been assessed among young adult cancer survivors (YACS). This study describes frailty status among YACS participating in a physical activity (PA) intervention trial.
Methods
YACS were categorized at baseline using the 5-item FRAIL scale: fatigue; weight loss; illness; ambulation; resistance. Chi-square tests compared frailty and non-cancer comorbidities by characteristics. Prevalence rates (PRs) for the independent associations between characteristics, frailty, and comorbidities were estimated using modified Poisson regression models.
Results
Among 280 YACS (82% female; mean (M) age = 33.4 ± 4.8 years, M=3.7 ± 2.4 years post-diagnosis), 11% frail, 17% prefrail; the most frequent criteria were fatigue (41%), resistance (38%), and ambulation (14%). Compared to BMI < 25, higher BMI was associated with increased likelihood of frailty (BMI 25–30, PR: 2.40, 95% CI: 1.38–4.17; BMI > 30, PR: 2.95, 95% CI: 1.71–5.08). Compared to 0, ≥ 30 min/week of moderate-to-vigorous PA was associated with reduced frailty (PR: 0.39, 95% CI: 0.25–0.60). Most YACS (55%) reported ≥ 1 comorbidity, most frequently depression (38%), thyroid condition (19%), and hypertension (10%). Comorbidities were more common for women (59% vs. 37%) and current/former smokers (PR: 1.71, 95% CI: 1.29–2.28).
Conclusion
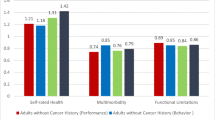
Prevalence of frailty and comorbidities in this sample was similar to other YACS cohorts and older adults without cancer and may be an indicator of accelerated aging and increased risk for poor outcomes.
Implications for Cancer Survivors
Assessment of frailty may help identify YACS at increased risk for adverse health outcomes.
Similar content being viewed by others
References
“Key Statistics for Cancers in Young Adults. ” https://www.cancer.org/cancer/types/cancer-in-young-adults/key-statistics.html (accessed Jun 16, 2023).
Lewis DR, Siembida EJ, Seibel NL, Smith AW, Mariotto AB. Survival outcomes for cancer types with the highest death rates for adolescents and young adults, 1975–2016. ” Cancer Jul. 2021. https://doi.org/10.1002/cncr.33793.
Salchow J, et al. Comprehensive assessments and related interventions to enhance the long-term outcomes of child, adolescent and young adult cancer survivors - presentation of the CARE for CAYA-Program study protocol and associated literature review. ” BMC Cancer. Jan. 2020;20(1):16. https://doi.org/10.1186/s12885-019-6492-5.
Chao C et al. “Chronic comorbidities among survivors of adolescent and young adult cancer.,” J. Clin. Oncol, vol. 38, no. 27, pp. 3161–3174, Sep. 2020, doi: https://doi.org/10.1200/JCO.20.00722.
Morley JE, et al. Frailty consensus: a call to action. J Am Med Dir Assoc. Jun. 2013;14(6):392–7. https://doi.org/10.1016/j.jamda.2013.03.022.
Fried LP et al. “Frailty in older adults: Evidence for a phenotype.,” J. Gerontol. A Biol. Sci. Med. Sci, vol. 56, no. 3, pp. M146-56, Mar. 2001, doi: https://doi.org/10.1093/gerona/56.3.m146.
Hoogendijk EO, Afilalo J, Ensrud KE, Kowal P, Onder G, Fried LP. Frailty: implications for clinical practice and public health. ” Lancet. Oct. 2019;394(10206):1365–75. https://doi.org/10.1016/S0140-6736(19)31786-6.
Bandeen-Roche K et al. “Phenotype of frailty: characterization in the women’s health and aging studies.,” J. Gerontol. A Biol. Sci. Med. Sci, vol. 61, no. 3, pp. 262–266, Mar. 2006, doi: https://doi.org/10.1093/gerona/61.3.262.
Dent E, et al. Physical frailty: ICFSR international clinical practice guidelines for identification and management. ” J Nutr Health Aging. 2019;23(9):771–87. https://doi.org/10.1007/s12603-019-1273-z.
Kim DJ, Massa MS, Potter CM, Clarke R, Bennett DA. Systematic review of the utility of the frailty index and frailty phenotype to predict all-cause mortality in older people. ” Syst Rev. Sep. 2022;11(1):187. https://doi.org/10.1186/s13643-022-02052-w.
Bouillon K, et al. Measures of frailty in population-based studies: an overview. ” BMC Geriatr. Jun. 2013;13:64. https://doi.org/10.1186/1471-2318-13-64.
Abellan G, van Kan Y, Rolland H, Bergman JE, Morley SB, Kritchevsky, Vellas B. “The I.A.N.A Task Force on frailty assessment of older people in clinical practice.,” J. Nutr. Health Aging, vol. 12, no. 1, pp. 29–37, Jan. 2008, doi: https://doi.org/10.1007/BF02982161.
