Abstract
Purpose
Cancer survivors face higher rates of unemployment compared with individuals without a history of cancer. Compared to other cancer types, head and neck cancer (HNC) survivors face unique disease and treatment-specific issues that may limit return to work (RTW). This review aimed to determine employment outcomes of HNC survivors post-treatment and identify factors associated with RTW.
Methods
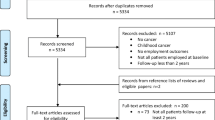
A systematic search was conducted in MEDLINE, CINAHL and PsycINFO in December 2021. Inclusion criteria included adults (≥ 18 years); completed treatment for HNC; data available on RTW post-treatment. Both quantitative and qualitative studies were considered. Studies were critically appraised and data synthesised narratively.
Results
Twenty-nine publications were included: 22 quantitative, four qualitative and three mixed methods. The proportion of HNC survivors who RTW ranged from 32 to 90%, with participants taking 3.6–11 months to RTW. Working in a professional role and having a supportive work environment were positively associated with RTW.
Conclusions
The proportion of HNC survivors who RTW varies significantly which may be due to the heterogeneity between the studies including difference in clinical characteristics of the participants and/or sample size. Future studies that are longitudinal, adequately powered and measure a range of clinical and demographic variables are needed to better understand the RTW experience and assist development of effective RTW strategies.
Implications for Cancer Survivors
This review suggests potential areas for intervention, including enhanced symptom management and engaging with employers to foster supportive work environments to support RTW of HNC survivors.

Similar content being viewed by others
References
Cancer Council Australia. Australians living with and beyond cancer in 2040. Sydney: Cancer Council Australia; 31 January 2018.
American Cancer Society. Cancer Facts & Figures 2021. Atlanta: American Cancer Society; 2021.
de Boer AG, Taskila T, Tamminga SJ, Frings-Dresen MH, Feuerstein M, Verbeek JH. Interventions to enhance return-to-work for cancer patients. Cochrane Database Syst Rev. 2011. https://doi.org/10.1002/14651858.CD007569.pub2.
Jemal A, Torre L, Soerjomatram I, Bray F. The Cancer Atlas. 3rd ed. Georgia: American Cancer Society, Inc.; 2019.
Amir Z, Neary D, Luker K. Cancer survivors’ views of work 3 years post diagnosis: a UK perspective. Eur J Oncol Nurs. 2008. https://doi.org/10.1016/j.ejon.2008.01.006.
Grunfeld EA, Cooper AF. A longitudinal qualitative study of the experience of working following treatment for gynaecological cancer. Psychooncology. 2012. https://doi.org/10.1002/pon.1874.
Kennedy F, Haslam C, Munir F, Pryce J. Returning to work following cancer: a qualitative exploratory study into the experience of returning to work following cancer. Eur J Cancer Care (Engl). 2007. https://doi.org/10.1111/j.1365-2354.2007.00729.x.
McKay G, Knott V, Delfabbro P. Return to work and cancer: the Australian experience. J Occup Rehabil. 2013. https://doi.org/10.1007/s10926-012-9386-9.
Johnsson A, Fornander T, Rutqvist LE, Olsson M. Factors influencing return to work: a narrative study of women treated for breast cancer. Eur J Cancer Care (Engl). 2010. https://doi.org/10.1111/j.1365-2354.2008.01043.x.
de Boer AG, Taskila T, Ojajarvi A, van Dijk FJ, Verbeek JH. Cancer survivors and unemployment: a meta-analysis and meta-regression. JAMA. 2009. https://doi.org/10.1001/jama.2009.187.
Ross L, Petersen MA, Johnsen AT, Lundstroem LH, Carlsen K, Groenvold M. Factors associated with Danish cancer patients’ return to work A report from the population-based study ‘The Cancer Patient’s World.’ Cancer Epidemiol. 2012. https://doi.org/10.1016/j.canep.2011.06.001.
Syse A, Tretli S, Kravdal O. Cancer’s impact on employment and earnings–a population-based study from Norway. J Cancer Surviv. 2008. https://doi.org/10.1007/s11764-008-0053-2.
Short PF, Vasey JJ, Tunceli K. Employment pathways in a large cohort of adult cancer survivors. Cancer. 2005. https://doi.org/10.1002/cncr.20912.
