Abstract
Purpose
Many workers had flexible work arrangements during the COVID-19 pandemic. This study aimed to identify the association between flextime and remote working and job resignation among Japanese young adult cancer survivors after diagnosis.
Methods
This cross-sectional observational study was conducted using an online survey with 401 Japanese young adult cancer survivors diagnosed with adult-onset cancer and aged 20–39 years at the time of the survey in January 2022. A multivariable Cox regression analysis was performed to analyze the impact of flextime and remote working on job resignation.
Results
In the sample, 264 participants (65.8%) were female, and 185 (46.1%) had been diagnosed with cancer between 1 and 5 years ago. After adjusting for potential confounders, the multivariable Cox regression analysis revealed that young adult cancer survivors using remote working only (HR 0.44, 95% CI 0.21–0.96, p = 0.04) and both flextime and remote working (HR 0.37, 95% CI 0.21–0.64, p < 0.01) experienced a lower risk of job resignation after cancer diagnosis compared to those who did not use flextime and remote working.
Conclusions
Young adult cancer survivors who used remote working only or remote working combined with flextime could reduce their risk of job resignation after a cancer diagnosis.
Implications for Cancer Survivors
This study showed that having the option of remote working can be important for young adult cancer survivors’ continuing employment. Furthermore, social welfare systems need to promote a workplace culture and climate that allows remote working.

Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Feuerstein M, Todd BL, Moskowitz MC, Bruns GL, Stoler MR, Nassif T, et al. Work in cancer survivors: a model for practice and research. J Cancer Surviv. 2010;4:415–37. https://doi.org/10.1007/s11764-010-0154-6.
van der Meer DJ, Karim-Kos HE, van der Mark M, Aben KKH, Bijlsma RM, Rijneveld AW, et al. Incidence, survival, and mortality trends of cancers diagnosed in adolescents and young adults (15–39 years): a population-based study in the Netherlands 1990–2016. Cancers. 2020;12:3421. https://doi.org/10.3390/cancers12113421.
Moke DJ, Tsai K, Hamilton AS, Hwang A, Liu L, Freyer DR, et al. Emerging cancer survival trends, disparities, and priorities in adolescents and young adults: a California cancer registry-based study. JNCI Cancer Spectr. 2019;3:pkz031. https://doi.org/10.1093/jncics/pkz031.
Hydeman JA, Uwazurike OC, Adeyemi EI, Beaupin LK. Survivorship needs of adolescent and young adult cancer survivors: a concept map** analysis. J Cancer Surviv. 2019;13:34–42. https://doi.org/10.1007/s11764-018-0725-5.
Blinder VS, Gany FM. Impact of cancer on employment. J Clin Oncol. 2020;38:302–9. https://doi.org/10.1200/JCO.19.01856.
Moran JR, Short PF, Hollenbeak CS. Long-term employment effects of surviving cancer. J Health Econ. 2011;30:505–14. https://doi.org/10.1016/j.jhealeco.2011.02.001.
Bradley CJ, Brown KL, Haan M, Glasgow RE, Newman LS, Rabin B, et al. Cancer survivorship and employment: intersection of oral agents, changing workforce dynamics, and employers’ perspectives. J Natl Cancer Inst. 2018;110:1292–9. https://doi.org/10.1093/jnci/djy172.
Torp S, Paraponaris A, Van Hoof E, Lindbohm ML, Tamminga SJ, Alleaume C, et al. Work-related outcomes in self-employed cancer survivors: a European multi-country study. J Occup Rehabil. 2019;29:361–74. https://doi.org/10.1007/s10926-018-9792-8.
Désiron HA, Crutzen R, Godderis L, Van Hoof E, de Rijk A. Bridging health care and the workplace: formulation of a return-to-work intervention for breast cancer patients using an intervention map** approach. J Occup Rehabil. 2016;26:350–65. https://doi.org/10.1007/s10926-015-9620-3.
de Boer AG, Verbeek JH, Spelten ER, Uitterhoeve AL, Ansink AC, de Reijke TM, et al. Work ability and return-to-work in cancer patients. Br J Cancer. 2008;98:1342–7. https://doi.org/10.1038/sj.bjc.6604302.
Stone DS, Ganz PA, Pavlish C, Robbins WA. Young adult cancer survivors and work: a systematic review. J Cancer Surviv. 2017;11:765–81. https://doi.org/10.1007/s11764-017-0614-3.
Rabin C. Cancer-related self-disclosure in the workplace/school by adolescent and young adult cancer survivors. J Adolesc Young Adult Oncol. 2020;9:528–33. https://doi.org/10.1089/jayao.2019.0159.
de Boer AG, Torp S, Popa A, Horsboel T, Zadnik V, Rottenberg Y, et al. Long-term work retention after treatment for cancer: a systematic review and meta-analysis. J Cancer Surviv. 2020;14:135–50. https://doi.org/10.1007/s11764-020-00862-2.