Ness KK et al. “Physiologic frailty as a sign of accelerated aging among adult survivors of childhood cancer: a report from the St Jude Lifetime cohort study.,” J. Clin. Oncol, vol. 31, no. 36, pp. 4496–4503, Dec. 2013, doi: https://doi.org/10.1200/JCO.2013.52.2268.
Ness KK, et al. Premature physiologic aging as a paradigm for understanding increased risk of adverse health across the lifespan of survivors of childhood cancer. J Clin Oncol. Jul. 2018;36:2206–15. https://doi.org/10.1200/JCO.2017.76.7467.
Smitherman AB, Anderson C, Lund JL, Bensen JT, Rosenstein DL, Nichols HB. “Frailty and Comorbidities Among Survivors of Adolescent and Young Adult Cancer: A Cross-Sectional Examination of a Hospital-Based Survivorship Cohort.,” J. Adolesc. Young Adult Oncol, vol. 7, no. 3, pp. 374–383, Jun. 2018, doi: https://doi.org/10.1089/jayao.2017.0103.
Valle CG et al. “Promoting physical activity in young adult cancer survivors using mHealth and adaptive tailored feedback strategies: Design of the Improving Physical Activity after Cancer Treatment (IMPACT) randomized controlled trial.,” Contemp. Clin. Trials, vol. 103, p. 106293, Apr. 2021, doi: https://doi.org/10.1016/j.cct.2021.106293.
Harris PA, et al. The REDCap consortium: building an international community of software platform partners. ” J Biomed Inform. Jul. 2019;95:103208. https://doi.org/10.1016/j.jbi.2019.103208.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. “Research electronic data capture (REDCap): A metadata-driven methodology and workflow process for providing translational research informatics support.,” J. Biomed. Inform, vol. 42, no. 2, pp. 377–381, Apr. 2009, doi: https://doi.org/10.1016/j.jbi.2008.08.010.
Morley JE, Malmstrom TK, Miller DK. “A Simple Frailty Questionnaire (FRAIL) Predicts Outcomes in Middle Aged African Americans.,” J. Nutr. Health Aging, vol. 16, no. 7, pp. 601–608, Jul. 2012, doi: https://doi.org/10.1007/s12603-012-0084-2.
“36-Item Short Form Survey (SF-36) | RAND. ” https://www.rand.org/health-care/surveys_tools/mos/36-item-short-form.html (accessed Dec. 08, 2019).
Hayek S, et al. Prevalence and predictors of frailty in childhood cancer survivors and siblings: a report from the childhood cancer survivor study. ” J Clin Oncol. Jan. 2020;38(3):232–47. https://doi.org/10.1200/JCO.19.01226.
Pranikoff S et al. “Frail young adult cancer survivors experience poor health-related quality of life.,” Cancer, vol. 128, no. 12, pp. 2375–2383, Jun. 2022, doi: https://doi.org/10.1002/cncr.34196.
Wing RR et al. “Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes.,” Diabetes Care, vol. 34, no. 7, pp. 1481–1486, Jul. 2011, doi: https://doi.org/10.2337/dc10-2415.
Smitherman AB et al. “Accelerated aging among childhood, adolescent, and young adult cancer survivors is evidenced by increased expression of p16INK4a and frailty.,” Cancer, vol. 126, no. 22, pp. 4975–4983, Nov. 2020, doi: https://doi.org/10.1002/cncr.33112.
Services US Department of Health and Human., “Centers for Disease Control and Prevention (CDC) behavioral risk factor Surveillance System Survey Questionnaire.,” Atlanta: CDC, 2005.
Nelson DE, et al. The Health Information National Trends Survey (HINTS): development, design, and dissemination. ” J Health Commun. 2004;9(5):443–60. https://doi.org/10.1080/10810730490504233. discussion 81, Oct.
Olfert MD et al. “Self-Reported vs. Measured Height, Weight, and BMI in Young Adults.,” Int. J. Environ. Res. Public Health, vol. 15, no. 10, Oct. 2018, doi: https://doi.org/10.3390/ijerph15102216.
Godin G, Shephard RJ. “A simple method to assess exercise behavior in the community.,” Can. J. Appl. Sport Sci, vol. 10, no. 3, pp. 141–146, Sep. 1985.
“A simultaneous. evaluation of 10 commonly used physical activ… Medicine & Science in Sports & Exercise.” https://journals.lww.com/acsm-msse/Abstract/1993/01000/A_simultaneous_evaluation_of_10_commonly_used.12.aspx (accessed Jun. 16, 2023).
Zou G. A modified poisson regression approach to prospective studies with binary data. ” Am J Epidemiol. Apr. 2004;159(7):702–6. https://doi.org/10.1093/aje/kwh090.
Williams A et al. “Frailty and neurocognitive decline in young adult survivors of childhood cancer: A longitudinal analysis from the St. Jude lifetime cohort.,” JCO, vol. 38, no. 15_suppl, pp. 10555–10555, May 2020, doi: https://doi.org/10.1200/JCO.2020.38.15_suppl.10555.
Ghachem A, et al. Evidence from two cohorts for the frailty syndrome as an emergent state of parallel dysregulation in multiple physiological systems. ” Biogerontology. Feb. 2021;22(1):63–79. https://doi.org/10.1007/s10522-020-09903-w.