Schultz PN, Beck ML, Stava C, Sellin RV. Cancer survivors. Work Relat Issues Aaohn J. 2002;5:220–6.
Australian Institute of Health and Welfare. Cancer in Australia. In: Cancer series no. 101. Australian Institute of Health and Welfare. 2017. https://www.aihw.gov.au/getmedia/3da1f3c2-30f0-4475-8aed-1f19f8e16d48/20066-cancer-2017.pdf.aspx?inline=true. Accessed 2 Jun 2018
Cancer Research UK. Ten most common cancers in males. In: Cancer incidence for common cancers. 2018. https://www.cancerresearchuk.org/health-professional/cancer-statistics/incidence/common-cancers-compared. Accessed 15 Jul 2018.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018. https://doi.org/10.3322/caac.21442.
Hong A, Lee CS, Jones D, Veillard AS, Zhang M, Zhang X, Smee R, Corry J, Porceddu S, Milross C, Elliott M, Clark J, Rose B. Rising prevalence of human papillomavirus-related oropharyngeal cancer in Australia over the last 2 decades. Head Neck. 2016. https://doi.org/10.1002/hed.23942.
Vidal L, Gillison ML. Human papillomavirus in HNSCC: recognition of a distinct disease type. Hematol Oncol Clin North Am. 2008. https://doi.org/10.1016/j.hoc.2008.08.006.
Critical Appraisal Skills Program. CASP Qualitative Research Checklist 2017. http://docs.wixstatic.com/ugd/dded87_25658615020e427da194a325e7773d42.pdf. Accessed 26 Sep 2017.
Downes MJ, Brennan ML, Williams HC, Dean RS. Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS). BMJ Open. 2016. https://doi.org/10.1136/bmjopen-2016-011458.
Hong QN, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M, Dagenais P, Gagnon M-P, Griffiths F, Nicolau B, O’Cathain A, Rousseau M-C, Vedel I. Mixed Methods Appraisal Tool (MMAT). McGill University. 2018. http://mixedmethodsappraisaltoolpublic.pbworks.com/w/file/fetch/127916259/MMAT_2018_criteria-manual_2018-08-01_ENG.pdf. Accessed 20 Nov 2018.
Dewa CS, Trojanowski L, Tamminga SJ, Ringash J, McQuestion M, Hoch JS. Work-related experiences of head and neck cancer survivors: an exploratory and descriptive qualitative study. Disabil Rehabil. 2018. https://doi.org/10.1080/09638288.2017.1291764.
Moore KA, Ford PJ, Farah CS. “I have quality of life…but…” exploring support needs important to quality of life in head and neck cancer. Eur J Oncol Nurs. 2014. https://doi.org/10.1016/j.ejon.2013.10.010.
Semple CJ, Dunwoody L, George Kernohan W, McCaughan E, Sullivan K. Changes and challenges to patients’ lifestyle patterns following treatment for head and neck cancer. J Adv Nurs. 2008. https://doi.org/10.1111/j.1365-2648.2008.04698.x.
Semple CJ, Rutherford H, Killough S, Moore C, McKenna G. Long-term impact of living with an obturator following a maxillectomy: a qualitative study. J Dent. 2019. https://doi.org/10.1016/j.jdent.2019.103212.
Spalthoff S, Zimmerer R, Jehn P, Gellrich NC, Handschel J, Kruskemper G. Neck dissection’s nurden on the patient: Functional and psychosocial aspects in 1,652 patients with oral squamous cell carcinomas. J Oral Maxillofac Surg. 2017. https://doi.org/10.1016/j.joms.2016.09.037.
Agarwal J, Krishnatry R, Chaturvedi P, Ghosh-Laskar S, Gupta T, Budrukkar A, Murthy V, Deodhar J, Nair D, Nair S, Dikshit R, D’Cruz AK. Survey of return to work of head and neck cancer survivors: a report from a tertiary cancer center in India. Head Neck. 2017. https://doi.org/10.1002/hed.24703.
Lee MS, Nelson AM, Thompson LM, Donovan KA. Supportive care needs of oral cancer survivors: prevalence and correlates. Oral Oncol. 2016. https://doi.org/10.1016/j.oraloncology.2015.11.007.
