Abstract
Weekend discharges occur less frequently than discharges on weekdays, contributing to hospital congestion. Artificial intelligence algorithms have previously been derived to predict which patients are nearing discharge based upon ward round notes. In this implementation study, such an artificial intelligence algorithm was coupled with a multidisciplinary discharge facilitation team on weekend shifts. This approach was implemented in a tertiary hospital, and then compared to a historical cohort from the same time the previous year. There were 3990 patients included in the study. There was a significant increase in the proportion of inpatients who received weekend discharges in the intervention group compared to the control group (median 18%, IQR 18–20%, vs median 14%, IQR 12% to 17%, P = 0.031). There was a corresponding higher absolute number of weekend discharges during the intervention period compared to the control period (P = 0.025). The studied intervention was associated with an increase in weekend discharges and economic analyses support this approach as being cost-effective. Further studies are required to examine the generalizability of this approach to other centers.
Similar content being viewed by others
References
Australian Medical Association (2021) Public hospitals: cycle of crisis
Richardson DB, Mountain D (2009) Myths versus facts in emergency department overcrowding and hospital access block. Med J Aust 190(7):369–374. https://doi.org/10.5694/j.1326-5377.2009.tb02451.x
Cadel L, Guilcher SJT, Kokorelias KM, Sutherland J, Glasby J, Kiran T, Kuluski K (2021) Initiatives for improving delayed discharge from a hospital setting: a sco** review. BMJ Open 11(2):e044291. https://doi.org/10.1136/bmjopen-2020-044291
Goncalves-Bradley DC, Lannin NA, Clemson LM, Cameron ID, Shepperd S (2016) Discharge planning from hospital. Cochrane Database Syst Rev 1:CD000313. https://doi.org/10.1002/14651858.CD000313.pub5
Lin C-J, Cheng S-J, Shih S-C, Chu C-H, Tjung J-J (2012) Discharge planning. Int J Gerontol 6(4):237–240. https://doi.org/10.1016/j.ijge.2012.05.001
Daghistani T, Elshawi R, Sakr S, Ahmed A, Al-Thwayee A, Al-Mallah M (2019) Predictors of in-hospital length of stay among cardiac patients: a machine learning approach. Int J Cardiol. https://doi.org/10.1016/j.ijcard.2019.01.046
Maharlou H, Kalhori S, Shahbazi S, Ravangard R (2018) Predicting length of stay in intensive care units after cardiac surgery: comparison of artificial neural networks and adaptive neuro-fuzzy system. Healthc Inform Res 24(2):109–117
Bacchi S, Tan Y, Oakden-Rayner L, Jannes J, Kleinig T, Koblar S (2022) Machine learning in the prediction of medical inpatient length of stay. Intern Med J 52(2):176–185. https://doi.org/10.1111/imj.14962
Seneviratne MG, Shah NH, Chu L (2020) Bridging the implementation gap of machine learning in healthcare. BMJ Innov 6(2):45–47. https://doi.org/10.1136/bm**nov-2019-000359
Kovoor JG, Bacchi S, Gupta AK, O’Callaghan PG, Abou-Hamden A, Maddern GJ (2023) Artificial intelligence clinical trials and critical appraisal: a necessity. ANZ J Surg. https://doi.org/10.1111/ans.18263
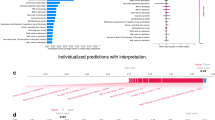
Bacchi S, Gluck S, Tan Y, Chim I, Cheng J, Gilbert T, Menon DK, Jannes J, Kleinig T, Koblar S (2020) Prediction of general medical admission length of stay with natural language processing and deep learning: a pilot study. Intern Emerg Med. https://doi.org/10.1007/s11739-019-02265-3
Bacchi S, Gluck S, Tan Y, Chim I, Cheng J, Gilbert T, Jannes J, Kleinig T, Koblar S (2021) Mixed-data deep learning in repeated predictions of general medicine length of stay: a derivation study. Intern Emerg Med 16(6):1613–1617. https://doi.org/10.1007/s11739-021-02697-w
Bacchi S, Gilbert T, Gluck S, Cheng J, Tan Y, Chim I, Jannes J, Kleinig T, Koblar S (2021) Daily estimates of individual discharge likelihood with deep learning natural language processing in general medicine: a prospective and external validation study. Intern Emerg Med. https://doi.org/10.1007/s11739-021-02816-7
Lam L, Lam A, Bacchi S, Abou-Hamden A (2022) Neurosurgery inpatient outcome prediction for discharge planning with deep learning and transfer learning. Br J Neurosurg. https://doi.org/10.1080/02688697.2022.2151565
Kovoor JG, Bacchi S, Gupta AK, Stretton B, Nann SD, Aujayeb N, Lu A, Nathin K, Lam L, Jiang M, Lee S, To MS, Ovenden CD, Hewitt JN, Goh R, Gluck S, Reid JL, Khurana S, Dobbins C, Hewett PJ, Padbury RT, Malycha J, Trochsler MI, Hugh TJ, Maddern GJ (2023) Surgery’s rosetta stone: natural language processing to predict discharge and readmission after general surgery. Surgery 174(6):1309–1314. https://doi.org/10.1016/j.surg.2023.08.021
Abadi M, Barham P, Chen J, Chen Z, Davis A, Dean J, Devin M, Ghemawat S, Irving G, Isard M, Kudlur M, Levenberg J, Monga R, Moore S, Murray D, Steiner B, Tucker P, Vasudevan V, Warden P, Wicke M, Yu Y, Zheng X (2016) TensorFlow: a system for large-scale machine learning. Proceedings of the 12th USENIX symposium on operating systems design and implementation (OSDI ’16)
Varnava A, Sedgwick J, Deaner A, Ranjadayalan K, Timmis A (2002) Restricted weekend service inappropriately delays discharge after acute myocardial infarction. Heart 87(3):216–219
Rix E (2022) Fixing weekend discharge key to improving capacity at South Australia's hospitals. Australian Broadcasting Corporation. https://www.abc.net.au/news/2022-08-13/why-monday-is-the-worst-day-for-south-australian-hospitals/101330274.