Hamood R, Hamood H, Merhasin I, Keinan-Boker L. Work transitions in breast cancer survivors and effects on quality of life. J Occup Rehabil. 2019;29:336–49. https://doi.org/10.1007/s10926-018-9789-3.
Alleaume C, Bendiane MK, Bouhnik AD, Rey D, Cortaredona S, Seror V, et al. Chronic neuropathic pain negatively associated with employment retention of cancer survivors: evidence from a national French survey. J Cancer Surviv. 2018;12:115–26. https://doi.org/10.1007/s11764-017-0650-z.
Landeiro LCG, Gagliato DM, Fêde AB, Fraile NM, Lopez RM, da Fonseca LG, et al. Return to work after breast cancer diagnosis: an observational prospective study in Brazil. Cancer. 2018;124:4700–10. https://doi.org/10.1002/cncr.31735.
Jeon SH. The long-term effects of cancer on employment and earnings. Health Econ. 2017;26:671–84. https://doi.org/10.1002/hec.3342.
Tison A, Sagaon-Teyssier L, Sansonetti C, Blatier JF, Paraponaris A, VICAN 2 group. Transitions in the labor market after cancer: a comparison of self-employed workers and salaried staff. Support Care Cancer. 2016;24:4879–86. https://doi.org/10.1007/s00520-016-3343-7.
Jagsi R, Hawley ST, Abrahamse P, Li Y, Janz NK, Griggs JJ, et al. Impact of adjuvant chemotherapy on long-term employment of survivors of early-stage breast cancer. Cancer. 2014;120:1854–62. https://doi.org/10.1002/cncr.28607.
Luker K, Campbell M, Amir Z, Davies L. A UK survey of the impact of cancer on employment. Occup Med (Lond). 2013;63:494–500. https://doi.org/10.1093/occmed/kqt104.
Torp S, Gudbergsson SB, Dahl AA, Fosså SD, Fløtten T. Social support at work and work changes among cancer survivors in Norway. Scand J Public Health. 2011;39(6 Suppl):33–42. https://doi.org/10.1177/1403494810395827.
Blinder V, Patil S, Eberle C, Griggs J, Maly RC. Early predictors of not returning to work in low-income breast cancer survivors: a 5-year longitudinal study. Breast Cancer Res Treat. 2013;140:407–16. https://doi.org/10.1007/s10549-013-2625-8.
Roelen CA, Koopmans PC, Schellart AJ, van der Beek AJ. Resuming work after cancer: a prospective study of occupational register data. J Occup Rehabil. 2011;21:431–40. https://doi.org/10.1007/s10926-010-9274-0.
Fiva JH, Haegeland T, Rønning M. Health status after cancer: does it matter which hospital you belong to? BMC Health Serv Res. 2010;10:204. https://doi.org/10.1186/1472-6963-10-204.
Lindbohm ML, Kuosma E, Taskila T, Hietanen P, Carlsen K, Gudbergsson S, et al. Cancer as the cause of changes in work situation (a NOCWO study). Psychooncology. 2011;20:805–12. https://doi.org/10.1002/pon.1797.
Mitsui K, Endo M, Imai Y, Ueda Y, Ogawa H, Muto G, et al. Predictors of resignation and sick leave after cancer diagnosis among Japanese breast cancer survivors: a cross-sectional study. BMC Public Health. 2021;21:138. https://doi.org/10.1186/s12889-021-10168-2.
Endo M, Muto G, Imai Y, Mitsui K, Nishimura K, Hayashi K. Predictors of post-cancer diagnosis resignation among Japanese cancer survivors. J Cancer Surviv. 2020;14:106–13. https://doi.org/10.1007/s11764-019-00827-0.
Cambridge University Press. Flextime (Cambridge Dictionary). https://dictionary.cambridge.org/us/dictionary/english/flextime. Accessed May 23, 2022
Cambridge University Press. Remote working (Cambridge Dictionary). https://dictionary.cambridge.org/us/dictionary/english/remote-working. Accessed May 23, 2022
Barrero JM, Bloom N, Davis SJ Why working from home will stick. University of Chicago, Becker Friedman Institute for Economics Working Paper. 2021 2020–174. https://doi.org/10.2139/ssrn.3741644
Papanikolaou D, Schmidt LDW. Working remotely and the supply-side impact of COVID-19. Rev Asset Pricing Stud. 2022;12:53–111. https://doi.org/10.1093/rapstu/raab026.
Nuwer R. No workplace like home. Sci Am Mind. 2016;27:38–43. https://doi.org/10.1038/scientificamericanmind0916-38.
Bloom N, Liang J, Roberts J, Ying ZJ. Does working from home work? Evidence from a Chinese experiment. Q J Econ. 2015;130:165–218. https://doi.org/10.1093/qje/qju032.