Wells M, Swartzman S, Lang H, Cunningham M, Taylor L, Thomson J, Philp J, McCowan C. Predictors of quality of life in head and neck cancer survivors up to 5 years after end of treatment: a cross-sectional survey. Support Care Cancer. 2016. https://doi.org/10.1007/s00520-015-3045-6.
Wells M, Cunningham M, Lang H, Swartzman S, Philp J, Taylor L, Thomson J. Distress, concerns and unmet needs in survivors of head and neck cancer: a cross-sectional survey. Eur J Cancer Care (Engl). 2015. https://doi.org/10.1111/ecc.12370.
Baxi SS, Salz T, **ao H, Atoria CL, Ho A, Smith-Marrone S, Sherman EJ, Lee NY, Elkin EB, Pfister DG. Employment and return to work following chemoradiation in patient with HPV-related oropharyngeal cancer. Cancers Head Neck. 2016. https://doi.org/10.1186/s41199-016-0002-0.
Gallagher KK, Sacco AG, Lee JS, Taylor R, Chanowski EJ, Bradford CR, Prince ME, Moyer JS, Wolf GT, Worden FP, Eisbruch A, Chepeha DB. Association between multimodality neck treatment and work and leisure impairment: a disease-specific measure to assess both impairment and rehabilitation after neck dissection. JAMA Otolaryngol Head Neck Surg. 2015. https://doi.org/10.1001/jamaoto.2015.2049.
Koch R, Wittekindt C, Altendorf-Hofmann A, Singer S, Guntinas-Lichius O. Employment pathways and work-related issues in head and neck cancer survivors. Head Neck. 2015. https://doi.org/10.1002/hed.23640.
Pierre CS, Dassonville O, Chamorey E, Poissonnet G, Ettaiche M, Santini J, Peyrade F, Benezery K, Sudaka A, Bozec A. Long-term quality of life and its predictive factors after oncologic surgery and microvascular reconstruction in patients with oral or oropharyngeal cancer. Eur Arch Otorhinolaryngol. 2014. https://doi.org/10.1007/s00405-013-2592-z.
Cooper AF, Hankins M, Rixon L, Eaton E, Grunfeld EA. Distinct work-related, clinical and psychological factors predict return to work following treatment in four different cancer types. Psychooncology. 2013. https://doi.org/10.1002/pon.3049.
Lee MT, Gibson S, Hilari K. Gender differences in health-related quality of life following total laryngectomy. Int J Lang Commun Disord. 2010. https://doi.org/10.3109/13682820902994218.
Verdonck-de Leeuw IM, van Bleek WJ, Leemans CR, de Bree R. Employment and return to work in head and neck cancer survivors. Oral Oncol. 2010. https://doi.org/10.1016/j.oraloncology.2009.11.001.
Liu HE. Changes of satisfaction with appearance and working status for head and neck tumour patients. J Clin Nurs. 2008. https://doi.org/10.1111/j.1365-2702.2008.02291.x.
Vartanian JG, Carvalho AL, Toyota J, Kowalski IS, Kowalski LP. Socioeconomic effects of and risk factors for disability in long-term survivors of head and neck cancer. Arch Otolaryngol Head Neck Surg. 2006. https://doi.org/10.1001/archotol.132.1.32.
Ramirez MJ, Ferriol EE, Domenech FG, Llatas MC, Suarez-Varela MM, Martinez RL. Psychosocial adjustment in patients surgically treated for laryngeal cancer. Otolaryngol Head Neck Surg. 2003. https://doi.org/10.1016/S0194-59980300478-9.
Terrell JE, Nanavati K, Esclamado RM, Bradford CR, Wolf GT. Health impact of head and neck cancer. Otolaryngol Head Neck Surg. 1999. https://doi.org/10.1016/S0194-5998(99)70326-8.
Handschel J, Gellrich NC, Bremerich A, Kruskemper G. Return to work and quality of life after therapy and rehabilitation in oral cancer. In Vivo. 2013;3:401–7.
Buckwalter AE, Karnell LH, Smith RB, Christensen AJ, Funk GF. Patient-reported factors associated with discontinuing employment following head and neck cancer treatment. Arch Otolaryngol Head Neck Surg. 2007. https://doi.org/10.1001/archotol.133.5.464.