Gordon EH, Hubbard RE. “Differences in frailty in older men and women.,” Med. J. Aust, vol. 212, no. 4, pp. 183–188, Mar. 2020, doi: https://doi.org/10.5694/mja2.50466.
Bauer J et al. “Sarcopenia: A time for action. an SCWD position paper.,” J. Cachexia Sarcopenia Muscle, vol. 10, no. 5, pp. 956–961, Oct. 2019, doi: https://doi.org/10.1002/jcsm.12483.
Apóstolo J, et al. Effectiveness of interventions to prevent pre-frailty and frailty progression in older adults: a systematic review. ” JBI Database System Rev Implement Rep. Jan. 2018;16(1):140–232. https://doi.org/10.11124/JBISRIR-2017-003382.
Shin H, Bartlett R, De Gagne JC. Health-Related Quality of Life among Survivors of Cancer in Adolescence: an integrative literature review. ” J Pediatr Nurs. 2019;44:97–106. https://doi.org/10.1016/j.pedn.2018.11.009.
Nolan VG, Krull KR, Gurney JG, Leisenring W, Robison LL, Ness KK. “Predictors of future health-related quality of life in survivors of adolescent cancer.,” Pediatr. Blood Cancer, vol. 61, no. 10, pp. 1891–1894, Oct. 2014, doi: https://doi.org/10.1002/pbc.25037.
Vargo MM. “Outcome Measures and Patient-Reported Metrics in Cancer Rehabilitation.,” Curr. Oncol. Rep, vol. 25, no. 8, pp. 869–882, Aug. 2023, doi: https://doi.org/10.1007/s11912-023-01412-6.
Adams SC, et al. Young Adult Cancer Survivorship: recommendations for patient Follow-up, Exercise Therapy, and Research. ” JNCI Cancer Spectr. Feb. 2021;5(1). https://doi.org/10.1093/jncics/pkaa099.
Rolland Y et al. “Sarcopenia: its assessment, etiology, pathogenesis, consequences and future perspectives.,” J. Nutr. Health Aging, vol. 12, no. 7, pp. 433–450, Sep. 2008, doi: https://doi.org/10.1007/bf02982704.
Woolford SJ, Sohan O, Dennison EM, Cooper C, Patel HP. “Approaches to the diagnosis and prevention of frailty.,” Aging Clin. Exp. Res, vol. 32, no. 9, pp. 1629–1637, Sep. 2020, doi: https://doi.org/10.1007/s40520-020-01559-3.
Ness KK, Wogksch MD. Frailty and aging in cancer survivors. ” Transl Res. Jul. 2020;221:65–82. https://doi.org/10.1016/j.trsl.2020.03.013.
Anderson C, Smitherman AB, Nichols HB. “Conditional relative survival among long-term survivors of adolescent and young adult cancers.,” Cancer, vol. 124, no. 14, pp. 3037–3043, Jul. 2018, doi: https://doi.org/10.1002/cncr.31529.
Janssen SHM, et al. Learning from long-term adolescent and young adult (AYA) cancer survivors regarding their age-specific care needs to improve current AYA care programs. ” Cancer Med. Apr. 2023. https://doi.org/10.1002/cam4.6001.
Acknowledgements
We would like to thank the members of the UNC Weight Research Program for their valuable support, including Brooke Nezami, Karen Hatley, Kristen Polzien, Molly Diamond, and Lindsey Camp.
Funding
Support for Erin Coffman was from the National Institutes of Health, National Cancer Institute (T32CA057726 to the Lineberger Comprehensive Cancer Center Cancer Education and Control Training Program); National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases (T32DK007686 to the UNC Nutrition Training Grant); This work was supported by National Institutes of Health, National Cancer Institute, Grant/Award Numbers: R01CA204965 (to CGV), P30CA016086; National Institute of Diabetes and Digestive and Kidney Diseases, Grant/Award Number: P30DK056350; Lineberger Comprehensive Cancer Center, University of North Carolina at Chapel Hill, University Cancer Research Fund; National Center for Advancing Translational Sciences, Grant/Award Number: UL1TR002489.
Author information
Authors and Affiliations
Contributions
Conceptualization: E.M.C., A.B.S., E.A.W., D.S.W., D.F.T., C.G.V.; Methodology: E.M.C., A.B.S., E.A.W., D.S.W., D.F.T., C.G.V.; Formal analysis and investigation: E.M.C; Writing - original draft preparation: E.M.C; Writing - review and editing: E.M.C., A.B.S., E.A.W., D.S.W., C.G.V.; Funding acquisition: E.M.C., D.F.T., C.G.V.
Corresponding author
Ethics declarations
Conflict of interest disclosures
None.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Coffman, E.M., Smitherman, A.B., Willis, E.A. et al. Frailty and comorbidities among young adult cancer survivors enrolled in an mHealth physical activity intervention trial. J Cancer Surviv (2023). https://doi.org/10.1007/s11764-023-01448-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11764-023-01448-4