SA Health (2023) Non-Medicare and Long Stay Nursing Home Patient Fees. Government of South Australia. https://www.sahealth.sa.gov.au/wps/wcm/connect/public+content/sa+health+internet/services/hospitals/going+to+hospital+what+to+know+and+expect/non-medicare+and+long+stay+nursing+home+patient+fees.
Marshall A, Vasilakis C, El-Darzi E (2005) Length of stay-based patient flow models: recent developments and future directions. Health Care Manag Sci 8(3):213–220
Harrison GW, Escobar GJ (2010) Length of stay and imminent discharge probability distributions from multistage models: variation by diagnosis, severity of illness, and hospital. Health Care Manag Sci 13(3):268–279. https://doi.org/10.1007/s10729-010-9128-5
Litvak E, Bisognano M (2011) More patients, less payment: increasing hospital efficiency in the aftermath of health reform. Health Aff 30(1):76–80
Casagranda I, Costantino G, Falavigna G, Furlan R, Ippoliti R (2016) Artificial Neural Networks and risk stratification models in emergency departments: the policy maker’s perspective. Health Policy 120(1):111–119. https://doi.org/10.1016/j.healthpol.2015.12.003
Ippoliti R, Falavigna G, Zanelli C, Bellini R, Numico G (2021) Neural networks and hospital length of stay: an application to support healthcare management with national benchmarks and thresholds. Cost Eff Resour Alloc 19(1):67. https://doi.org/10.1186/s12962-021-00322-3
Brady AP, Allen B, Chong J, Kotter E, Kottler N, Mongan J, Oakden-Rayner L, Dos Santos DP, Tang A, Wald C, Slavotinek J (2024) Develo**, purchasing, implementing and monitoring AI tools in radiology: practical considerations. A multi-society statement from the ACR, CAR, ESR RANZCR & RSNA. Insights Imaging 15(1):16. https://doi.org/10.1186/s13244-023-01541-3
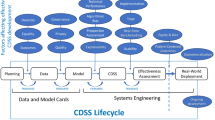
Stretton B, Kovoor JG, Hains L, Kleinig O, Tan S, Gupta AK, Ittimani M, Dwyer A, McNeil K, Chan W, Cusack M, O’Callaghan PG, Maddison J, Bacchi S (2024) How will the artificial intelligence algorithm work within the constraints of this healthcare system? Intern Med J 54(1):190–191. https://doi.org/10.1111/imj.16308
Stretton B, Kovoor J, Gupta A, Hains L, Bacchi S, Wong B, O’Callaghan PG, Barreto S, Hugh TJ, Murphy E, Trochsler M, Padbury R, Boyd M, Maddern G (2023) Get out what you put in: optimising electronic medical record data. ANZ J Surg 93(9):2056–2058. https://doi.org/10.1111/ans.18559
Kleinig O, To MS, Ovenden CD, Kovoor JG, Goh R, Lam L, Wenzel T, Tan Y, Harish H, Gupta AK, Gluck S, Gilbert T, Bacchi S (2024) Vital sign measurements demonstrate terminal digit bias and boundary effects. Emerg Med Australas. https://doi.org/10.1111/1742-6723.14395
Kovoor JG, Bacchi S, Gupta AK, Stretton B, Malycha J, Reddi BA, Liew D, O’Callaghan PG, Beltrame JF, Zannettino AC, Jones KL, Horowitz M, Dobbins C, Hewett PJ, Trochsler MI, Maddern GJ (2023) The adelaide score: an artificial intelligence measure of readiness for discharge after general surgery. ANZ J Surg. https://doi.org/10.1111/ans.18546
Ratnapalan S, Lang D (2020) Health care organizations as complex adaptive systems. Health Care Manag (Frederick) 39(1):18–23. https://doi.org/10.1097/HCM.0000000000000284
Funding
S.B. is supported by a Fulbright Scholarship. P.J.P. receives a L3 Future Leader Fellowship from the National Heart Foundation of Australia (FLF106656).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
P.J.P. has received consulting fees from Amgen, Ely Lilly and Esperion and speaker honoraria from Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Merck Schering-Plough, Novartis, Novo Nordisk, Pfizer and Sanofi.
Statement of human and animal rights
Ethics approval was granted for this project by the Central Adelaide Local Health Network Human Research Ethics Committee (reference number 18686).
Informed consent
For this study, a waiver of consent was granted, and consent was not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Stretton, B., Booth, A.E.C., Satheakeerthy, S. et al. Translational artificial intelligence-led optimization and realization of estimated discharge with a supportive weekend interprofessional flow team (TAILORED-SWIFT). Intern Emerg Med (2024). https://doi.org/10.1007/s11739-024-03689-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11739-024-03689-2