So N, McDowell LJ, Lu L, Xu W, Rock K, Waldron J, Bernstein LJ, Chan HB, Huang SH, Giuliani M, Hope A, O’Sullivan B, Bratman SV, Cho J, Kim J, Jang R, Bayley A, Ringash J. The prevalence and determinants of return to work in nasopharyngeal carcinoma survivors. Int J Radiat Oncol Biol Phys. 2019. https://doi.org/10.1016/j.ijrobp.2019.09.008.
Chen SC, Huang BS, Hung TM, Lin CY, Chang YL. Impact of physical and psychosocial dysfunction on return to work in survivors of oral cavity cancer. Psychooncology. 2019. https://doi.org/10.1002/pon.5173.
Chen YJ, Lai YH, Lee YH, Tsai KY, Chen MK, Hsieh MY. Impact of illness perception, mental adjustment, and sociodemographic characteristics on return to work in patients with head and neck cancer. Support Care Cancer. 2021. https://doi.org/10.1007/s00520-020-05640-5.
Granstrom B, Tiblom Ehrsson Y, Holmberg E, Hammerlid E, Beran M, Tano K, Laurell G, Swedish H, Neck CR. Return to work after oropharyngeal cancer treatment-highlighting a growing working-age population. Head Neck. 2020. https://doi.org/10.1002/hed.26123.
Isaksson J, Wilms T, Laurell G, Fransson P, Ehrsson YT. Meaning of work and the process of returning after head and neck cancer. Support Care Cancer. 2016. https://doi.org/10.1007/s00520-015-2769-7.
Mertl J, Žáčková E. Řepová B 2018 Quality of life of patients after total laryngectomy the struggle against stigmatization and social exclusion using speech synthesis. Disabil Rehabil Assist Tech. 2017. https://doi.org/10.1080/174831071319428.
Zecena Morales C, McDowell L, Lisy K, Piper A, Jefford M. Return to work in survivors of human papillomavirus-associated oropharyngeal cancer: an Australian experience. Int J Radiat Oncol Biol Phys. 2020. https://doi.org/10.1016/j.ijrobp.2019.09.001.
World Bank. World Bank Open Data In: World development indicators. The World Bank Group. 2018. https://data.worldbank.org/. Accessed 14 Apr 2018.
Check DK, Hutcheson KA, Poisson LM, Pocobelli G, Sakoda LC, Zaveri J, Chang SS, Chubak J. Factors associated with employment discontinuation among older and working age survivors of oropharyngeal cancer. Head Neck. 2019. https://doi.org/10.1002/hed.25943.
Petersson LM, Wennman-Larsen A, Nilsson M, Olsson M, Alexanderson K. Work situation and sickness absence in the initial period after breast cancer surgery. Acta Oncol. 2011. https://doi.org/10.3109/0284186X.2010.533191.
Fantoni SQ, Peugniez C, Duhamel A, Skrzypczak J, Frimat P, Leroyer A. Factors related to return to work by women with breast cancer in northern France. J Occup Rehabil. 2010. https://doi.org/10.1007/s10926-009-9215-y.
Lee MK, Kang HS, Lee KS, Lee ES. Three-year prospective cohort study of factors associated with return to work after breast cancer diagnosis. J Occup Rehabil. 2017. https://doi.org/10.1007/s10926-016-9685-7.
Vooijs M, Leensen MC, Hoving JL, Daams JG, Wind H, Frings-Dresen MH. Disease-generic factors of work participation of workers with a chronic disease: a systematic review. Int Arch Occup Environ Health. 2015. https://doi.org/10.1007/s00420-015-1025-2.
Kiasuwa Mbengi RL, Nicolaie AM, Goetghebeur E, Otter R, Mortelmans K, Missinnne S, Arbyn M, Bouland C, de Brouwer C. Assessing factors associated with long-term work disability after cancer in Belgium: a population-based cohort study using competing risks analysis with a 7-year follow-up. BMJ Open. 2018. https://doi.org/10.1136/bmjopen-2016-014094.
Kiasuwa Mbengi R, Otter R, Mortelmans K, Arbyn M, Van Oyen H, Bouland C, de Brouwer C. Barriers and opportunities for return-to-work of cancer survivors: time for action–rapid review and expert consultation. Syst Rev. 2016. https://doi.org/10.1186/s13643-016-0210-z.