Kollerup A, Ladenburg J, Heinesen E, Kolodziejczyk C. The importance of workplace accommodation for cancer survivors – the role of flexible work schedules and psychological help in returning to work. Econ Hum Biol. 2021;43:101057. https://doi.org/10.1016/j.ehb.2021.101057.
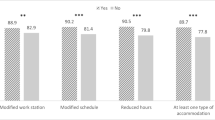
Alleaume C, Paraponaris A, Bendiane MK, Peretti-Watel P, Bouhnik AD. The positive effect of workplace accommodations on the continued employment of cancer survivors five years after diagnosis. Support Care Cancer. 2020;28:4435–43. https://doi.org/10.1007/s00520-019-05189-y.
Mujahid MS, Janz NK, Hawley ST, Griggs JJ, Hamilton AS, Katz SJ. The impact of sociodemographic, treatment, and work support on missed work after breast cancer diagnosis. Breast Cancer Res Treat. 2010;119:213–20. https://doi.org/10.1007/s10549-009-0389-y.
Hallgren E, Ayers BL, Moore R, Purvis RS, McElfish PA, Maraboyina S, et al. Facilitators and barriers to employment for rural women cancer survivors. J Cancer Surviv. 2022. https://doi.org/10.1007/s11764-022-01179-y.
Ministry of Health, Labour and Welfare of Japan. Labor Contract Act. 2007. https://www.japaneselawtranslation.go.jp/ja/laws/view/3744. Accessed Apr 18 2023.
Takahashi M, Tsuchiya M, Horio Y, Funazaki H, Aogi K, Miyauchi K, et al. Job resignation after cancer diagnosis among working survivors in Japan: timing, reasons and change of information needs over time. Jpn J Clin Oncol. 2018;48:43–51. https://doi.org/10.1093/jjco/hyx143.
Fujisawa D, Umezawa S, Fujimori M, Miyashita M. Prevalence and associated factors of perceived cancer-related stigma in Japanese cancer survivors. Jpn J Clin Oncol. 2020;50:1325–9. https://doi.org/10.1093/jjco/hyaa135.
Ministry of Health, Labour and Welfare of Japan. Jirei kara manabu tiryou to shigoto no ryoritsu no tame no syokuba niokeru hokenkatsudo no hintosyu [Collection of tips for occupational health activities to support balancing treatment and work on the basis of case studies]. 2014. https://www.mhlw.go.jp/new-info/kobetu/roudou/gyousei/anzen/dl/140328-01.pdf. Accessed Apr 18, 2023.
Japan Institute for Labour Policy and Training. Byoki no tiryo to shigoto no ryoritsu ni kansuru jittaichosa [Survey on balancing treatment and working life in individuals with chronic/intractable illness]. 2018. https://www.jil.go.jp/institute/research/2018/documents/180.pdf. 2018. Accessed Jun 10, 2021.
Schaufeli WB. Applying the job demands-resources model: a ‘how to’ guide to measuring and tackling work engagement and burnout. Organ Dyn. 2017;2:120–32.
Kruse D, Park SR, van der Meulen RY, Schur L. Disability and remote work during the pandemic with implications for cancer survivors. J Cancer Surviv. 2022;16:183–99. https://doi.org/10.1007/s11764-021-01146-z.
Dey M, Frazis H, Piccone DSJ, Loewenstein MA. Teleworking and lost work during the pandemic: new evidence from the CPS. https://ssrn.com/abstract=3807195. Accessed Sep 6, 2022
Ministry of Health, Labour, and Welfare, Japan. Basic plan to promote cancer control programs. https://www.mhlw.go.jp/english/wp/wp-hw2/part2/p3_0026.pdf. Accessed Aug 11, 2022
Acknowledgements
The authors would like to extend special thanks to the young adult cancer survivors who participated in the study.
Funding
This study was supported by grants from the Japan Society for the Promotion of Science (JSPS KAKENHI Grant-in-Aid for Young Scientists, grant number 19K19639) to Takafumi Soejima. The funders had no role in the study design, data collection and analysis, decision of publication, or manuscript preparation.
Author information
Authors and Affiliations
Contributions
All authors contributed to the conception and design of the study. Data collection was performed by Takafumi Soejima. All authors contributed to the data analysis and interpretation, drafted the manuscript, and critically reviewed it. All authors approved the final version of the manuscript and agreed to be accountable for all aspects of the work and ensure that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki and the Ethical Guidelines for Medical and Biological Research Involving Human Subjects established by the Ministry of Health, Labor, and Welfare of Japan. Approval was granted by the Ethics Committee of the Graduate School of Health Sciences, Kobe University (August 31st, 2021/No. 1029).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Soejima, T., Tokita, M. & Kitao, M. Impact of flexible work arrangements on job resignation after cancer diagnosis among Japanese young adult cancer survivors. J Cancer Surviv (2023). https://doi.org/10.1007/s11764-023-01421-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11764-023-01421-1