Ervasti J, Kivimaki M, Dray-Spira R, Head J, Goldberg M, Pentti J, Jokela M, Vahtera J, Zins M, Virtanen M. Socioeconomic gradient in work disability in diabetes: evidence from three occupational cohorts. J Epidemiol Community Health. 2016. https://doi.org/10.1136/jech-2015-205943.
Piha K, Laaksonen M, Martikainen P, Rahkonen O, Lahelma E. Interrelationships between education, occupational class, income and sickness absence. Eur J Public Health. 2010. https://doi.org/10.1093/eurpub/ckp162.
Blinder VS, Patil S, Thind A, Diamant A, Hudis CA, Basch E, Maly RC. Return to work in low-income Latina and non-Latina white breast cancer survivors: a 3-year longitudinal study. Cancer. 2012. https://doi.org/10.1002/cncr.26478.
Ahn E, Cho J, Shin DW, Park BW, Ahn SH, Noh DY, Nam SJ, Lee ES, Yun YH. Impact of breast cancer diagnosis and treatment on work-related life and factors affecting them. Breast Cancer Res Treat. 2009. https://doi.org/10.1007/s10549-008-0209-9.
Carlsen K, Jensen AJ, Rugulies R, Christensen J, Bidstrup PE, Johansen C, Huitfeldt Madsen IE, Dalton SO. Self-reported work ability in long-term breast cancer survivors A population-based questionnaire study in Denmark. Acta Oncol. 2013. https://doi.org/10.3109/0284186X.2012.744877.
van Egmond MP, Duijts SFA, Loyen A, Vermeulen SJ, van der Beek AJ, Anema JR. Barriers and facilitators for return to work in cancer survivors with job loss experience: a focus group study. Eur J Cancer Care (Engl). 2017. https://doi.org/10.1111/ecc.12420.
Cullen KL, Irvin E, Collie A, Clay F, Gensby U, Jennings PA, Hogg-Johnson S, Kristman V, Laberge M, McKenzie D, Newnam S, Palagyi A, Ruseckaite R, Sheppard DM, Shourie S, Steenstra I, Van Eerd D, Amick BC 3rd. Effectiveness of workplace interventions in return-to-work for musculoskeletal, pain-related and mental health conditions: an update of the evidence and messages for practitioners. J Occup Rehabil. 2018. https://doi.org/10.1007/s10926-016-9690-x.
Odeen M, Magnussen LH, Maeland S, Larun L, Eriksen HR, Tveito TH. Systematic review of active workplace interventions to reduce sickness absence. Occup Med (Lond). 2013. https://doi.org/10.1093/occmed/kqs198.
Ostlund U, Kidd L, Wengstrom Y, Rowa-Dewar N. Combining qualitative and quantitative research within mixed method research designs: a methodological review. Int J Nurs Stud. 2011. https://doi.org/10.1016/j.ijnurstu.2010.10.005.
Silver JK, Baima J, Mayer RS. Impairment-driven cancer rehabilitation: an essential component of quality care and survivorship. CA Cancer J Clin. 2013. https://doi.org/10.3322/caac.21186.
Mewes JC, Steuten LM, Ijzerman MJ, van Harten WH. Effectiveness of multidimensional cancer survivor rehabilitation and cost-effectiveness of cancer rehabilitation in general: a systematic review. Oncologist. 2012. https://doi.org/10.1634/theoncologist.2012-0151.
Duijts SF, Faber MM, Oldenburg HS, van Beurden M, Aaronson NK. Effectiveness of behavioral techniques and physical exercise on psychosocial functioning and health-related quality of life in breast cancer patients and survivors–a meta-analysis. Psychooncology. 2011. https://doi.org/10.1002/pon.1728.
de Boer AG, Taskila TK, Tamminga SJ, Feuerstein M, Frings-Dresen MH, Verbeek JH. Interventions to enhance return-to-work for cancer patients. Cochrane Database Syst Rev. 2015. https://doi.org/10.1002/14651858.CD007569.pub3.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Claudia Zecena Morales. The first draft of the manuscript was written by Claudia Zecena Morales and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zecena Morales, C., Lisy, K., McDowell, L. et al. Return to work in head and neck cancer survivors: a systematic review. J Cancer Surviv 17, 468–483 (2023). https://doi.org/10.1007/s11764-022-01298-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-022-01298-6